Prognosis and Results After Periodontal Therapy
Overall Prognosis
The overall prognosis is the expected outcome for the patient. It is determined on the basis of the specific risk factors that the individual patient presents. For example, a patient with a systemic disease such as type 1 or type 2 diabetes that overlays chronic periodontitis is likely to have a less positive treatment outcome than another patient with the same oral conditions but no systemic disease. Healing and resolution of periodontal disease will be altered for individuals with systemic diseases and conditions because these patients respond differently to bacterial infection. Many factors discussed in Chapters 6, 7, and 9 will alter patient responses and therefore will complicate the overall prognosis. Individuals with systemic diseases and conditions are less likely to follow the course of healing that one would expect—regeneration and repair of periodontal tissues over the days and weeks after treatment.
All information available from the subjective and objective assessment of each patient is applied to formulate the overall prognosis. This prognosis is also sometimes referred to as a global prognosis. Once the overall prognosis is analyzed and determined, an individual tooth prognosis is determined for each tooth.1 These categories are somewhat arbitrary because some patients may only have a few teeth, so the prognosis for those individual teeth and the global prognosis may be the same.
To determine the overall case prognosis, the following questions need to be addressed2:
• Should treatment be undertaken?
• Is treatment likely to succeed (retain the teeth and provide good function)?
• If prosthetic replacements will be made, can the periodontally treated teeth support the burden?
The factors considered in making an overall prognosis for patients with periodontal disease include age, systemic health, smoking, type of periodontal disease, oral conditions (including inflammation and bone levels), and the attitude and perceptions of the patient. Many clinicians consider the attitude, perceptions, and cooperation of the patient the most critical factors in the lasting success of periodontal treatment. Prognosis is far from an exact science and research to develop better methods for assigning prognosis based on objective clinical criteria is ongoing.3
Age is a significant consideration. Epidemiologic studies (see Chapter 3) show that older patients demonstrate greater periodontal destruction as they age. However, concern arises when younger patients have significant periodontal destruction. In fact, younger individuals are less likely than older individuals with similar amounts of periodontal disease to respond well to treatment because some genetic or unidentified systemic factor is contributing to the advancement of the disease at an early age. Older individuals would have been more resistant and taken years longer to lose the same amount of attachment and support for the teeth. The prognosis for the older person in this case would be better than for the younger person with similar periodontal destruction because of a greater ability to control the disease process in the older person.
Systemic diseases and conditions influence the host’s ability to respond to periodontal diseases. These diseases include diabetes, neutrophil defects, and factors associated with immunosuppression such as human immunodeficiency virus (HIV) infection or organ transplantation. Chapter 9 provides an extensive description of systemic diseases that affect periodontal disease and treatment.
Smoking has a direct relationship to the prevalence and incidence of periodontal disease. Smoking affects not only the severity of disease but also the healing potential of the oral tissues. Patients who smoke do not respond as well to periodontal therapy as those who do not.2,4 Other forms of tobacco, such as cigar smoking and spit tobacco use, probably have the same effect on prognosis, although most research thus far has centered on cigarette smoking.
Oral conditions are an obvious consideration. Heavy deposits of plaque biofilm and calculus and severity of inflammation must be factored into the analysis. Clinical attachment loss indicates how much support for the tooth has been lost. This bone loss is significant because the prognosis is adversely affected as the attachment level gets closer to the root apex. Also, teeth weakened by extensive bone and attachment loss may not be serviceable for certain restorative procedures, such as abutment teeth for fixed partial dentures or removable partial dentures. Overall or global prognosis is defined by categories described in Table 18-1.1,2
TABLE 18-1
Global Prognosis Categories and Definitions1
| PROGNOSIS | CONDITIONS |
| Excellent | No bone loss, excellent gingival condition, no systemic considerations, good patient cooperation |
| Good | Adequate remaining periodontal support and ease of maintenance, adequate patient cooperation |
| Fair | Attachment loss and furcation involvement (Class I), patient cooperation likely, systemic factors controlled |
| Poor | Attachment loss and furcation involvement that can only be maintained with difficulty (Class II or III), tooth mobility, presence of systemic factors |
| Questionable | Poor crown-to-root ratio, poor root form, root proximity, Class II or III furcations, mobility, presence of systemic factors |
| Hopeless | Advanced bone loss, inadequate attachment, uncontrolled environmental/systemic factors, tooth should be extracted |
Individual Tooth Prognosis
Pocket depths, particularly persistent deep pockets, can harbor pathogenic plaque biofilms and are associated with increased inflammation. The extent that deep pockets exist in the mouth, or remain after Phase I therapy, can adversely affect the prognosis for the tooth. There is also some evidence that persistent deep pockets are an important risk indicator for future periodontal disease destruction not limited to the original site.1 Deep pockets also generally reflect loss of attachment to the tooth, a further indication that the tooth is weakened and an indicator of a less favorable prognosis. Bleeding is also associated with deep pockets and persistent inflammation. The relationship of persistent bleeding to the progression of periodontal disease is presented in Box 18-1.
Mobility is associated with less favorable periodontal outcomes but is not confirmed as a risk factor. It is caused by inflammation in the periodontal ligament and bone loss. Mobility can result from loss of support for the tooth (bone and clinical attachment loss) or trauma from occlusion. If the mobility can be corrected by altering occlusal forces (see Chapter 11), then it has no detrimental effect on prognosis. However, if the mobility is the direct result of loss of support for the tooth, then the prognosis is less favorable.1
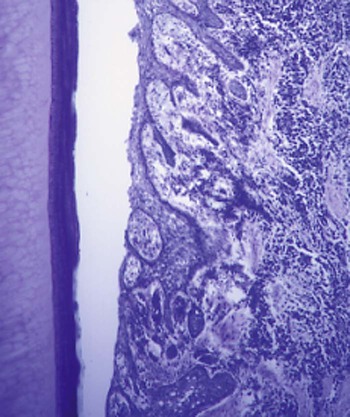
Tooth morphologic features can alter the prognosis for specific teeth. Findings such as lingual grooves and cervical projections of enamel lead to isolated pocketing and can permit severe periodontal infections. These are not uncommon findings. Cervical enamel projections are estimated to occur in about 25% of mandibular molars and in 20% of maxillary molars. Some are very small and therefore insignificant; others can extend several millimeters and lead directly into furcation areas (remember there is no soft tissue attachment to enamel surfaces). Lingual grooves are found on about 6% of maxillary lateral incisors and 3% of maxillary central incisors.2 An example of a long lingual groov/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses