Biofilms
Learning objectives
■ Define the origin and components of cuticle.
■ Discuss the composition of acquired pellicle and plaque.
■ Describe the location and composition of calculus.
■ Explain why saliva is important in determining oral health.
Key terms
Cuticular protein
Disclosing solution
Hydroxyapatite
Pellicle or acquired pellicle
Plaque
Primary or developmental cuticle
Prismless zone of enamel
Reduced enamel epithelium
Salivary corpuscles
Serumal calculus
Overview
This chapter describes substances that form on the surface of the teeth and explains how they develop. Microbial biofilms are a major concern today because they are also associated with implantable medical devices. The dental plaque is composed of a biofilm. It is important that this biofilm is characterized as it exists on the surface of the body and is capable of being analyzed and characterized and treated with known agents. The primary cuticle is of cellular origin and is formed before tooth eruption. All other products originate from saliva. The primary cuticle forms the zone of junctional epithelium; the remaining epithelium is lost soon after the teeth erupt into incisal or occlusal contact. Saliva contains salivary proteins and glycoproteins that attach to enamel or exposed cementum or dentin. Saliva then deposits a thin protein coat or membrane, called a pellicle, on the surface of the tooth. The pellicle, although protective to the tooth, allows plaque to form on the surface of the tooth. This plaque is composed of bacteria and salivary proteins that will become a dense layer that gradually accumulates on the tooth’s surface if not removed. The bacteria in plaque may produce acid that can cause etching and disintegration of the tooth’s surface. This leads to the initiation of dental caries. Dental caries therefore develops in areas where brushing or washing of the tooth’s surface does not occur. In other instances, plaque may not produce acid but may become mineralized into calculus. Calculus forms by mineralization of the remaining plaque bacteria into a hydroxyapatite deposit on the enamel and exposed cementum surfaces. Continuous acquisition of calculus forms a thick deposit that should be removed, because the potential for inflammation or infection of gingival tissue could lead to destructive periodontal disease.
Cuticle
The primary or developmental cuticle is deposited on the enamel’s surface by the ameloblasts as their last function, shortly before the tooth crown erupts into the oral cavity. At this time, the formed enamel has reached a thickness of 2 to 2.5 mm over the cusps and is fully mineralized. In their final action, the ameloblasts secrete a thin, structureless protein membrane on the tooth’s surface. On the outer surface of this cuticle is the remainder of the enamel organ cells, termed the reduced enamel epithelium. This cellular membrane on the tooth’s surface includes the ameloblasts and other remnants of the enamel organ. Ameloblasts form the primary cuticle.
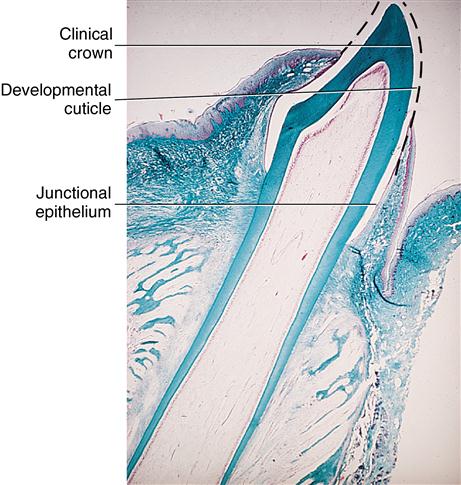
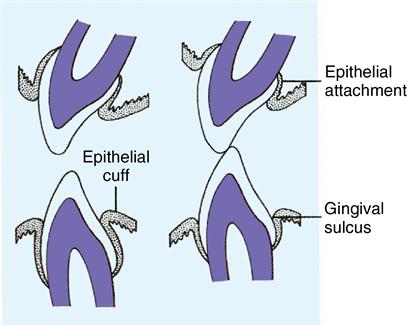
The reduced enamel epithelium is lost during eruption of the teeth in the oral cavity (Fig. 16-1). Only the developmental cuticle remains on the surface of the tooth as it erupts into occlusal function. However, this cuticle is not present long on the enamel because abrasion from contact of the opposing teeth causes it to wear away. Only that part covering the enamel in the gingival crevice remains (Fig. 16-2). This membrane serves as an attachment of the gingival junctional epithelial cells to the tooth. The sulcular epithelium is continually forming protein, which renews the gingival attachment throughout its life. Cuticular protein, which initiates attachment of the junctional epithelium to enamel, is the most important function of the primary cuticle.
Acquired pellicle
When the tooth’s surface is cleansed, salivary proteins and glycoproteins are quickly deposited with their strong attraction for the enamel surface. The resulting layer forms a thin, structureless membrane about 0.5 to 1.0 mm thick, which is in contrast to the previously formed cuticular layer. This membrane is termed the pellicle or acquired pellicle (Fig. 16-3). Although the pellicle is bacteria free when formed, bacteria rapidly attach to its surface. The pellicle covers the entire free surface of the enamel and may penetrate any convenient defect in the tooth’s surface, such as a crack, a pit, or an overhanging restoration (Fig. 16-4). Normally, surface layers of enamel rods are straight and at right angles to the tooth surface. The zone is about 30 mm thick, with the long axis of the apatite crystals oriented nearly perpendicular to the enamel surface. This area is termed the prismless zone of enamel. The acquired pellicle overlying this zone has a fine, granular appearance and is approximately 500 Å thick when viewed in ultrastructure (see Fig. 16-4). If the pellicle is lost as a result of an oral prophylaxis, it forms again in a few minutes. Although the acquired pellicle is considered protective to the enamel surface, it does provide an attachment site for bacteria, which form plaque.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses