Chapter 18
Treatment planning
What is the overall treatment objective?
The key to developing any treatment plan is to have a clear objective. The terms tooth-driven implant placement and prosthodontically driven implant placement have been coined to emphasize this fundamental principle. Simply placing implants in any available bone without considering the restorative requirements risks restorations that have aesthetic and functional compromise, are difficult or impossible to keep clean, are prone to failure, or, at worst, are unrestorable and need to be removed.
This chapter discusses the key questions that need to be addressed during the planning process (< ?xml:namespace prefix = "mbp" />
Table 18.1 Questions that need to be addressed for planning dental implants
Is the final restoration to be fixed or removable by the patient?
Most patients have a desire for fixed restorations, and when small numbers of teeth are missing, this is usually feasible. However, for edentulous patients or when there is a large alveolar deficiency, detailed assessment may show that implant overdentures are the restoration of choice or may be the only realistic option.
What are the diagnoses and constraints for treatment and maintenance?
What are the aesthetic goals?
Which teeth are to be replaced in part-dentate patients?
If teeth have migrated or erupted into abnormal positions, or where there is marked dentoalveolar disproportion, the number and form of missing teeth to be replaced are not always clear-cut. This is quite often the case when teeth are missing for developmental reasons. Extractions or orthodontic tooth movements may be required to allow appropriate numbers and sizes of tooth replacements (
What is the ideal form and position of the individual teeth to be replaced?
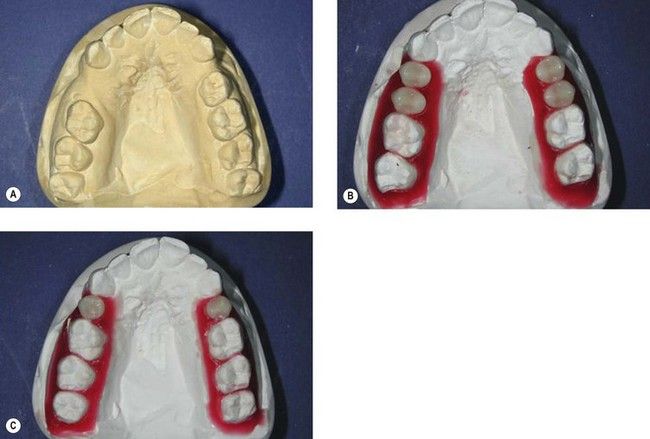
The precise external form of a proposed tooth replacement has a major influence not only on the appearance of the final restoration but also on numbers of implants and their positioning. The space occupied by the proposed replacement, whether teeth or alveolus, is referred to as the prosthetic envelope. Several methods can be used to help establish this aspect of the proposed restoration from both the aesthetic and the occlusal standpoint (
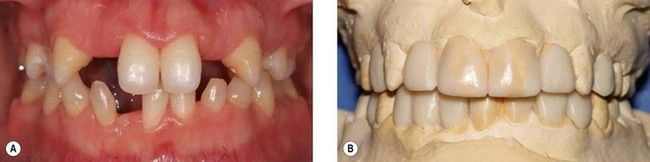
Fig 18.3 A wax-up of the proposed restorations has been made for a patient who has completed orthodontic treatment to realign teeth in preparation for dental implants. The wax-up helps to analyse the prosthetic envelope of the proposed restorations, which in turn directs the three-dimensional positions of dental implants.
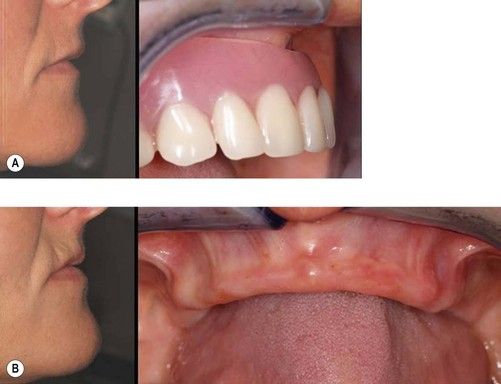
What is the ideal soft tissue frame of the teeth to be replaced?
The frame of gingiva around teeth is as important as the teeth in producing satisfactory aesthetics. Trial dentures and wax-based trial prostheses can help both dentist and patient visualize possibilities and limitations for the soft tissue frame around possible implant restorations (
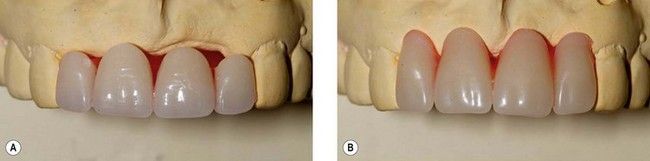
Fig 18.4 The trial tooth set up with well-proportioned teeth (A) shows that there is a significant alveolar deficit. If the deficit were to be replaced with teeth alone, they would have the appearance of gingival recession (B). If the compromise is unacceptable, this investigation reveals the need for exploring possibilities for replacement of alveolar tissue in the form of tissue grafts or by prosthetic means.
Does acceptable lip and facial support rely largely on the presence of a removable prosthesis?
Following tooth loss, it is usual for resorption in the maxilla to result in loss of buccal and vertical alveolar volume. Appropriately positioned maxillary artificial teeth come to lie in a buccal location relative to the resorbed alveolus (
What are the occlusal objectives?
Is there space within an existing tooth-borne occlusal scheme to accommodate the proposed arrangement of teeth to be replaced?
Even a small amount of mandibular incisor anterior migration after maxillary tooth loss can create difficulties (
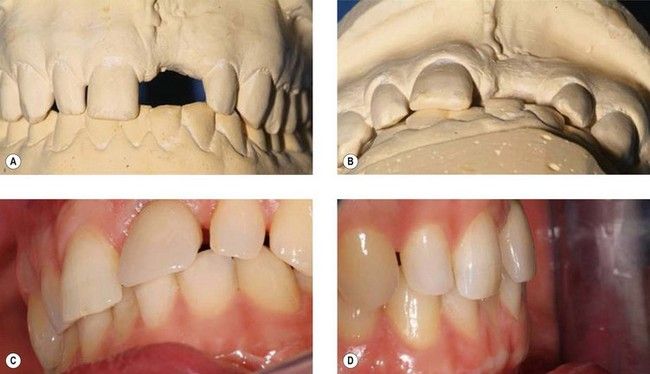
Fig 18.6 Failure to appreciate the prosthetic requirements for an implant restoration at the maxillary left central incisor. Although from the anterior view (A) there appears to be sufficient space, the occlusal view (B) shows that the mandibular incisors encroach on the required prosthetic envelope. It was not possible to simply adjust the mandibular incisors enough to create space, and the final restoration is significantly compromised (C and D). The patient declined orthodontic treatment to realign the mandibular teeth.
In addition to considering space for the external contours of the tooth replacement, it is necessary to decide whether there is sufficient internal volume to accommodate whatever method is chosen to attach the restoration to the implant (
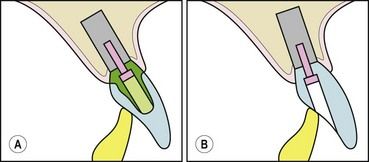
Fig 18.7 Examples of space requirements for implant-restoration attachment mechanisms for a maxillary incisor. (A) A cemented restoration requires sufficient volume to accommodate an abutment with adequate resistance and retention to be screwed into the implant. (B) A crown screwed directly into the implant without an intervening abutment may require less interocclusal volume than the cemented alternative. The position of the implant in panel A would make it difficult to provide the style of restoration shown in panel B because masking a visible screw access hole would be problematic.
Is the proposed restoration protected in excursions?
In addition to being accommodated in the static occlusion, the proposed restoration must integrate into the dynamic occlusion. Implant restorations can be designed to carry excursive contacts, share excursive contacts with natural teeth, or, if possible, to be clear of excursive contacts altogether. Philosophies for implant occlusion are drawn from conventional dental occlusal paradigms with the added precautionary principles, where possible, of axial loading of implants; excursions on teeth rather than implants; and sharing occlusal loads between implants, particularly in posterior areas of the mouth, where loads are higher.
In addition to clinical observation, trial dentures and wax-ups enable occlusal features to be identified and modifications in occlusion to be investigated.
It may be judged necessary to change occlusal relationships to achieve the occlusal goals, for example, by recontouring of teeth, orthodontic movement, or reorganization of an existing occlusal scheme.
Is there space within the prosthetic envelope of a denture to accommodate overdenture attachments?
The size, shape, and position of the denture will be dictated largely by the anatomy of the patient. Clearly, the denture needs to be large enough in cross section to accommodate overdenture attachments.
What are the requirements to facilitate access for oral hygiene?
In order to reduce the risk of peri-implant inflammation, restorations must be designed to allow easy access for cleaning by the patient. Fixed restorations for the edentate maxilla in particular may not easily meet these objectives (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses