17
Class II division 2 malocclusion
INTRODUCTION
The British Standards Classification defines Class II division 2 malocclusion as follows: the lower incisor edges occlude posterior to the cingulum plateau of the upper incisors; the upper central incisors are retroclined, the overjet is usually minimal but may be increased. Among Caucasians, the prevalence is reported to be about 10%.1
AETIOLOGY
This malocclusion has a strong genetic component2 with most resulting from the interplay of skeletal and soft tissue factors.
Skeletal Factors
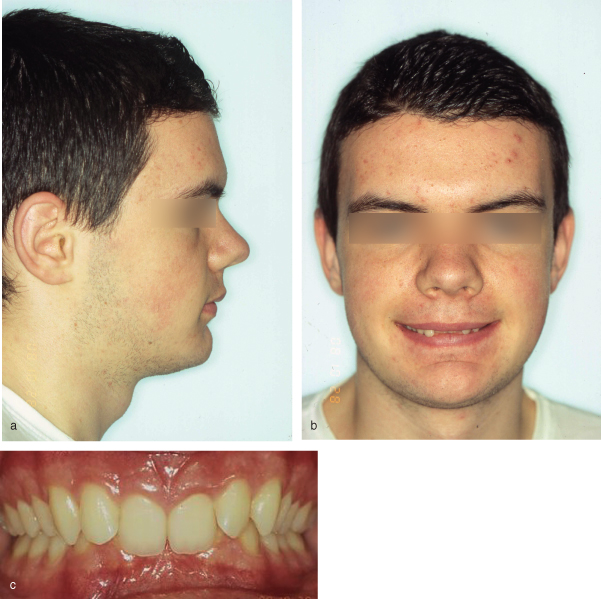
Usually the skeletal pattern is mildly Class II, due to mandibular retrognathia, but it may be Class I or even mildly Class III.3,4 A reduced lower facial height is typical,5 in association with an anterior (anticlockwise) mandibular growth rotation, which tends to increase the overbite and lead to forward projection of the chin2,5 (Figure 17.1a). Due to the relatively wide maxillary base, and narrower lower intercanine width,6 the first premolars may be in lingual crossbite (scissors bite).
Figure 17.1 (a) Class II skeletal pattern with reduced FMPA, deep labiomental fold and relatively prominent chin point; (b) associated high lower lip line evident on smiling; and (c) typical Class II division 2 malocclusion.
Soft Tissue Factors
As the lower facial height is reduced, the lower lip line is high on the upper incisors, covering more that one-third of the labial surface, and is the predominant cause of their retroclination7 (Figure 17.1b). Increased resting lower lip pressure (∼2.5 times as high as the upper lip resting pressure) is a complementary factor.8 Upper and lower lips are also thicker compared with Class 1 malocclusion.9 Depending on the lower lip level, the relatively shorter maxillary lateral incisor crowns may either be retroclined along with the central incisors or escape lower lip control and be of average inclination but mesiolabially rotated, a manifestation of inherent crowding (Figure 17.1c). The reduced lower facial height also leads to a relative soft tissue excess of the lower lip, reflected in the commonly observed deep labio-mental fold. Where the lips are strap-like regardless of the skeletal pattern, the upper and lower incisors may be retroclined (bimaxillary retroclination; Figure 17.2); this is sometimes associated with a gummy smile and may be aggravated by upper incisor overeruption.
Figure 17.2 Bimaxillary retroclination; peg-shaped lateral incisor; retained primary canine (the permanent canine was palatally displaced).

Dental Factors
The cingulum on the upper incisors may be reduced or absent, thereby allowing overeruption of the lower incisors to increase the interincisal angle and deepen the overbite.10 The latter may be exacerbated by a Class II skeletal pattern and retroclination of upper and lower incisors. Relative to other malocclusion types, a more acute upper incisor crown–root angulation10 and smaller mesiodistal width of the upper and lower incisors have been identified.2 There is also a higher incidence of palatally impacted maxillary canines11 and of peg-shaped or absent maxillary lateral incisors12 (Figure 17.2). Retroclination of the upper incisors, and possibly of the lower incisors, worsens pre-existing crowding.
TREATMENT PLANNING
The factors which should be considered, in particular, with regard to treatment planning are given in Table 17.1. Two principal decisions have to be made with regard to treatment in relation to the incisor relationship and crowding: to accept or correct the incisor relationship; to extract or not for relief of crowding and incisor alignment.
Table 17.1 Factors to consider in treatment planning of Class II division 2 malocclusions
| Factor | Implications for management |
| Underlying anteroposterior and vertical skeletal discrepancy | In general, the more Class II the skeletal pattern and the more reduced the Frankfort-mandibular planes angle (FMPA), the more difficult to achieve optimal dentofacial correction by orthodontic means alone. Consider along with growth potential and profile (see below) |
| Growth potential and pattern of facial growth | Skeletal II deep bite correction is facilitated by favourable facial growth. Inherent forward mandibular growth rotation tendency (anticlockwise) aids skeletal Class II correction but tends to increase overbite unless the interincisal angle is altered and a cingulum stop created. In an adult, overbite reduction by incisor intrusion rather than molar extrusion is advisable as the latter is unlikely to be stable |
| Profile considerations | Little objective difference exists in lip fullness between extraction and non-extraction treatment, but the latter is favoured, particularly with bimaxillary retroclination. For an unfavourable profile (marked skeletal Class II and very reduced FMPA) in an adult, a combined surgical orthodontic approach is required |
| Lower lip level | Inferior lower lip movement away from the upper incisor crowns is essential to promote stability. Where the lower lip covers the full crown height of the upper incisors, permanent retention is likely |
| Presence and degree of crowding | Avoid lower arch extractions as may encourage overbite increase by retroclination of the labial segment. Because it is often trapped lingually by the upper incisors, proclination of the lower incisors and mild intercanine expansion is possible to relieve crowding and may be reasonably stable |
| Depth of overbite and incisor inclinations | Overbite depth and upper incisor inclination determine the treatment approach: accepting or correcting the incisor relationship (Table 17.2). Traumatic overbite (palatal to upper incisors/labial to lower incisors with/without attrition; Figure 17.3) may require joint restorative/orthodontic management (Table 17.2) |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


