19 Determination of Working Length
Precise determination of working length is of critical importance for a successful endodontic outcome. Without knowledge of the exact working length, no root canal should be instrumented and/or filled. Nevertheless, determination of working length can present considerable problems for the clinician. The problems may derive from the definition of working length itself, and may also relate to the broad variation in root canal anatomy. In this regard it is important to consider all of the methods for determining working length (e.g., radiographic, electronic, and tactile determination), which can be applied either singly or combined. Problems and special situations must be recognized and effectively dealt with to ensure that the working length determination is precise for each root canal of each tooth undergoing endodontic treatment.
The endodontic working length is defined as the distance between a fixed coronal reference point (e.g., a cusp tip) and an apical reference point (the apical constriction). The dentist can arbitrarily determine the coronal reference point, but it must be clearly defined and reproducible (by another clinician and by the same clinician at a subsequent sitting). Clinical experience has shown that the best coronal reference point is a cusp tip. The defined reference point for each individual root canal must be recorded in the patient’s chart.
The working length is marked on an endodontic file/instrument using a silicone rubber stopper. The apical reference point must also be defined, as described in detail below. Although the exact position of the apical end reference point is still controversial, it appears to be advantageous in virtually all cases to end root canal instrumentation in the area of the apical constriction and not to exceed this point (Tronstad, 1991).
The instrumentation and obturation of root canals should end at the apical constriction (physiologic foramen) for the following reasons:
• no apical injury;
• no injury to the periodontal ligament;
• maintenance of accessory lateral canals;
• no extrusion of root canal filling material;
• no apical transport of infected pulpal tissues;
• adequate compaction of the root canal filling against the canal walls;
• no infected tissue remnants within the canal.
The determination of working length should also take into consideration the condition of the pulp in each individual case. In the case of a vital tooth, the clinician’s primary concern is to keep the apical wound as small as possible, while with a necrotic pulp the main concern is removal of all bacteria. Both of these objectives can be met by terminating the apical extent of root canal instrumentation in the region of the apical constriction. Considering that the apical constriction in many cases is a line and not a point, one can argue whether root canal filling in cases of pulpal necrosis should extend closer to the anatomic apex while with vital teeth it should end at the apical constriction.
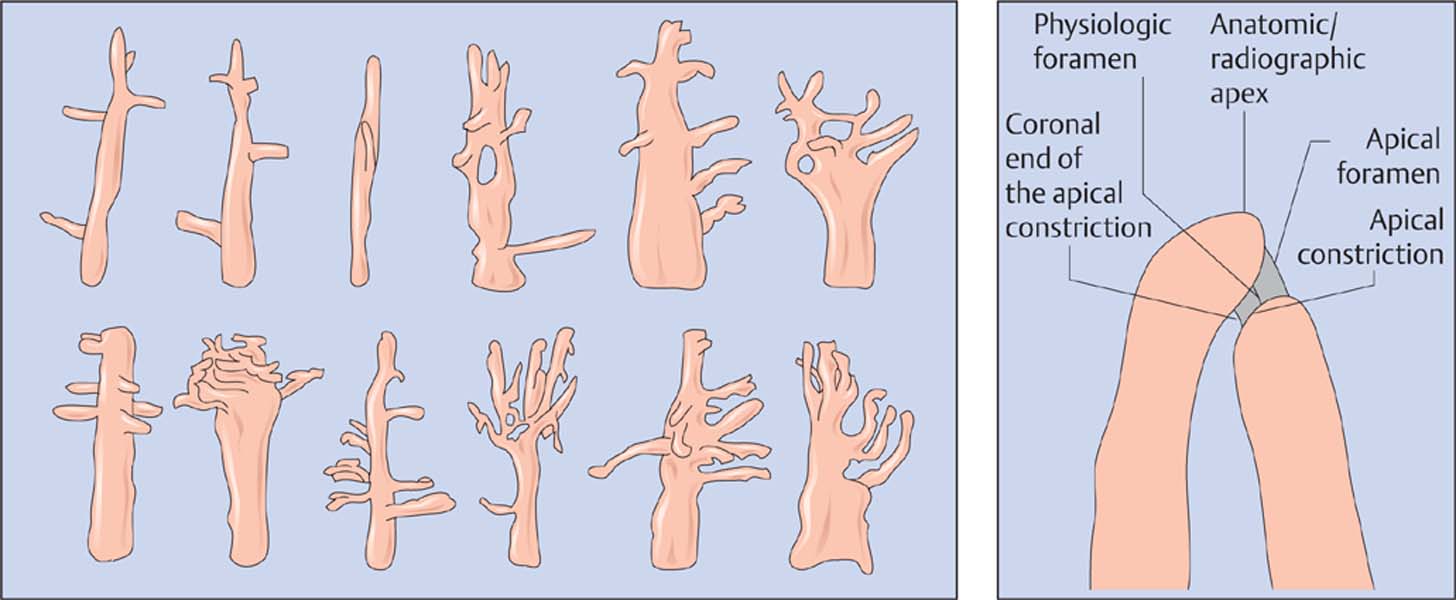
While the coronal reference point can be determined arbitrarily, the position of the apical constriction must be determined using a measurement device. Because of the enormous anatomic variations in the region of the root tip (Hess, 1917; Meyer, 1961), this determination presents a considerable challenge to the clinician and his or her method(s) of measurement. Various studies have demonstrated that the average distance between the apical constriction and the anatomic apex is 1 mm. However, this value varies with a range of 0–4 mm (Kuttler, 1955; Green, 1956; Dummer et al., 1984). For these reasons, the use of “average values” for the determination of the apical endpoint for instrumentation is clinically unacceptable.
Clinical Methods for Working Length Determination
The following methods can be used for determination of the position of the apical constriction:
• radiographic measurement;
• electronic method;
• tactile length determination.
Radiographic measurement
This technique has also been referred to as an “instrument contrast radiograph” and is the most widely used method for the determination of working length. If the film packet is positioned for the parallel radiographic technique, held in a film holder, the anatomic apex of the tooth can be determined and directly observed (in this case it is congruent with the radiographic apex). On average, the distance from the anatomic apex to the apical constriction is 1 mm. For this reason, the radiograpically determined working length should be 1 mm shorter than the distance between the coronal reference point and the anatomic apex. However, because of the range of anatomic variation described above, even this measurement determination may be somewhat less than precise.
Numerous research studies on extracted teeth have demonstrated that the apical constriction resides between 0 and 4 mm from the apex (Kuttler, 1955; Dummer et al., 1984). This could lead to over-instrumentation or under-instrumentation in cases in which the clinical apical endpoint is established (e.g., radiographically) 1 mm from the anatomic apex.
With these facts in mind, it becomes clear that radiographic determination of working length is not an exact science but rather a potentially arbitrary method. On the other hand, radiographic determination provides many additional details and information (canal curvatures, accessory canals, obliterated canals, obstructions), which the other two methods for working length determination cannot provide.
Even when using eccentric radiographic projections, there still may be uncertainty about the arrangement of the individual canals lingually or buccally in the case of root canals that overlap in a radiographic projection (mesial root canals of mandibular and maxillary molars and maxillary premolars). For this reason, during the preparation of radiographic images, only one root canal system should be instrumented at a time or different types of instrument types should be used in the various canals (K files, Hedström files). It is also prudent to always use the same instrument in the same canal (e.g., buccal). This will simplify examination and evaluation of the radiographs even at a later date.
19.1 Root canal anatomy
Structural anatomy of root canals: there are numerous patterns of ramification and the position of the apical constriction is variable.
Right: Schematic depiction of the root tip. A linearly shaped constriction will terminate apical to the physiologic foramen.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses