17 DEFINITIVE CASTS AND DIES
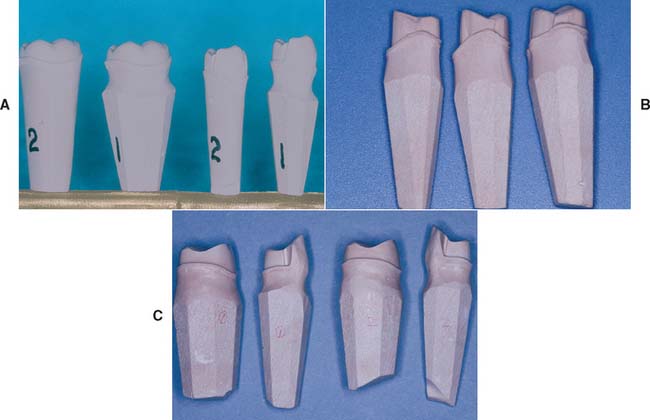
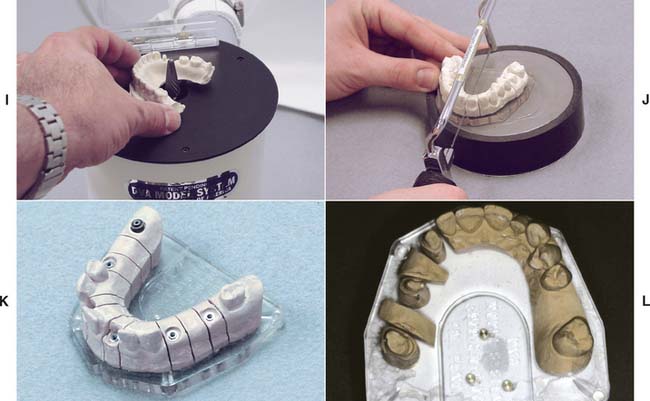
The definitive cast (or master or working cast) is the replica of the prepared teeth, ridge areas, and other parts of the dental arch. The die is the positive reproduction of the prepared tooth and consists of a suitable hard substance of sufficient accuracy (usually an improved stone, resin, or metal) (Fig. 17-1).
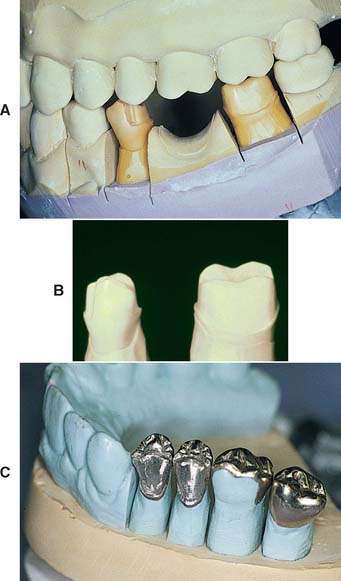
Fig. 17-1 Removable die system. A, Definitive cast. B, The individual dies. C, Epoxy die.
(C, Courtesy of Dr. J. H. Bailey.)
PREREQUISITES
The cast that will be used to make the fixed restoration must meet certain requirements. It must reproduce all details captured in the impression and should be free of defects. Depending on their location, however, minor imperfections may be acceptable (Fig. 17-2). The cast must meet certain requirements:
The die for the fixed restoration also must meet certain requirements:
MATERIALS SCIENCE
Gypsum
CaSO4 • ½H2O + 1½H2O → CaSO4 • 2H2O
The hemihydrate is manufactured by heating the dihydrate under controlled conditions to drive off some of the water of crystallization (a process called calcination). The differences between the various types of dental gypsum are attributable to calcination. The physical properties of die stone are improved over those of dental stone and plaster because less water is needed to obtain a sufficiently fluid mix.*
Hand mixing of gypsum products is easy, but results are better when the mixing is done mechanically in a vacuum. Porosity is reduced, with a concomitant increase in strength, after only 15 seconds of mechanical mixing. Newly poured casts should be left undisturbed for at least 30 minutes; superior results are achieved at 1 hour, although these times may vary among brands.
Surface detail reproduction is acceptable with type IV and type V gypsum products. The materials are capable of reproducing a 20-μm-wide line as prescribed by ADA specification No. 19.1 However, not all brands of die stone are compatible with all brands of impression material,2,3 and if poor surface detail reproduction is experienced, an alternative product should be selected.
Gypsum’s greatest disadvantage is its relatively poor resistance to abrasion. Attempts to overcome this have included the use of so-called “gypsum hardeners.” Although these materials (e.g., colloidal silica) have relatively little effect on the hardness of the stone, they improve abrasion resistance (some by as much as 100%).4 Their use is accompanied by a slight increase in setting expansion, but such is probably not clinically significant. An alternative approach5 is to impregnate the surface of the die with a low-viscosity resin such as cyanoacrylate. As mentioned earlier, abrasion resistance is the physical property most improved by this technique. Care is needed when the resin is selected and applied so that the resin film will have no significant thickness.6 Experts continue their efforts to improve the properties of die stone. One approach is to apply additives used in industrial applications (e.g., concrete manufacture) to dental gypsum products.7 Another is the use of a gum arabic, calcium hydroxide mixture.8 Resin-strengthened gypsum products such as ResinRock,* with high strength and low expansion,9 are also popular and are particularly suitable for casts for implant restorations (see Chapter 13).
Resin
Epoxy resins suitable for fabrication of precision dies are available, although there is a great deal of variability among brands.10 The amount of shrinkage upon polymerization is quantitatively about equal to the expansion with gypsum. Polymerization shrinkage is less of a problem with newer formulations11 and polyurethane resin.12 When used with poly (vinyl siloxane), contemporary resin systems produce complete arch casts with similar dimensional accuracy to traditional die stone.13 In general, detail reproduction is better14; however, prostheses fabricated on resin dies tend to fit more tightly than those made on gypsum.15
Electroplated Dies
Besides resin, electroplating can be used to overcome the poor abrasion resistance of gypsum. This technique16 has been in use for many years and involves the deposition of a coat of pure silver or copper on the impression. The areas to be plated are first coated with finely powdered silver or graphite to make them conduct electricity, and the impression is then placed in an electroplating bath. A layer of pure metal is deposited on the impression and is supported with type IV stone or resin.
Although electroplating has been in use for some time, several problems remain. Variable degrees of distortion commonly occur, and the technique must be performed slowly; otherwise, distortions in the metal subsequently stress the impression. The time necessary to produce a cohesive film of metal (typically 8 hours) is ample for the development of dimensional changes in the impression. However, when made properly, an electroplated die can be as accurate as a stone die,17,18 although not all impression materials are suitable for plating. Because of their low surface energies, silicone impression materials are difficult to electroplate evenly. Some brands, however, are easier to plate than others.19 Polyether impressions, because of their hydrophilic nature, imbibe water and become distorted; they therefore cannot be plated accurately. Polysulfide polymers can be silver plated, but it is much more difficult to copper plate them. The main drawback of silver plating is the use of a cyanide solution, which requires special precautions because of its extreme toxicity.
Flexible Die Materials
Flexible die materials are similar to heavy-bodied silicone or polyether impression materials (see Chapter 14) and have been used to make interim restorations20,21 or indirect composite resin inlays or onlays22,23 chairside. The advantages of the flexible material over a stone die include more rapid setting and the ease of removal of the interim restoration or inlay. When choosing materials for flexible dies, the dentist must be sure to select a compatible combination of impression and die materials that provides good surface details. One study24 revealed that the best detail reproduction was obtained when Impregum F die material* was combined with Extrude Light impression material.†
SELECTION CRITERIA
Choosing one cast-and-die system over another depends on several factors:
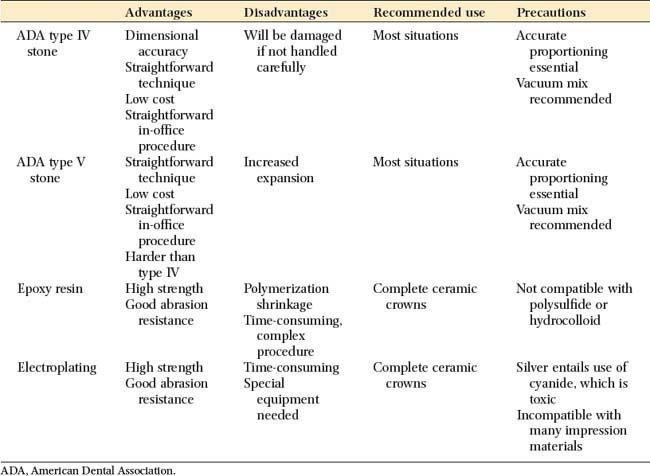
The advantages and disadvantages of the available materials are summarized in Table 17-1.
Available Methods
Removable dies
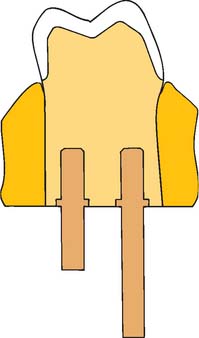
In a removable die system (see Fig. 17-1), the die is an integral component of the definitive cast and can be lifted from the cast to facilitate access. Precise relocation of the die in the definitive cast is crucial to this system’s success and is usually accomplished with brass pins or dowels (Fig. 17-5). When a single dowel is used, it should have at least one flat surface to provide resistance against rotation. Alternative methods (e.g., the popular Pindex* system [Fig. 17-6]), use multiple or interlocking dowels to ensure such resistance.

Fig. 17-6 Removable dies made with the Pindex (Whaledent) dowel system (see Fig. 17-21).
(Courtesy of Coltène/Whaledent AG, Altstatten, Switzerland.)
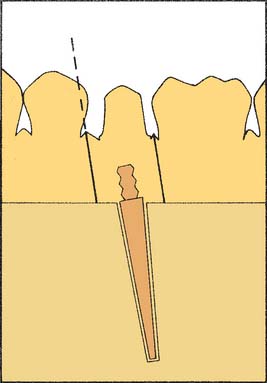
The cast is made in two pours of type IV or V stone† of contrasting colors: the first forms the teeth, and the second forms the base of the cast. The area to be removed is coated with a separating agent before the second layer is poured. In other areas, undercuts are provided to prevent unwanted separation. The location and orientation of the dowels are critical; if they are improperly placed, the dowels do not allow the die of the prepared teeth to be withdrawn from the cast (Fig. 17-7).
In normal situations, dowels are positioned in the stone before it is set. However, drilling the cast and cementing the pins into the set stone are also possible.25
The Pindex system is designed to facilitate this latter technique. All removable die systems depend on careful execution so that the die will separate cleanly and return to place accurately. In one study, investigators found similar accuracy with four removable die systems, although the Pindex system showed the least horizontal movement, and the brass dowel pins produced the least occlusogingival reseating discrepancy.26
Solid cast with individual die
The solid cast-and–individual die system, also referred to as the multiple-pour technique, has certain advantages over the removable die system; its primary advantage is its simplicity. It may also be slightly more accurate.27 When the impression is judged to be satisfactory, it is poured in type IV or V stone in the area of the preparation or preparations only. When set, it is separated. A second pour is then made of the entire arch. (Sometimes the second pour is used for an additional set of individual dies for polishing, and the solid cast is obtained from a third pour.)
The first pour, which is the most accurate, is trimmed into a die with a handle of sufficient length (similar to a tooth root [Fig. 17-8]). The complete arch cast (second pour) is mounted on an articulator. The wax pattern is started on the initial pour (the die) and is then transferred to the articulated cast for refinement of axial contours and occlusal anatomy (see Chapter 18). When completed, this pattern is returned to the die so that the margins can be readapted immediately before investing.
Alternative die systems
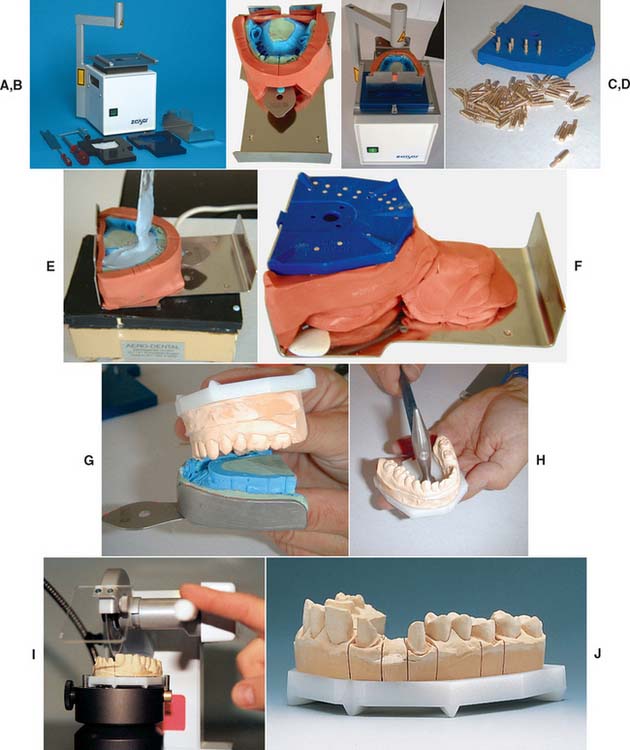
The Di-Lok* technique (Fig. 17-9) involves the use of a specially articulated tray for precise reassembly of a sectioned definitive cast. The impression is poured, and the cast is trimmed into a horseshoe configuration that fits in the special tray. The tray is filled with a second mix, and the cast is seated. When the stone has set, the tray is disassembled, saw cuts are made on each side of the preparation, and the resulting die is trimmed. The cast and die can be reassembled in the tray, which is then mounted on an articulator. A disadvantage of this system is that the overall size of the tray can make articulation and manipulation awkward and difficult.
The DVA Model System* (Fig. 17-10) and the Zeiser model system† (Fig. 17-11) use a precision drill and special baseplates that are aligned and drilled to provide die removal. These systems offer the advantage of allowing for the expansion of stone, which is relieved by the saw cuts.
Choice of Definitive Cast-and-Die System
The choice of a specific technique relies on operator preference and an assessment of each method’s advantages and disadvantages. If they are used properly, all the available systems achieve clinically acceptable accuracy.28 When establishing a new relationship with a dental technician, it is important to determine which cast-and-die systems are preferred and why the technician has chosen them. Close cooperation between the dentist and technician is a key factor in fixed prosthodontics.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses