The Motivationally or Financially Impaired Patient
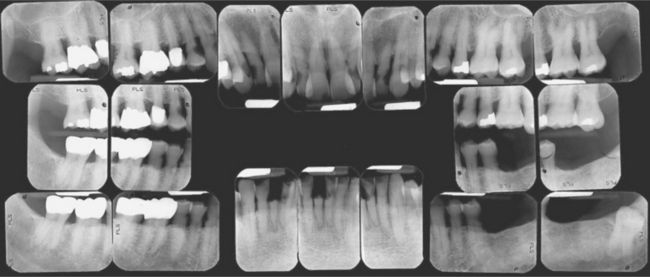
Many patients are fatalistic about their teeth. They have serious doubts as to whether their teeth can or should be saved. They see the challenge of trying to rehabilitate their mouths as insurmountable and believe they do not have the time, energy, ability, or money to accomplish the task. These are all perceptions; sometimes they are realistic, and sometimes they are not. In many cases, significant improvements in oral health can be accomplished that are within the patient’s financial means and capacity to handle treatment (Figure 17-1). For the treatment to be successful, however, the patient must become willing to accept responsibility for his or her own oral condition. Unfortunately, some patients are unwilling or unable to accept that responsibility at least initially. Herein lies one of the greatest challenges to the practicing dentist learning to discern how a new patient will respond to this challenge. Indeed, although some patients accept responsibility easily, some will do so only after much education and encouragement, and others never will.
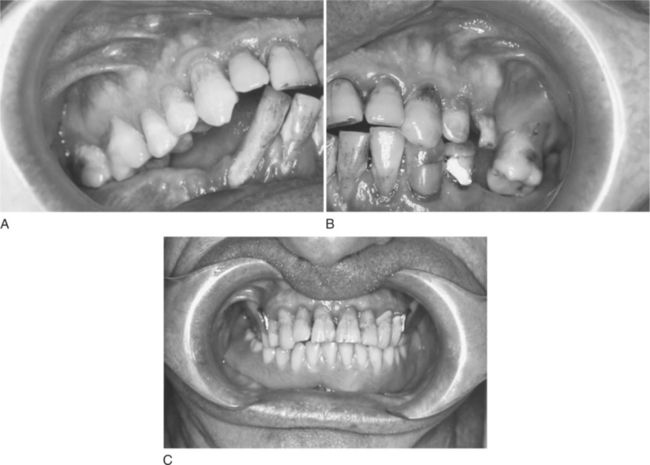
Figure 17-1 Motivationally and financially compromised patient before and after treatment. (Courtesy Dr. D. R. McArthur, Chapel Hill, NC.)
COMMON CLINICAL SCENARIOS
Several commonly encountered situations illustrate the kinds of beliefs and opinions that a motivationally impaired patient may hold. Each is an intellectual construct that can be expected to contain some truth and some fantasy. Listening carefully, the dentist will attempt to glean the real factors contributing to the patient’s oral disease, being careful to avoid the temptation to immediately dispel myths and misunderstandings on the spot. Because a considerable amount of thought and energy will have been invested in the construct, the patient may resent the intrusiveness of a health care professional who quickly dismisses it out of hand. The careful listener allows the patient sufficient latitude to characterize his or her perceptions concerning oral disease. As rapport and trust build in the relationship, the dentist will find opportunities to add to the patient’s knowledge base. Providing the patient with information to change and improve his or her own beliefs is a more effective strategy than trying to substitute entirely new ones. The latter approach often does not work at all, or if it does, acceptance is more often incomplete or short-lived, failing for two critical reasons. First, such a wholesale substitution invalidates the patient’s own thought processes, and secondly, it ignores the essential psychological and emotional investment that the construct holds for the patient. Several beliefs commonly held by such patients are discussed in the following sections.
Soft Teeth
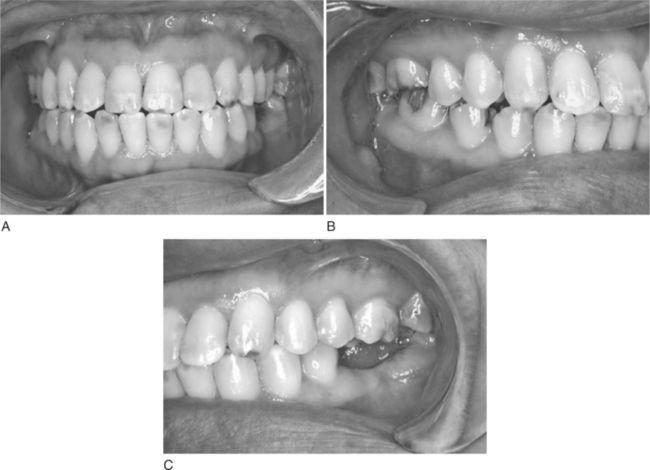
Patients who believe their teeth are “soft” typically report numerous visits to the dentist beginning in the early teens, and a long succession of teeth restored and restored again because of new and recurrent caries. By the time this patient reaches middle adulthood, some teeth may be missing and others have large restorations (Figure 17-2). Recurrent caries continues to be a problem. Although a dentist may have even told the patient as a child, “You have soft teeth,” the most frequent explanation is a cariogenic diet and poor oral hygiene. The patient may now believe that the teeth can no longer hold fillings and doubt that they are worth saving.
Pregnancy and Breast-feeding
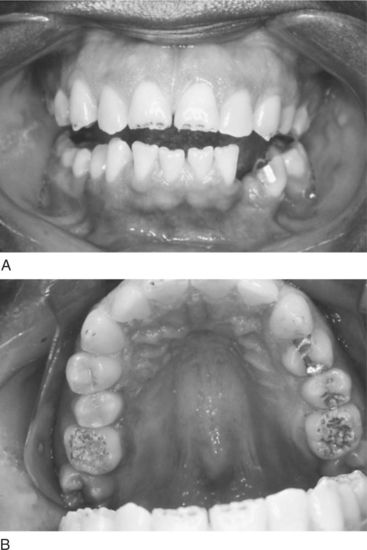
Female patients who have carried and delivered babies and later breast-fed them may relate a history of rampant caries developing during that time. In some cases, the caries may have become less active, but the patient continues to suffer from the ill effects of the earlier decay (Figure 17-3). Large restorations often are present, some teeth may now be fractured, and multiple full-coverage restorations may be necessary. Some of these patients may continue to suffer from rampant caries that they attribute to the earlier period of pregnancy and lactation. The patient may have been reluctant to replace missing teeth out of concern for the perceived poor prognosis or because of a maternal desire to take care of the dental needs of her children first.
Family Dentures
Some patients, often those with extensive restorative needs or those suffering from severe periodontal disease, are certain that dentures are inevitable. Because numerous family members have experienced this fate, they see becoming edentulous as unavoidable. Those who are most fatalistic often observe that they have inherited the condition. The dentist may be hard pressed to convince such patients that they have other alternatives.
A variant of this explanation comes from the patient who refuses the option of replacing missing teeth with a removable partial denture, arguing that the retentive clasps will harm the abutment teeth. The patient often relates stories of friends or family members who wore partial dentures and eventually lost all remaining teeth. It is not surprising that partial dentures may sometimes fail when one considers the often questionable prognosis of some abutment teeth, the added burden of removing plaque around the clasps and other partial denture components, and the continuing risk for caries or periodontal disease. When the patient witnesses such a failure, it only confirms the belief that the family wisdom is correct and the prophecy that he or she also will end up in dentures will be fulfilled (Figure 17-4).
Fear of the Dentist
The management of the anxious or fearful patient is discussed in Chapter 13. Patients who have been unable to come to terms with this problem often avoid dental treatment altogether. Those with untreated active caries suffer from gross tooth destruction, fractures, abscesses, and toothaches. They typically have a checkered history of episodic visits for pain relief. Similarly, patients with untreated, rapidly progressive, or severe periodontal disease become afflicted with pain, abscesses, and tooth loss. Despite the physical discomfort and loss of self-esteem, overcoming fear is a greater obstacle than such a patient can surmount, resulting in grave consequences to teeth, health, and self-image.
Fear of Losing Teeth
It is not at all unusual for the patient who has a severely compromised dental condition to present for an initial visit in pain. Many of these same patients are anxious about receiving dental care and have a history of sporadic, episodic dental treatment. In this scenario, the patient is faced with a pulpally involved tooth that will require extraordinary efforts to save. From a professional perspective, the patient’s time, energy, and financial resources could be spent far more wisely on other teeth that have a more promising restorative prognosis. The dentist recommends extraction, but the patient insists on saving the tooth and initiating the root canal therapy in spite of all arguments to the contrary. At this point, the patient’s judgment is clouded by both the pain experience and the emotional angst caused by the prospect of losing yet another tooth. Having been relieved of pain on this occasion, the patient then fails to return for any additional scheduled visits. The presence of pain and the “fear of losing any more teeth” were sufficient motivation to bring the patient to the office for acute care and initiation of the root canal therapy, but insufficient to sustain continuation with current or comprehensive dental treatment. The challenge for the dentist in this situation is to be able to take a positive motivation (patient’s desire to keep a pulpally involved tooth) and channel it in a responsible and productive way, while at the same time identifying and overcoming underlying fears and concerns.
Limited Financial Resources
Many patients report that they do not have the financial resources to pay for dental treatment. They often suffer from the ill effects of poor oral hygiene and inadequate professional care. They may be afflicted with oral disease of the same magnitude as that seen in the previous scenarios. It is important to recognize that although some purported financial limitations are valid, sometimes they are a reflection of other deeper issues or concerns, such as the fear of dental treatment. In general, patients with financial limitations fall into one of three groups:
Each of these groups presents a unique challenge to the dentist. Management alternatives for each are discussed later in this chapter.
Recognizing that the patient falls into one of the previous six scenarios, or a related situation, helps the dentist discern how the patient has arrived at the present situation and what real or perceived obstacles must be overcome to improve oral health. In many cases, the patient may have used financial or other concerns as both an explanation and an excuse. Over time, the concerns of such patients become barriers that they cannot get past, with the mere presence of the barrier justifying inaction and setting up the expectation of failure. Expecting failure, and afraid to act, the patient’s disease continues and adverse sequelae arise a self-fulfilling prophesy is met. Breaking this cycle represents a significant challenge for both patient and dentist.
IDENTIFYING THE UNDERLYING PROBLEM
The patient history and clinical examination are indispensable, not only in determining the clinical condition, but also in helping reveal how the condition evolved. At the initial visit, the motivationally impaired patient often is apologetic about the condition of his or her mouth. It is not unusual for such a patient to express embarrassment and self-consciousness about gross caries, fractured or missing teeth, periodontally involved teeth, and halitosis. It is imperative that the dentist be nonjudgmental, assuring the patient that his or her oral condition is not unique, and that the dentist and staff will do their best to help correct the problems and eliminate disease. In many cases, it will have taken great courage for the patient simply to come to the appointment. Any comments, stringent office policies regarding payment, or body language by the dentist or staff that the patient interprets as patronizing, demeaning, or unsympathetic can be devastating to the person’s self-esteem. Many motivationally impaired patients are extremely vulnerable at this point and may overreact to the smallest slight. On the positive side, if such patients are treated with respect and dignity and if their concerns are dealt with professionally and sensitively, they can become appreciative, cooperative, and loyal to the practice. As the history is taken and the examination conducted, the patient usually begins to open up and share concerns and perspectives. Box 17-1 includes useful questions to ask that will help to facilitate discussion with the patient.
As this process unfolds, specific causes for the compromised oral health will become apparent. The following are many of the common underlying causes for the patient’s condition. It is noteworthy that there is rarely a single cause for the patient’s lack of motivation to address oral problems. It is not unusual for the motivationally compromised patient to have a history that includes several of the following causes, and many of these patients may be affected by two or more of these factors at any moment in time.
Hereditary and Developmental Factors
Hereditary and developmental factors may include such conditions as hypocalcification, hypoplasia, amelogenesis imperfecta, severe fluorosis, a family predilection for periodontal disease, or a physiologically low pain threshold (Figure 17-5). Identifying such factors can be useful in two important respects: Helping the dentist develop treatment strategies that target the root causes of the patient’s oral disease; and providing positive psychological benefit to the patient who now sees a logical reason for the condition of his or her teeth and may come to find hope that there is a solution.
Metabolic, Endocrine, and Immune Deficiency Factors
Hormonal changes are known factors in the development of pubertal and pregnancy gingivitis (Figure 17-6). Altered immune function can contribute to periodontal disease and other intraoral abnormalities and infections. Identifying these issues and sharing that insight with the patient will have the same potential benefits as noted previously relating to hereditary and developmental factors.
Knowledge and Informational Issues
Some patients are fully capable of understanding the relationship between their behavior and the oral disease, but suffer from a lack of information or, perhaps worse, from misinformation. Sometimes they have correct information, but are reluctant to act on it. As the examination continues, the dentist has an opportunity to gain a sense of the patient’s level of knowledge about oral health and disease. This may not be the best time to try to educate or reeducate the patient, however. Only after a full understanding of all problems has been reached and a conscious decision made regarding the most effective intervention, should the dentist attempt to modify the patient’s knowledge base.
In some instances, intellectually challenged patients may be unable to understand the connection between oral disease and deleterious habits, including poor oral self care. Intellectually, psychologically, or physically challenged patients also may have care providers who are unaware that they are contributing to oral disease by supplying highly cariogenic snacks as rewards or pacifiers in the management of their clients. In such a situation, the care provider must be given correct and appropriate information that can be used to help improve the patient’s oral health.
Interrelationship of Oral Health and Self-Image
A poor self-image often diminishes an individual’s interest in good oral health and reduces tolerance for the cost and discomfort of dental treatment. If the patient is not happy with himself or herself or with life in general, it is unlikely that enthusiasm will be generated for dental care. Such patients are more likely than most to need extensive and complex treatment, reinforcing this negative perception. Some may barely cope with the issues of daily life, and it may be too much for them to deal with the fear and the expense of dental treatment they often consider elective. A rarely vocalized but often perceived sentiment is “My bad teeth are just one more bad thing in my life.” This negative perspective might have redeeming value if some tangible benefit to avoiding dental treatment could be described. Unfortunately, this is almost never the case. Left unattended and untreated, oral disease worsens, the likelihood of pain and infection increases, and with the exception of full denture construction, the costs and complexity of treatment continue to grow. Furthermore, as the oral condition deteriorates, the patient’s appearance becomes less attractive and the self-image suffers even more.
Behavioral and Nutritional Factors
The motivationally impaired patient is also likely to have poor dietary habits, to engage in self-destructive behaviors, and to be less likely to engage in health-promoting practices, such as effective oral self care or regular physical exercise. These issues may have a deeper root cause in economic poverty. But regardless of the cause, they can have a significant negative impact on the patient’s sense of wellness and the actual state of oral, mental, and physical health. Poor nutrition contributes to dental caries and, to a lesser extent, to periodontal disease. Self-destructive habits, such as smoking and excessive alcohol consumption, also contribute to oral disease (see Chapters 11 and 12). Behavioral causes can be the most complex and most difficult to solve; for many patients they can also be the most fundamental and the most important. Such patients can also be a challenge for the dentist to manage (see the Ethics in Dentistry box). In extreme cases, such persons may be clinically depressed and have the expectation that they will not live a normal life span. In this situation, antidepressant therapy may be necessary and integral to any attempts to modify behavior relating to oral health. For more on managing patients with clinical depression see Chapter 14.
Psychological Gain
Some patients may find a psychological benefit in being impaired. They may garner sympathy for their poor oral health from family members, friends, and co-workers, using it to avoid work or other responsibilities. For such patients, a health-related disability may have become part of a defense mechanism, used as a shield to deflect blame or responsibility. Sometimes, it may actually be safer or more comfortable for the patient to believe that the situation is hopeless. In cases in which it seems possible that the patient has a large investment in poor health, the dentist has the challenging but absolutely essential task of determining whether the patient really seeks improved oral health. If so, does he or she want merely a temporary fix, or a genuine solution? How much emotional energy is the patient capable of investing in dental treatment?
Real Versus Perceived Financial Barriers
In the course of early discussions with the patient, the dentist needs to determine, as tactfully as possible, whether the patient has financial limitations and to evaluate whether those limitations are real or perceived. The extent to which those limitations will preclude treatment must be determined. Will disease control treatment be feasible? Should outside financial assistance for the patient be sought? Is the reported financial limitation in actuality an expression of some other underlying barrier to treatment? These questions need to be handled with tact and can only be raised as the patient begins to have trust in the dentist. If financial issues are raised too early or insensitively, the patient may perceive the queries as an intrusion into his or her private life and conclude that the dentist is “after my money.” Such a breach in the dentist-patient relationship may be irreparable.
EVALUATING THE POTENTIAL FOR CHANGE
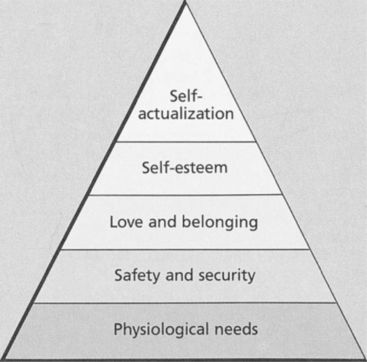
Maslow’s hierarchy is a model frequently used to explain an individual’s value system and priorities at a particular point in life (Figure 17-7). This hierarchy is also an excellent tool to help assess the patient’s potential to be motivated to change his or her dental condition. If, in fact, satisfaction of the person’s needs is restricted to Level 1, Physiological (most basic human needs), then it is unlikely that efforts to convince the patient of the value of a healthy oral condition will be effective. By the same token, the patient who has all of his or her basic needs met and is now motivated by Level 5, Self-Actualization, is more likely to be amenable to a sophisticated intellectual rationale supporting the benefits of optimal oral health. This is not, however, a guarantee that those efforts will be successful because that same patient has complete freedom to accept or reject the rationale and may choose to do so on strictly intellectual grounds. The patient also may choose to reject it because other self-actualizing concepts are more appealing or take precedence. Therefore Maslow’s hierarchy should not be viewed as an infallible tool, but simply as a useful method for attempting to determine whether a patient is likely to be amenable to change, and if so, what strategies are more likely to succeed.
Some factors contributing to the patient’s motivational impairment cannot be altered, most notably those relating to heredity or physical and mental development. Some environmental factors, such as job stress, can be altered, whereas others realistically cannot. Behavioral factors are strongly influenced by the patient’s psychological perspective and sense of self-worth. When psychological barriers to change are not significant and when the patient has a positive sense of self-worth, the potential for eliminating deleterious behaviors and promoting positive ones is good. The potential for eliminating or minimizing psychological barriers to change is highly variable and completely under the patient’s control. The best the dentist can hope to accomplish is to raise the patient’s consciousness to the recognition that the barriers do exist. With time, and a professional and supportive approach, these patients may accept the responsibility to change. Attempting to improve the patient’s sense of self-worth is a similarly difficult undertaking with no guarantee of success. However, if early in the treatment the dentist can bring about a positive change in the patient’s appearance, the person may be buoyed by an improved sense of self and begin to develop faith that the effort is worthwhile. When these issues are dealt with effectively, educating the patient about the benefits of dental treatment is much easier.
It is also important to evaluate the patient’s potential for improving oral self care. The motivationally impaired patient often has poor oral home care, creating an unfavorable environment for the long-term success of any treatment. Most patients are receptive to some level of oral health instruction. How much they absorb and how effectively they implement that instruction varies, however. It is particularly important for the office staff to be attuned to the patient’s dental history, knowledge base, and specific barriers to care. The dental staff, and the hygienist in particular, must have an understanding of the patient’s individual needs and take those needs into account when crafting an instructional plan. With the motivationally impaired patient, a routine impersonal approach to oral physiotherapy instruction is unlikely to succeed. A compassionate, thoughtful, and patient-specific approach to educating the patient regarding effective oral self care is much more likely to produce the desired result. It can also result in other positive changes, such as giving the patient a greater appreciation for the benefits of comprehensive dental care.
MAKING A TREATMENT DECISION
Once a determination has been made as to whether the motivationally impaired patient wants to improve his or her oral health status, a plan of care must be developed and informed consent obtained. If the patient remains unmotivated or is unwilling to modify the circumstances and attitudes that led to the oral problems, then there may be no alternative but to recommend the extraction of questionable teeth and transition the patient to complete dentures. If the patient is receptive and motivated to change, however, then more comprehensive treatment can be suggested. Some of these treatment options are discussed later in this chapter.
The presentation of treatment options carries unique importance with the motivationally impaired patient. At the outset, such a patient is more likely to have an unusually pessimistic view of the treatment and its chances of success. The same patient may also have unrealistic expectations about how long or how demanding the dental treatment will be. Although candid, the discussion must not be coercive, threatening, or intimidating. The patient must feel comfortable enough with the provider to be able to share what are often deep-seated concerns and reservations.
For this patient, informed consent also carries greater than normal significance/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses