Chapter 17
Rhytidoplasty
History of Rhytidoplasty
The manifestation of human desire to regain a younger appearance that has been lost over time due to the natural aging process is the basis of esthetic surgery. The overall goal of these procedures is to restore age and sun-damaged facial anatomy to a normal, more youthful condition. Although variable by ethnic and genetic background, youthful appearance generally consists of a tapered, slightly ovoid face, and smoothness of the facial skin with full soft tissue volume.1–3 The signs of aging are also variable and depend on an array of factors. Illnesses, sun exposure, skin type, medications, and environmental factors can all contribute to the phenomenon we know as aging. Elastin and elastic tissues within the face undergo abnormal changes that allow the skin and deeper tissues to droop and sag. The deep anatomical structures of the face, which include the orbicularis oculi and platysma muscles, cheek fat, and superficial fascia, also change position over time and play an important role in this process. Visible signs of this ongoing course are proportional to the degree of change in position of these deep anatomical structures within the face. As these structures become increasingly ptotic, the desirable, youthful appearance diminishes.4,5
The evolution of facial cosmetic surgery began over 2000 years ago in ancient India and Egypt, and a myriad of surgical specialties have advanced and modified the rhytidoplasty (commonly referred to as a face-lift) procedure since that time. The modern face-lift procedure, however, began in the early nineteenth century and was first attempted by German surgeons. In this procedure, the skin was stretched and ellipses of excess skin were excised without undermining the tissue.4,5 The skin flap was based on vascular perforators of the skin, which were, unfortunately, interrupted during the procedure. The blood supply to the skin was then based completely on vascular attachments to nearby undissected skin. Despite its eventual maturation to a more scientifically based and viable flap surgery, this procedure failed to address the deeper soft tissues and often resulted in an unnatural, stretched-face appearance that failed to create the desired youthful appearance and relapsed too quickly. Nevertheless, this technique was used for many decades and provided an effective, if less than ideal, means of improving skin laxity.6
In the 1960s, Aufricht and others recognized that to obtain natural and long-lasting results, the deeper structures of the face had to be addressed in addition to the skin. His description included the performance of soft tissue suspension sutures with plication. This generally resulted in a more natural postoperative appearance that lasted a longer time before the tissues began to relapse.6
In 1974, Skoog described an important new concept and technique during which dissection was carried beneath the superficial fascia of the face. As described by his innovative technique, the skin and platysma of the lower face were raised and repositioned as a cohesive unit. In contrast to earlier subcutaneous techniques that simply redraped the skin over aged, ptotic, deeper structures, this procedure addressed these anatomically deep structures by including them in the dissection.7–9
Also beginning in the 1970s, work published by Mitz and Peyronie, with contributions and under the direction of the famed Paul Tessier, coined the term superficial musculoaponeronic system (SMAS) to replace the previously known superficial fascia as described by Skoog.6,10 Their work and publication gave birth to the contemporary subcutaneous face-lift with concurrent elevation of the SMAS. This technique was straightforward for experienced surgeons owing to the fact that the SMAS dissection was an easy addition to the commonly performed subcutaneous flap. In addition to repositioning the cutaneous tissues of the lower face, this innovation undermined the platysma muscle of the lower face and repositioned it similarly to the cutaneous tissues, providing structure and longevity. Inadequacies of this procedure, however, included lack of cheek fat repositioning and nasolabial fold exclusion.7,11–15
Beginning in the early 1980s, Hamra began developing techniques that addressed the issues of the nasolabial fold and cheek fat. The triplane face-lift technique, which was published in 1982, was essentially a variation on the Skoog flap. In 1986, Hamra described a deep-plane rhytidectomy technique. This procedure raised the cheek fat from the underlying muscles of facial expression (zygomaticus major and zygomaticus minor) while remaining attached to the skin. This flap is then repositioned in a musculocutaneous fashion to include both the platysma of the lower face and the aforementioned cheek fat. As described by Hamra, this procedure resulted in superior improvement of the nasolabial fold while enhancing the jawline. Evolutionarily, this procedure began to include the orbicularis oculi muscle and the flap was repositioned with vectors that opposed those of aging (superolateral for the midface and superomedial for the orbicularis oculi region). After inclusion of the orbicularis oculi muscle, the term composite rhytidectomy was used to describe the procedure, which was now intended to address all three anatomical elements of the aging face.7,12–14,16,17
Although there continues to be a variety of different techniques, no one procedure has proved singular in its utility.16 Surgeons choose procedures based on familiarity, educational background, or particular anatomical needs. As with most surgical procedures, it is best to have more than one option available, choosing the one most appropriate based on the specific needs of the patient.
Anatomy
A thorough understanding of the anatomy of the head and neck is a critical element to any surgeon performing face-lifting procedures. When performing a face-lift, many anatomical structures must be taken into consideration and their precise location and orientation is crucial to predictably good results.
The skin of the face and neck represents the most external and recognizable structure that is evaluated and considered during face-lift surgery. However, one must also recognize the significant importance of the underlying nerves, vessels, SMAS, muscles, ligaments, and bone, as they contribute greatly to the appearance of the overlying skin.
The skin is a very demanding structure that requires precise handling during any surgical technique. Aside from its cosmetic importance, this squamous epithelium also serves as the body’s major defense organ. The epidermis is divided into five layers from superficial to deep consisting of the stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and the stratum basale. The cellular component of the epithelium is about 95% keratinocytes but also includes melanocytes, Langerhans cells, and Merkel cells. The keratinized stratified squamous epithelium of skin (epidermis) overlies a complex dermal substructure.
The deeper dermis is divided into papillary and reticular subsets. The papillary dermis is the uppermost layer of the dermis. It is intimately associated with the rete ridges of the epidermis and composed of fine and loosely arranged collagen fibers. The reticular dermis is the lower layer of the dermis. It is composed of densely packed collagen fibers and serves as the primary location of dermal elastic fibers.
Deep to the dermis lies the hypodermis, consisting primarily of the subcutaneous fat. The thickness of this layer varies greatly among individuals. Variability also exists in different locations on the face. This fatty layer is divided into lobules by fibrous connections, or septa. The cheeks and neck often present with significant amounts of subcutaneous fat in comparison with other areas of the face such as the forehead and chin. This is important when considering the various face-lift procedure options.9,18–20
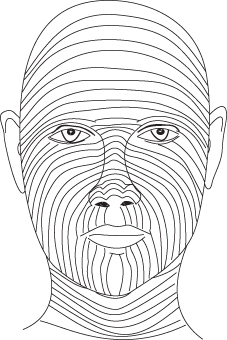
As will be discussed later in this chapter, it is imperative that the surgeon consider relaxed skin tension lines when planning rhytidoplasty procedures (Figure 17.1). These lines, by definition, are lines of skin tension present when the skin is in its most relaxed state. In order to achieve the least amount of scarring following a skin incision, the direction of the incision relative to the lines of relaxed skin tension must be considered.21 Although every incision will create a scar, creating a scar that follows these lines produces the most ideal cosmetic result.
Figure 17.1 Relaxed skin tension lines.
For obvious reasons, a thorough knowledge of the facial nerve anatomy is imperative when performing rhytidoplasty. The incidence of injury to this nerve is low, approximately 0.5–2.6%, but remains of significant concern due to the devastating nature of any injury to it during surgery. The course of the facial nerve as it emerges from beneath the superficial lobe of the parotid progresses from deep to superficial. Anterior and inferior to the ear, it is deep to the deep investing fascia. Continuing distally, the nerve separates into its two main trunks, and eventually into its five distal branches. The frontal branch becomes more superficial at the level of the zygomatic arch. Here, it lies just beneath the temporoparietal fascia. As the SMAS layer is a continuation of the temporoparietal fascia, SMAS imbrications must only be accomplished inferior to the level of the zygomatic arch in order to avoid the frontal branch of the nerve. The zygomatic and buccal branches of the facial nerve course between 0.8 and 3.5 cm anterior to the external auditory canal as they travel toward the anterior edge of the parotid gland. The zygomatic branch exits the parotid gland in close association with Stenson’s duct and deep to the parotideomasseteric fascia. As it continues forward, it terminates deep to the zygomaticus major muscle. The buccal branch traverses the surface of the masseter muscle, deep to the parotideomasseteric fascia, as it travels from deep to superficial. The marginal mandibular branch exits the parotid gland superior to the angle of the mandible in 80% of people. In 19% of cases, it may pass inferior to the mandible as much as 3 cm. At the antegonial notch, the mandibular branch crosses, or already has crossed, the mandible deep to the parotideomasseteric fascia or superficial layer of the deep cervical fascia. It continues anteriorly to innervate the depressors of the lips and mentalis muscle. The cervical branch of the facial nerve exits the parotid gland below the angle of the mandible and begins deep to the superficial layer of the deep cervical fascia. It continues anteriorly to traverse the undersurface of the platysma and provide its innervation.22
Knowledge of the position of these various branches relative to the level of dissection during face-lift surgery is imperative to preclude serious complications and should be forefront in the mind of the surgeon at all times.22–28
The ultimate vascular supply to the face originates from the common carotid artery and its branches. The common carotid branches into internal and external components. The ophthalmic portion of the internal carotid gives rise to the ophthalmic artery that serves as a major tributary that supplies the face. The divisions of this major artery supply the forehead, nose, and eyes.29
The external carotid artery gives off eight major divisions but the primary one in the area of the rhytidoplasty procedure is the facial artery. The facial artery arises in the carotid triangle and provides significant blood supply to the face, terminating as the superior and inferior labial arteries to the lips, and the angular artery of the lateral aspect of the dorsum of the nose. The internal maxillary artery is one of the terminal braches of the external carotid. It arises behind the neck of the mandible and gives rise to the infraorbital artery. This branch of the maxillary artery emerges below the inferior orbital margin and supplies the lower eyelid. The final terminal branch of the external carotid artery is the superficial temporal artery. This artery begins within the substance of the parotid gland and travels within the SMAS across the zygomatic arch. It gives off the transverse facial artery that ultimately supplies the lateral canthal area. The superficial temporal artery continues superiorly above the zygomatic arch to give off its terminal branches that supply the forehead, parietal, and frontal areas.30,31
Critical to the surgical anatomy of the face-lift is the SMAS. The SMAS is essentially an inferior continuation of the galea aponeurotica of the skull and, as it continues inferiorly, becomes the platysma muscle (Figure 17.2). The muscles of facial expression are interconnected by this layer and it acts as a conduit from facial muscle contraction to skin movement. The SMAS is attached by retinacular cutis fibers within the subcutaneous layer to the skin.26 Facial expressions are a consequence of contractions of the SMAS that are then transmitted intimately to the skin. Damage to or interruption of these connections can lead to significant distortion of facial expression.20
Figure 17.2 Coronal cross section anatomy.
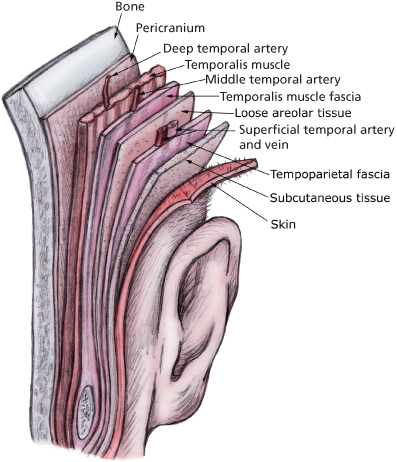
As the SMAS has now become the major important layer in performing a good contemporary face-lift, it is important to relate all the significant anatomical structures to this layer. Within the confines of the typical face-lift dissections, the major vessels and nerves of the face lie deep to the SMAS. Although in the lower face cranial nerve VII and sensory nerves lie deep to the SMAS,8 as one progresses superiorly, cranial nerve VII becomes more superficial as it crosses the zygomatic arch and continues within the SMAS. Its terminal innervation occurs within the frontalis muscle.
SMAS ptosis is responsible for many of the aging effects seen over time. During most current face-lifting procedures, the SMAS must be addressed to correct laxity and droop. Failure to do so will inevitably result in rapid relapse and a poor surgical result.
Patient Evaluation
Patterns of facial aging occur as the structural units of the face become increasingly ptotic, volume loss occurs, and skeletal changes manifest. When evaluating the patient for a face-lifting procedure, a balance between patient expectation and surgical limitations must be considered. The surgical plan should be geared toward the esthetic goals of the patient. Oftentimes, these goals include restoration of smooth and taut facial contours, elimination of deep lines and creases, recreation of malar fullness relative to submalar depression, and reestablishment of overall facial symmetry.32 During the evaluation, the surgeon should keep in mind the various procedures available and form a consensus that balances the desires and limitations of both parties.33
Prior to surgery, the patient must undergo a complete medical history and physical examination. Major medical conditions must be addressed and controlled prior to the initiation of the surgical procedure. Consultation with the appropriate medical professional must be obtained regarding diseases of the cardiovascular, pulmonary, hepatic, or renal systems. Immunocompromising conditions such as diabetes, autoimmune and immunodeficiency syndromes, and chronic use of corticosteroids must also be attended to in the preoperative period. Inherent to this evaluation is the patient’s physical capacity to tolerate deep sedation or general anesthesia. A current medication list is also essential, as certain medications such as warfarin, aspirin, and nonsteroidal anti-inflammatory drugs play a significant role in both the intraoperative and postoperative course.
Over-the-counter drugs not regulated by the Food and Drug Administration such as gingko, garlic, and ginseng can produce similar anticoagulatory effects as seen with the more traditional prescribed anticoagulant medications. Any omission to recognize these conditions may lead to a poor anesthetic or surgical result. Evaluation of previous surgical scars of the body, and particularly of the head and neck, may provide great insight to the patient’s healing capacity and any risk of hypertrophic scarring or keloiding.34
A thorough investigation of the patient’s social history must be accomplished before considering face-lift surgery. Tobacco use, with its attendant microvascular constriction secondary to the effects of nicotine, can result in less than ideal, or in some cases, disastrous, results. As described by Rees et al., a face-lift patient who smokes has 12.46 times the chance of suffering potentially devastating skin slough than a patient who does not smoke. Alcohol use in excess must alarm the practitioner to potential hepatic effects and poor nutritional status that could lead to delayed healing. Many illicit drugs (such as cocaine) can have detrimental effects similar to tobacco use. Cardiovascular instability and disease resulting from such drug use can occasionally lead to fatal effects during anesthesia.35–37
During patient evaluation, the psychological history can provide insight into the motivation and expectations of the face-lift patient. Often, the perception of cosmetic surgery patients is of vain individuals with the simple desire to become beautiful. On the contrary, according to Lejour et al., they are generally people with a self-image of physical inferiority.38 Often, this will lead to patient dissatisfaction, as no procedure would likely change this perception.
Many patients also have unrealistic expectations of what can be accomplished by current surgical techniques, regardless of the expertise of the surgeon. Finally, some patients have the desire to treat issues different from those visualized by the surgeon. As an example, the practitioner may diagnose severe rhytides around the mouth and plan surgery around that area, while the patient only cares about the dyschromia of their cheek. This will terminate in a result that makes neither party happy.
A simple answer to this is to have the patient hold a face mirror in front of themselves while describing what they see and what they would like to have corrected. This allows both the surgeon and the patient an opportunity to have input on possible surgical options. Other good methods to improve the understanding of the patient include having the patient look in the mirror while extending the neck, and the surgeon using his or her hands to gently mimic the effects of the SMAS placation, both of which can roughly show the patient the expected results of rhytidoplasty.1,18,34
Because the surgeon is usually ill equipped to make this type of psychological judgment, any patient whose cognitive condition seems abnormal should be referred for psychological evaluation and counsel before surgery is initiated.34 If this important concept is ignored, the postoperative emotional disturbances can potentially be significant.
Informed consent is a legal process where the patient gives consent based on a clear realization and understanding of the facts, risks, benefits, and alternatives to treatment. Necessary to proper informed consent, the patient must possess adequate reasoning capabilities and be in possession of all relevant facts related to the procedure at the time consent is given. Any impairment in reasoning and judgment must be considered when providing informed consent. If cognitive incapabilities are present, informed consent cannot be obtained.
The evaluation of the face is oftentimes the most critical component to the successful outcome of face-lift surgery. This concept has been well established over time and supported by the literature. A detailed preoperative evaluation has as its ultimate goal the improvement of facial balance and shape and its use is advocated to help provide the best overall results.
Patterns of facial aging can be most clearly seen in the midface, as volume loss, skeletal changes, and gravitational descent are readily noticeable in this area. Visible folds and soft tissue sag are often manifestations of the transition point between subcutaneous and deep fat. As the midface becomes fuller laterally, the face assumes a more aged, round appearance and it loses its youthful, tapered appearance.39,40
A planned, systematic evaluation by the surgeon allows for the appropriate face-lifting procedure to be chosen along with other necessary or optional ancillary procedures. When evaluating a patient, the face should first be viewed as a complete unit. In this assessment, one should observe the patient’s skin texture and quality, its thickness, redundancy, rhytides, pigmentation, and previous scars. Facial shape and contour should also be noted.
Continuing through the evaluation, the face should then be examined while divided into facial thirds. The upper third extends from the hairline to glabella, the middle third of the face extends from glabella to subnasale, and the lower third is bounded by subnasale superiorly and the chin inferiorly.
In the evaluation of the face, one should consider the size and depth of the nasolabial folds, presence of jowling, perioral rhytides, and the position, shape, and type of attachment of the ear lobule.40
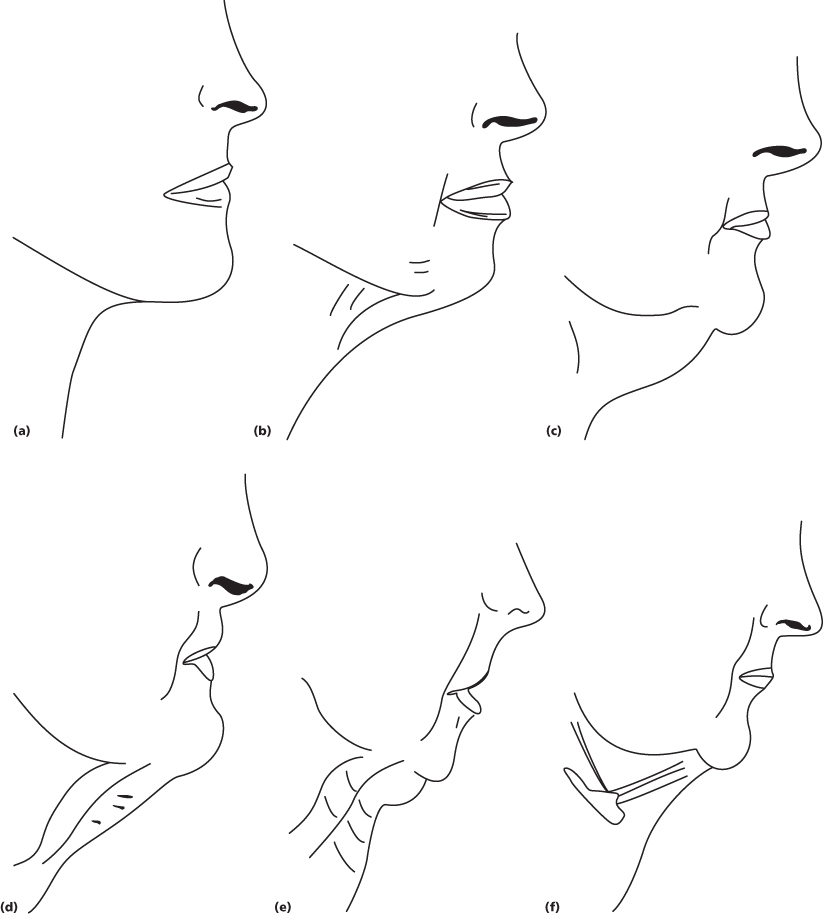
In 1978, Dedo published a classification of the neck that divides the neck profile into six unique categories (Figure 17.3). Using this classification aids the surgeon in choosing an appropriate set of procedures to correct the patient’s unique anatomical problems.41
Figure 17.3 Dedo classification. (a) Class 1: demonstrating good muscle tone, no submental fat, and a well-defined cervicomental angle. (b) Class 2: demonstrating cervical skin laxity and an obtuse cervicomental angle. (c) Class 3: demonstrating submental fat accumulation; may require submental lipectomy. (d) Class 4: demonstrating significant platysmal muscle banding. (e) Class 5: demonstrating retrognathia and/or microgenia. (f) Class 6: demonstrating a low hyoid.
Inherent to face-lift surgery it must be recognized that, as with most cosmetic surgeries, all the effects of facial aging cannot be corrected by this one procedure alone. Many innovations and modifications of the procedure have been attempted and will be discussed later in this chapter. But generally speaking, the face-lift does not address the upper face. In cases where this area does need to be treated, other procedures (such as endoscopic or open brow lifting or blepharoplasty) can be additionally performed to accomplish the needed corrections.
In addition to the clinical exam, it is mandatory to have a full set of high-quality photographs. These are used for patient evaluation purposes as well as for a medico-legal record. Often, patients who see facial changes occurring over a long period of time will feel that the results of their rhytidectomy are less than they expected. When shown the preoperative pictures, they will often come to the realization of how much was actually accomplished.
Pictures that should be taken include full-face frontal and lateral views, full-face frontal smile, three-quarter left and right full-face views, a submental-vertex view, and when considering platysmal plication, a grimacing picture (Figure 17.4). These allow the surgeon to consider all the treatment options, even without the patient being present.
Figure 17.4 Pictures for evaluation and documentation purposes. (a) Full-face frontal. (b) Lateral. (c) Full-face smiling. (d) Three-quarter left view. (e) Three-quarter right view. (f) Submental vertex. (g) Grimacing picture.

A number of excellent software packages are now available for soft and hard tissue cosmetic surgery treatment planning. Many of these allow for facial morphing to provide prediction images. It must be remembered that these are not 100% accurate, however, and the patient should be informed of this to prevent unreasonable expectations.
Rhytidectomy Procedures: a Review of Techniques
In 1974, Skoog established a breakthrough in the rhytidectomy technique as he described a procedure that involved more than simple stretching and excision of the skin as described and previously executed by the Germans. In this new procedure, the SMAS was also addressed, as dissection was carried underneath this layer. Since that time, a plethora of variations of the SMAS face-lift have been introduced and modified. The foundation of all face-lifting procedures today requires mobilization of the ptotic SMAS as well as the overlying superficial structures. The flap is then advanced to a more posterior-superior position in relation to the deeper skeleton and affixed to maintain its position over time.9,42
Rhytidectomy Skin Markings and Incision Design
Rhytidectomy skin marking and incisions are critical components of the operation. As described by Perkins and Dayan, before the commencement of the procedure, the surgeon must thoroughly evaluate and plan the incisions for three critical areas that are specific to the patient: the temporal, preauricular/tragus, and postauricular/occipital regions.
Incision placement in these areas depends on the patient’s sex, local anatomical factors (such as hairline and skin thickness), and the degree to which these regions need improvement.32
Proper preoperative marking of the planned incision is also an important and integral portion of the face-lift procedure. The patient must be marked in the sitting position to mimic natural gravitational forces. Beginning with the temporal incision, the traditional design consists of a curvilinear incision in the temporal hairline that continues inferiorly in a vertical fashion toward the tragus. This design in the temporal area has the advantage of allowing greater pull to be accomplished in the forehead area without a forehead or brow lift. The disadvantage is that it often results in temporal alopecia and movement of the temporal tuft of hair. Many surgeons therefore advocate a temporal incision that scallops as it follows the hairline (Figure 17.5). It is important to design the incision parallel to the hair shafts (rather than the typical perpendicular angle for most skin incisions) to prevent unnecessary hair loss mediated by inadvertent injury to the subjacent follicle.43–46
Figure 17.5 The temporal incision design. (a) Hair-sparing temporal incision. (b) Vertical temporal incision.

Continuing inferiorly, the preauricular incision should be planned to minimize postoperative visibility (Figure 17.6). A pretragal or posttragal incision can be placed depending on the contour of the tragus and the presence of a preauricular fold. The pretragal incision can be accomplished inconspicuously if a significant pretragal fold is present. If this is not present, the surgeon should consider a posttragal incision.44,47
Figure 17.6 The preauricular incision design. (a) Pretragal preauricular incision. (b) Posttragal preauricular incision.
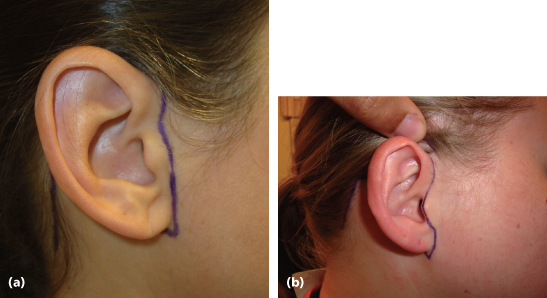
The most common incision design is to place the preauricular incision just behind the posterior edge of the tragus; it otherwise follows the normal skin folds and curvature of the preauricular area above and below the tragus. The incision should be placed 1 mm behind the tragus as it follows the helical insertion. It should exit at the junction of the earlobe and the face.
In patients with a preauricular fold, the preauricular incision works quite well, and is easier to perform than the posttragal incision. As this incision has been used for many years for temporomandibular joint (TMJ) surgery, it is well known to have very acceptable cosmetic results and can, in fact, sometimes be more esthetic than the posttragal incision, where scar contracture can cause the tragus to look distorted after healing. In addition, in males, it is important to al/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


