Ophthalmic Consequences of Maxillofacial Injuries
Perforating Injuries of the Orbit
Both prospective and retrospective studies of patients who have sustained midfacial fractures indicate that as many as 40% may sustain serious ocular injury that warrants ophthalmologic referral.1–8 A recent study9 has demonstrated that up to 91% of patients with orbital fractures who had an ophthalmic evaluation within 1 week of their injury sustained some form of ocular injury. Many of these were classified as mild but 45% were deemed to be moderate or severe injuries.
Ophthalmic Assessment
History
The following data are recorded:
1. The time, place, and circumstances of the injury
2. The exact nature of the injury
3. The nature of the object that caused the injury (e.g., a kick is more likely to damage the eye than a head butt)
4. The velocity and vector of the traumatic force
5. Whether glasses were worn (the glasses may have protected the eye or may have given rise to a glass foreign body entering the eye)
Clinical Examination
Assessment of Visual Function
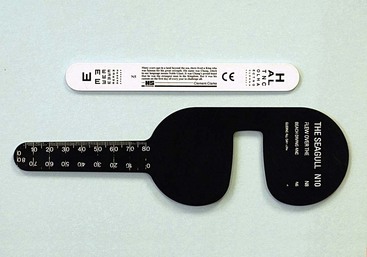
For convenience, the clinician can carry a means of assessing visual acuity for near vision in her or his pocket. For older patients, near acuity must be determined with the use of reading glasses or a pinhole (Fig. 18-1) because the eye’s ability to accommodate declines with age. If a formal means of visual acuity assessment is not available, the clinician can estimate visual acuity using a newspaper or paper currency.
Visual Fields
Examination for Structural Disorders
Ophthalmoscopy Through Dilated Pupils
The contraindications to pupillary dilation are as follows:
1. An iris-supported intraocular lens, which could be dislodged if the pupil were dilated
2. A history of intermittent blurring of vision and pain in the eye, suggestive of angle-closure glaucoma
The reader will no doubt be conversant with the normal appearance of the retina (Fig. 18-2) and the use of the direct ophthalmoscope. The following hints may, however, be of value:

FIGURE 18-2 The normal optic disc and retina.
1. The examiner looks through the ophthalmoscope from a 0.33-m (1-foot) distance, examining the red reflex initially. By this means, the examiner can identify any opacities in the media—for example, vitreous hemorrhage or traumatic cataract.
2. The patient is asked to fixate into the distance with the other eye. If the patient focuses for near vision, the examiner will have difficulty in focusing the ophthalmoscope.
3. If a bright light reflex gets in the way, the light is reflecting from the cornea. If the ophthalmoscope is rotated very slightly, the light reflex will diminish or disappear, because it will no longer be reflected back along the examiner’s visual pathway.
4. To observe a scene through a keyhole, the eye needs to be placed close to the keyhole. The same principle applies to ophthalmoscopy—the closer to the patient’s eye is the examiner, the wider the angle of view.
5. To examine the fovea, the patient is asked to look at the light.
6. To examine the peripheral retina, the patient is asked to move her or his eyes in sequence in different directions. When the patient looks up, the examiner is looking at the upper retina as it is brought down into view; the same principle applies to the other positions of gaze.
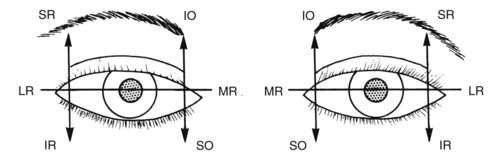
Examination of Eye Movements
Eye movements are commonly impaired following facial and head injury. It must be remembered, however, that an antecedent squint is not uncommon. Moreover, ptosis, blurred vision as a result of the eye injury, amblyopia, and a history of patching of the eye in childhood all may prevent the patient from experiencing double vision. Eye movements are therefore objectively assessed in all patients who have sustained an injury likely to be complicated by a motility disorder (e.g., a blowout fracture). Figure 18-3 indicates the primary directions of action of each of the extraocular muscles. The eye movements into each of these positions of gaze are examined.
The examiner sits directly opposite the patient and uses a penlight to examine the eye movements. The penlight is moved in a manner similar to that for peripheral visual field testing. The light is held at approximately 0.33 m (1-foot) from the patient. The examiner observes the exact position of the light reflexes on the cornea with respect to the pupil. The patient is asked to follow the light. The light is moved in an arc into each position of gaze, with the light constantly directed at the eyes. The symmetry of the light reflexes and symmetry of the positions of gaze are closely examined (see Fig. 18-3). The skilled observer is able to detect most motility disorders.
Minor Eye Injuries
Subconjunctival Hemorrhage and Bruised Eyelids
Subconjunctival hemorrhage (Fig. 18-4) with bruised eyelids commonly follows midfacial injury. Blood may track forward from an orbital injury, or bleeding may take place locally. A clear demarcation line to the bruising of the eyelid suggests orbital hemorrhage. Such bruising is usually benign, but it may be related to severe ocular injury. Careful examination of the eye is required in every case.

FIGURE 18-4 Subconjuctival hemorrhage.
Corneal Abrasion or Corneal Foreign Body
Treatment
After the administration of one drop of topical local anesthetic, which allows clinical examination and gives temporary pain relief, a medium-acting cycloplegic agent such as cyclopentolate (24 hours), which alleviates pain caused by ciliary spasm, and a topical antibiotic such as chloramphenicol are instilled. If a foreign body is present, it is removed. A corneal foreign body is removed with great care, preferably using binocular magnification. The physician can usually lift off a foreign body on the surface of the cornea by using a hypodermic needle held tangentially to the corneal surface, ensuring throughout the procedure that the patient is unable to move forward toward the needle. One drop of a topical nonsteroidal anti-inflammatory preparation is then instilled to alleviate pain.10
Nonperforating Eye Injuries
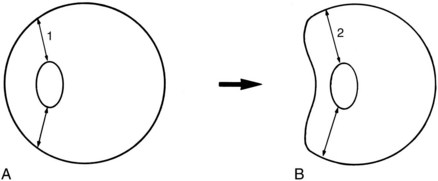
A high-speed anteroposterior force results in marked distortion of the globe (Fig. 18-5). The eye is transiently deformed, with notable distention in the coronal plane and shortening of the anteroposterior dimension. The sclera is inelastic and the aqueous and vitreous cannot be compressed. The iris, ciliary body, zonule of the lens, and peripheral retina may be torn from their insertions and, in severe cases, the sclera may rupture. Distortion of the posterior segment of the eye can result in a tear of the choroid associated with subretinal hemorrhage and, in the most severe case, avulsion of the optic nerve from the globe.
In this section, the results of injury to each component of the eye are discussed separately. However, almost any combination of injuries can occur, which can occasionally result in disorganization of the structures of the globe (Fig. 18-6).
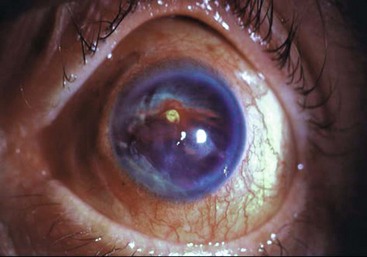
FIGURE 18-6 Disorganized anterior segment. The normal structures within the anterior chamber are not recognizable.
Conjunctiva and Cornea
Loss of the corneal epithelium (Fig. 18-7) is fairly common and causes the same signs and symptoms as a corneal erosion. The corneal endothelium is comprised of a monolayer of cells that probably do not replicate following injury. Their function is to maintain the clarity of the cornea by pumping water out of the cornea and into the anterior chamber. Damage to the corneal endothelium results from a combination of contusion, reactive inflammation, and raised intraocular pressure.11 This condition may culminate in permanent edema if the endothelial cell population is reduced below a critical level. Recovery of corneal clarity can take place in some patients after a number of/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses