Oral mucosa
Learning objectives
■ Describe the various types of oral mucosa including lining, masticatory, and specialized.
■ Explain the various changes in oral mucosa that occur with aging.
Key terms
Attached gingiva
Basal cell
Basal lamina
Circumvallate papilla
Col
Desmosomes
Ectopic
Eleidin
Filiform papillae
Foliate papillae
Fordyce spots
Free gingival groove
Free or marginal zone
Fungiform papillae
Hemidesmosomes
Interdental papilla
Interdental zone
Langerhans cells
Lining mucosa
Macula adherens
Masticatory mucosa
Median raphe
Melanocytes
Merkel cells
Mucogingival junction
Papillae
Rugae
Specialized mucosa
Stratum basale
Stratum corneum
Stratum granulosum
Stratum intermedium or stratum spinosum
Stratum superficiale
Supporting or sustentacular cells
Sweet, salty, sour, and bitter
Taste cells
Tonofibrils
Traction bands
Umami
Vermilion border
Overview
The structure of stratified squamous epithelium of the oral mucosa includes both the nonkeratinized lining mucosa of the cheeks, lips, soft palate, and floor of the mouth and the keratinized epithelium covering the palate and alveolar ridges. Masticatory mucosa consists of multiple layers of epithelial cells associated with the lamina dura layer, which contains blood vessels, nerve endings, and serous, mucous, or mixed glands. A third type of mucosa found on the surface of the tongue is specialized mucosa, consisting of four types of papillae, which are filiform, fungiform, foliate, and circumvallate.
Taste is associated with the latter three types of papillae, which are located on the tongue, soft palate, and pharynx. Traditionally four types of taste are regionally associated with the tongue; however, a fifth taste modality has been reported, umami. At the tip, sweet and salty tastes are perceived; sour taste is associated with the sides of the tongue; and bitter taste is at the back of the tongue. The tongue map is a traditional overview and is useful for determining broad regions of the tongue that are more sensitive to a specific taste modality and is useful for a general understanding and not for specifics.
Masticatory mucosa includes the gingiva, which is composed of the tissue surrounding the cervicals (necks) of the teeth. The gingiva consists of three areas, which are free, attached, and interdental. The free gingiva is characterized by the gingival sulcus. The attached gingiva has junctional epithelium, which binds the gingiva to the cervicals of the teeth. The interdental area is that tissue between the teeth below their contact point. The hard palate is covered by masticatory mucosa, which is firmly attached to the underlying bone.
Cells of the oral mucosa are termed keratinocytes and can be distinguished from the nonkeratinocytes, which are Langerhans cells, Merkel cells, and melanocytes. In case of inflammation, lymphocytes and leukocytes may appear in the mucosa. They are commonly found in gingival epithelium.
Four types of nerve receptors—heat, cold, pain, and touch—are located in the lips and oral cavity. They are most numerous in the lips and in the tip of the tongue. With age, the oral mucosa becomes thinner and may be lower on the cervicals of the teeth. Also, it can become less moist because of the decrease in activity of the salivary glands.
Structure of oral mucosa
The oral cavity is lined with stratified squamous epithelium, which is divided into three types of tissue (Fig. 14-1). Lining mucosa covers the floor of the mouth and the cheeks, lips, and soft palate. It does not function in mastication and therefore has little attrition. Masticatory mucosa covers the hard palate and alveolar ridges and is so named because it comes in primary contact with food during mastication. Specialized mucosa, which covers the surface of the tongue, is quite different in structure and appearance from the two previous tissues.
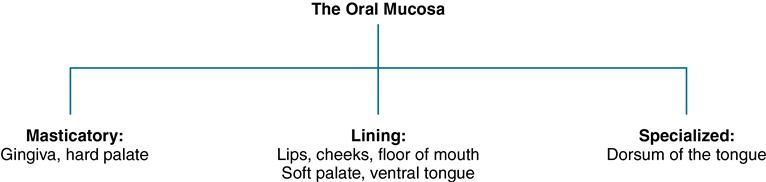
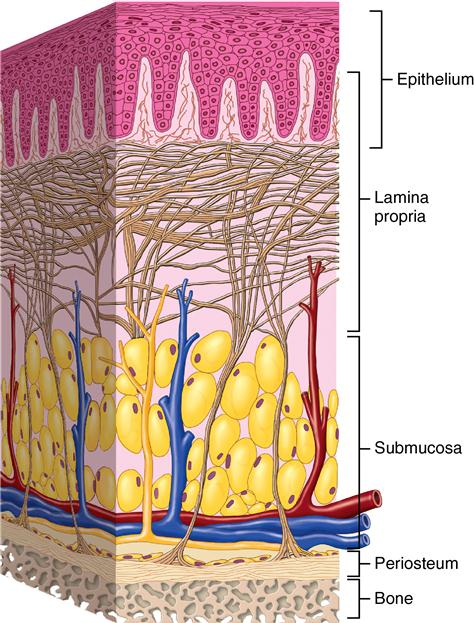
Each type of tissue has structural differences: the lining mucosa is soft, pliable, and nonkeratinized; the masticatory mucosa is keratinized, indicative of the abrasion/attrition that takes place during mastication. Specialized mucosa on the tongue surface is composed largely of cornified epithelial papillae, which function in mastication. The mucosa of the oral cavity has several features common to epithelium elsewhere in the body. One of these features is the lamina propria, the connective tissue layer immediately below the epithelium. It is composed of the papillary layer and deeper reticular layer (Fig. 14-2). In the papillary layer, the connective tissue extends into pockets in the epithelium. This increases the surface of the epithelium for contact with vascular supply and nerves. The reticular layer contains the deeper plexus of vessels and nerves supported by the connective tissue. These two layers, papillary and reticular, contribute the lamina propria or dermis. Beneath this zone is the submucosa or subcutaneous tissue (Box 14-1).
Lining mucosa
Lining mucosa is composed of a thin layer of epithelium and an underlying lamina propria. The epithelium is composed of a basal layer of cuboidal cells, termed the stratum basale. The next cell layer is called the stratum intermedium or stratum spinosum. The cells in this layer appear oval and somewhat flattened. The third or superficial layer is termed the stratum superficiale, and its cells are flattened, with many containing small oval nuclei (see Fig. 14-2). These three cell layers of the epidermis form the nonkeratinized epithelium of the oral mucosa and appear similar to the lining of the pharynx. Another component of the mucosa is the dermis or lamina propria, composed of the papillary and reticular connective tissue layers.
Lips
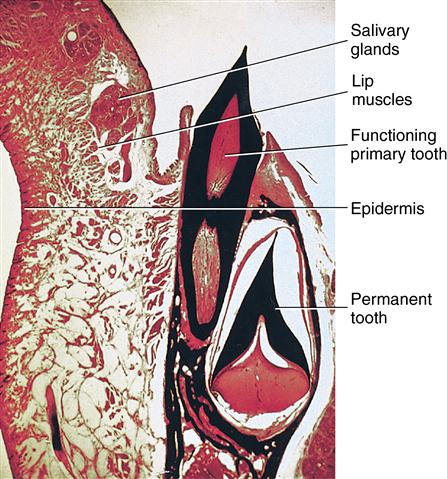
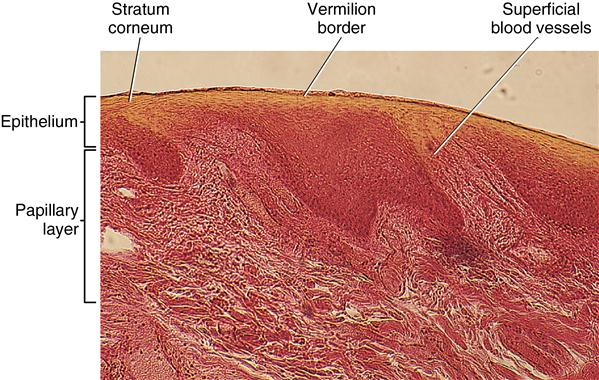
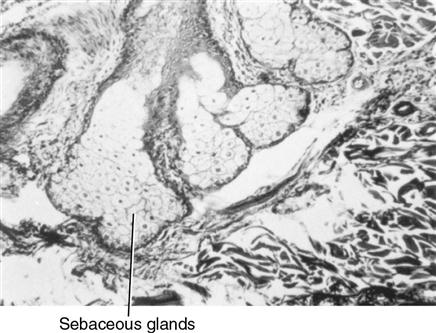
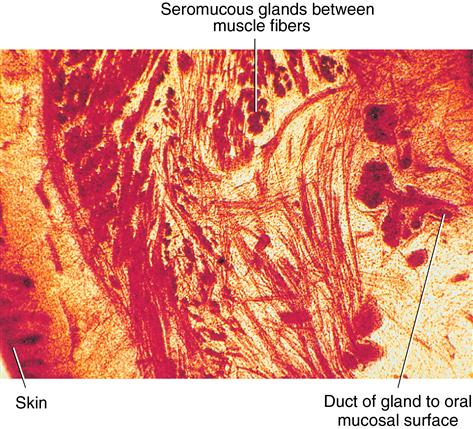
The inner oral surface of the lips is lined with moist surface, stratified squamous cells, and nonkeratinized epithelium and is associated with small, round seromucous glands of the lamina propria. These glands are part of the minor salivary glands found throughout the oral cavity. Beneath the lamina propria is the submucosa, in which fibers of the orbicularis oris muscle are located (Fig. 14-3). Nonkeratinized mucosa of the lips is distinguished by a red border known as the vermilion border. This area is at the junction between the oral mucosa and the skin of the lips, becoming modified into keratinized epithelium, which is different from skin or mucosa. There are three reasons that the vermilion border is red, including the following: the epithelium is thin; this epithelium contains eleidin, which is transparent; and the blood vessels are near the surface of the papillary layer, revealing the red blood cells’ color (Fig. 14-4). Also observable in the skin of the lips are hair follicles and their associated sebaceous glands, erector pili muscles, and sweat glands. Ectopic sebaceous glands can be seen at the angles of the mouth. They are not associated with hair follicles. These glands are known as Fordyce spots (Fig. 14-5).
Soft palate
Lining mucosa of the highly vascularized soft palate is more pink than the mucosa of the keratinized epithelium of the hard palate (Fig. 14-6). This tissue is pink because the lamina propria contains many small blood vessels. Beneath the connective tissue of the lamina propria is the submucosa, which contains muscles of the soft palate and mucous glands.
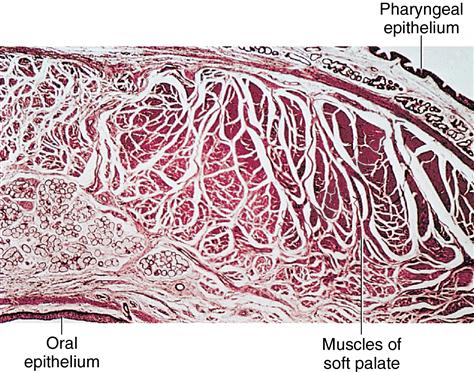
The nasal cavity is above, and respiratory epithelium covers the superior part of the soft palate. The oral cavity is below this tissue and is covered with stratified squamous epithelium. Observe the minor glands underlying the oral mucosa and muscle throughout the submucosa.
Cheeks
The mucosa of the cheeks is like that of the lips or soft palate, because each has stratified squamous epithelium that is nonkeratinized, lamina propria, and underlying submucosa. In the cheeks, however, the submucosa contains fat cells and mixed glands (seromucous) located within and between the muscle fibers. The presence of these glands and fat cells is a unique feature of the cheeks (Fig. 14-7).
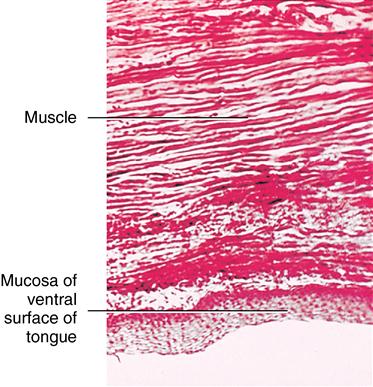
Ventral surface of the tongue
Lining mucosa also contains a lamina propria and submucosa. In the submucosa, muscle fibers are located under the surface of the tongue. The entire area exhibits dense, interlaced muscle and connective tissue fibers. Limits of the submucosa are not distinct because the submucosa continues with the deep muscles of the tongue along with connective tissue fibers (Fig. 14-8).
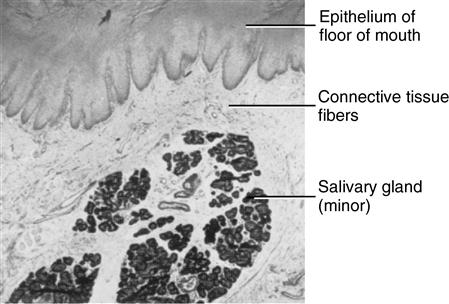
Floor of the mouth
Nonkeratinized mucous membrane covers the floor of the mouth and appears loosely attached to the lamina propria. In contrast, the adjacent undersurface of the tongue mucosa is firmly attached. In the floor of the mouth are minor salivary glands (Fig. 14-9) and the right and left major sublingual glands salivary glands, which produce a mostly mucous secretion.
Masticatory mucosa
Masticatory mucosa is the epithelium covering the gingiva and hard palate. This mucosa is thicker than the nonkeratinized mucosa with the addition of a keratinized surface of flat, cornified cells offering resistance to attrition. The basal and intermediate stratum (stratum spinosum) layers are the same as those of nonkeratinized epithelium. The granular layer (stratum granulosum) and the surface layer (stratum corneum) are the two other layers (Fig. 14-10). The cells of the basal layer are cuboidal or columnar. Their nuclei are irregularly oval and exhibit numerous mitotic figures as they undergo constant cell division. These basal cells gradually migrate to the surface of the mucosa. Fig. 14-9 shows the differences in each cell layer. The second layer, stratum spinosum, is several cells thick. These cells are oval to polygonal, and mitotic figures can be seen in this layer.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses