Traumatic Injuries to the Mandibular Condyle
The literature suggests that condylar fractures account for 17.5% to 52 % of all mandibular fractures. In most condylar fractures, direct force to the distal mandible sequentially shocks the joint area proximally.1–5
Condylar Neck Region Biomechanics
Multiple factors create condylar head displacement, including direction, magnitude, and the point of maximum force.6 Stability of the occlusion and jaw position (open versus closed) during the traumatic insult affect condylar displacement. Little or no displacement occurs in occlusion with adequate molar support; significant condylar displacement may occur with the mouth open, exposing condylar vulnerability.7
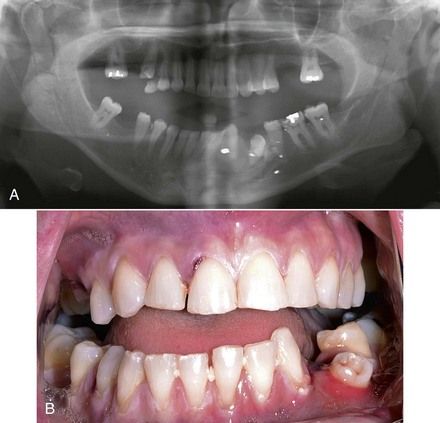
Surgeons commonly overlook condylar fractures.8 Subtle signs may mask diagnosis. On the other hand, patients may deform significantly. Patients may occlude prematurely on the ipsilateral side and open posteriorly on the contralateral side (Fig. 15-1). They will deviate toward the fracture side on opening because of disruption of lateral pterygoid forces.9 Patients with bilateral condylar fractures characteristically occlude posteriorly and open the anterior occlusion symmetrically (Fig. 15-2). Subtle findings may include limited mouth opening, limited mandibular movements, and preauricular pain.
According to a review by Zachariades et al,6 72% of condylar fractures are associated with concomitant mandibular fractures, usually parasymphyseal (Fig. 15-3). Body fractures prevail with bilateral condylar fractures, except in children.
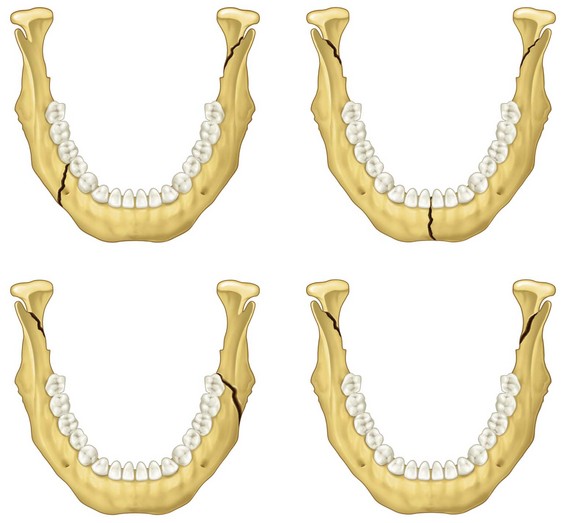
FIGURE 15-3 Condylar fracture patterns.
Concomitant facial fractures predominate with more proximal condylar fractures. The forces generated to yield coexistent facial fractures produce diacapitular (intracapsular) fractures (75%) and condylar base (subcondylar) fractures (25%).10 In isolated condylar fractures, the degree of malocclusion increases as the fracture moves distally. Malocclusion was present in only 12% of intracapsular fractures, 31 % of condylar neck fractures, and 57% of subcondylar fractures.9
Classification of Temporomandibular Joint Fractures
Temporomandibular joint (TMJ) classification schemes tend to be complex, difficult to use, and clinically irrelevant in treatment plan development.11 There are many variables to consider, including intracapsular versus extracapsular fractures, condylar fracture location (high, medium, or low), age of the patient, age of the fracture, dislocation of the condyle, simple versus comminuted, type of joint capsule injury, amount of occlusal support, ramus height shortening, and degree of fracture angulation (displacement).12,13
Condylar displacement and ramus shortening are useful determinants. Patients with displaced condylar fractures of 10 degrees or more, together with ramus height shortening of 2 mm or more, benefit from open reduction internal fixation. This is true despite the level of condylar fracture.10,13–17,24 The literature is conflicted concerning the indications for fracture repair based solely on condylar displacement; however, increased degrees of condylar displacement correspond to increased joint dysfunction and pain.19,20
Strasbourg Osteosynthesis Research Group
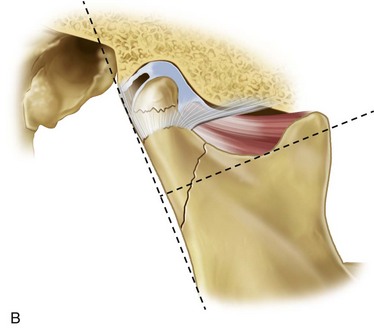
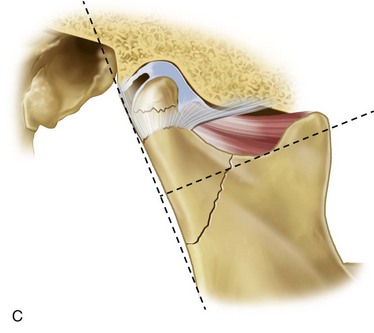
This system was developed to simplify the categorization of condylar fractures based on anatomic and clinical significance (Fig. 15-4).10,18,21,22 It may be stated as follows:
• Diacapitular fracture (through the head of the condyle). The fracture line starts in the condylar head and may extend outside of the capsule.
• Fracture of the condylar neck. More than half of the fracture is superior to an imaginary line extending from the most inferior portion of the sigmoid notch perpendicular to the tangent of the ramus (line A).
• Fracture of the condylar base. More than half of the fracture is inferior to line A.
• Displacement. Minimal displacement is defined as displacement less than 10 degrees or ramus height shortening 2 mm or less. Moderate displacement is defined as displacement of 10 to 45 degrees. Severe displacement is defined as displacement of 45 degrees or more.
Displacement refers to fracture line status. Dislocation refers to the luxation grade of the condylar head.21
Classification for Management of SUBCondylar Fractures
This system uses two proven indications, ramus height shortening and condylar displacement (coronal or sagittal plane), for open reduction and internal fixation (ORIF) and attempts to provide corresponding treatment guidelines.14,23,24
• Class 1 fractures. Minimally displaced leads to closed reduction; ramus height shortening less than 2 mm; degree of fracture displacement less than 10 degrees.
• Class 2 fractures. Moderately displaced leads to ORIF; ramus height shortening 2 to 15 mm; degree of fracture displacement 10 to 45 degrees.
• Class 3 fractures. Severely displaced leads to ORIF; ramus height shortening more than 15 mm; degree of fracture displacement more than 45 degrees.
Radiographic Evaluation of Condylar Fractures
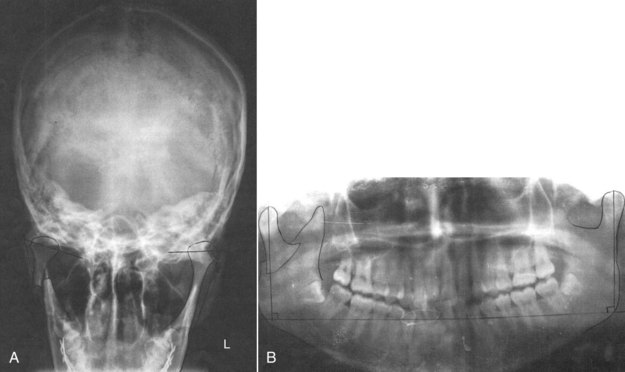
Various views may be used to evaluate these fracture.18,23,25 These include the standardized Towne’s radiograph, anterior posterior dimension (coronal position), Panorex, and medial lateral dimension (sagittal position).
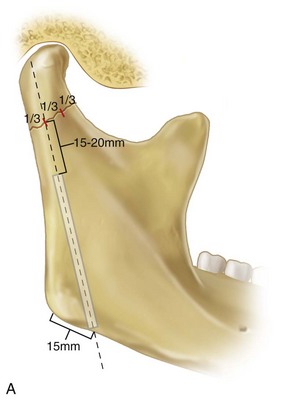
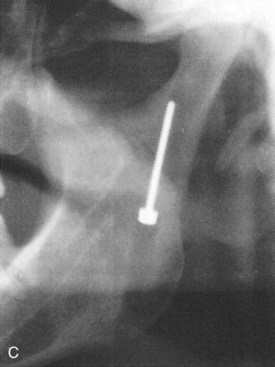
For the measurement of condylar process displacement,23,25 coronal displacement is evaluated with Towne’s radiograph (Fig 15-5A) and sagittal displacement with a panoramic radiograph.
To evaluate the loss of ramus height,18,23,25 a panoramic radiograph is used. The measurement technique is as follows (see Fig. 15-5B):
Mandibular Condylar Fractures
Indications for Reduction
There has been much disagreement about whether fractures should be treated open or closed. Social inequities, reimbursement quandaries, and surgical schedules guide choices when objective beneficial conclusions are hazy. Opening a condyle fracture is no simple task for the inexperienced or unaided; hence, a surgeon will acquiesce to an acceptable result, acquired with minimal surgical intervention. Reflecting their history and experience, there are centers where all condylar fractures are treated closed and a few where the vast majority are opened.26 Currently, without universal standards and indications, fractures are mostly opened on a case by case basis.
There are certain situations that are almost always perceived as absolute indications for ORIF of condylar fractures. Conversely, there are also clear indications for treating some condylar fractures with closed reduction. These are listed in Box 15-1. The quandary, then, is how to treat the remaining condylar fractures that fall in between the absolute indications for ORIF and the clear indications for closed reduction (CR).
Recent prospective randomized studies have compared CR with ORIF. Both CR and ORIF have been shown to be acceptable. Conclusive evidence, however, reveals that patients with ramus height shortening of 2 mm or more and condylar displacement of more than 45 degrees (severely displaced) benefit from ORIF regardless of fracture level or type of fixation performed.27,28 Patients in the open treatment group had less pain, discomfort, malocclusions, and greater range of motion in all parameters.14,18,26 The data are inconclusive concerning indications for fracture repair based solely on moderate condylar displacement (10 to 45 degrees); however, the degree of condylar displacement correlates directly with condylar dysfunction and long-term pain.19
Ellis, in 2009,29 retrospectively reviewed 332 patient cases with unilateral extracapsular condylar fractures to determine when open treatment of condylar process fractures would be meritorious. This study did not isolate fracture type or displacement of the condylar head. It was concluded that only a patient who develops a malocclusion after release from maxillomandibular fixation (MMF) need be considered for open reduction. In this study, only 1 of 332 patients developed a postoperative malocclusion.
A recent prospective, double-center study by Kokemueller et al26 has compared endoscope-assisted transoral reduction and internal fixation with CR. Inclusion criteria included unilateral condyle fractures exhibiting at least one of the following characteristics: more than 30 degrees of displacement, severe functional impairment (open bite or malocclusion), severe pain on movement, or vertical ramus shortening; high condylar fractures were excluded. Results revealed that the ORIF group was more symptom-free, with less malocclusion. The duration of MMF was shorter in the ORIF group compared with the CR group.
Treatment
Surgical Versus Nonsurgical Treatment
The surgical goals enumerated decades ago by Walker include the following five features20,33:
1. Pain-free mouth opening, with an interincisal distance beyond 40 mm
2. Good movement of the jaw in all excursive movements
ORIF and CR patients benefit from early mobilization and extensive rehabilitation, generally over a period of 6 to 12 weeks.34 Immediately after the traumatic injury, tissues are not yet tethered down by scar formation. Early mobilization of the joint after injury reduces permanent joint hypomobility.35,36 Rehabilitation with a target maximal incisal opening reaching more than 40 mm before 12 weeks is fundamental and ideal before 6 weeks. Once an MIO of more than 40 mm is reached, it should be maintained during the next few months while the soft and bony tissues are maturing.
Active (the patient does the work) and passive (bite sticks, external forces) all have their place. Usually, we recommend active physiotherapy during the first 6 weeks, especially if other fractures are present, and only passive forms when obstacles are encountered (Box 15-2).
Surgical Approaches to the Condylar and Subcondylar Regions
All open approaches have three common aspects to their success:
1. The ramus must be distracted.
2. The proximal condyle must be controlled and manipulated.
3. The fracture must be anatomically reduced and plated with more than one screw on the proximal segment.
Submandibular Approach.
This is also known as the Risdon approach.12,37–42
Advantages.
These include the ability to distract the mandibular ramus and direct access of the gonial angle.
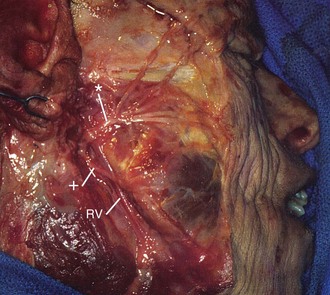
Pertinent Anatomy
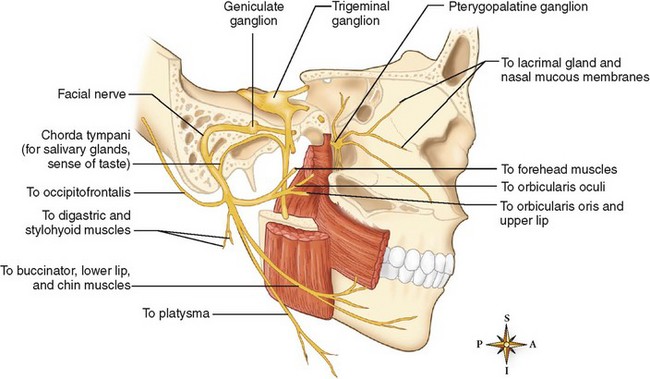
Marginal Mandibular Branch of the Facial Nerve.
Posterior to the facial artery, the marginal branch passes inferior to the border of the mandible in 19% to 56% of specimens studied (Fig. 15-6).37,38 The maximum inferior extent of the mandibular branch is 1.2 cm below the mandible. Anterior to the facial artery, the marginal branch passes inferior to the border of the mandible in 0% to 6% of specimens studied. It passes immediately deep to the superficial layer of the deep cervical fascia, which is immediately deep to the platysma, and superficial to the facial vessels.
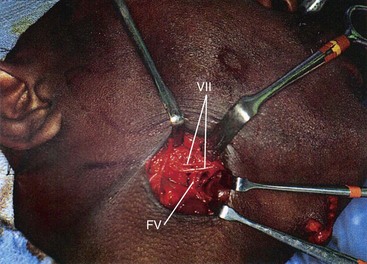
This passes through or along the superficial surface of the submandibular gland and approximates the inferior border of the mandible just anterior to the pterygomasseteric sling (Fig. 15-7). The artery then rounds the inferior border of the mandible and becomes superficial to the mandible. Generally, the anterior facial vein runs posterior to the facial artery above the inferior border of the mandible. The facial vein is just deep to the platysma.
Surgical Technique
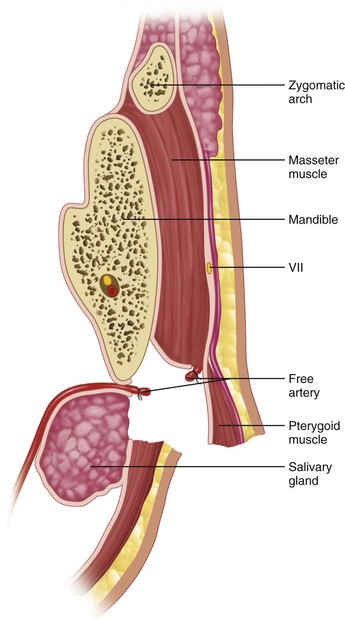
FIGURE 15-8 Anatomic landmarks of submandibular dissection.
• Through the platysma. Undermine and sharply dissect, being careful to stay superficial to the superficial layer of the deep cervical fascia.
• From the platysma to pterygomasseteric sling. Make a small incision through the superficial layer of the deep cervical fascia at the level of the skin incision (1.5 to 2 cm inferior to the mandible). The facial artery and vein may be retracted anteriorly or divided and ligated if necessary. Continue the dissection superiorly until the pterygomasseteric sling is encountered.
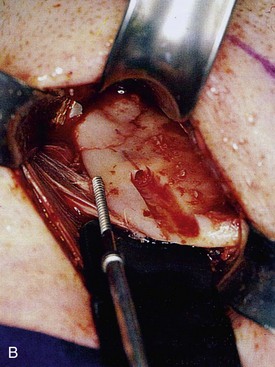
• Division of the pterygomasseteric sling. The use of a nerve stimulator is necessary through this portion of the dissection, with the absence of muscle relaxants, to identify the branches of the facial nerve. Sharply incise the pterygomasseteric sling with a scalpel along the inferior border of the mandible. Use a periosteal elevator to expose the ramus up to the level of the TMJ capsule and coronoid process. A sigmoid notch retractor is helpful in fully exposing the ramus.
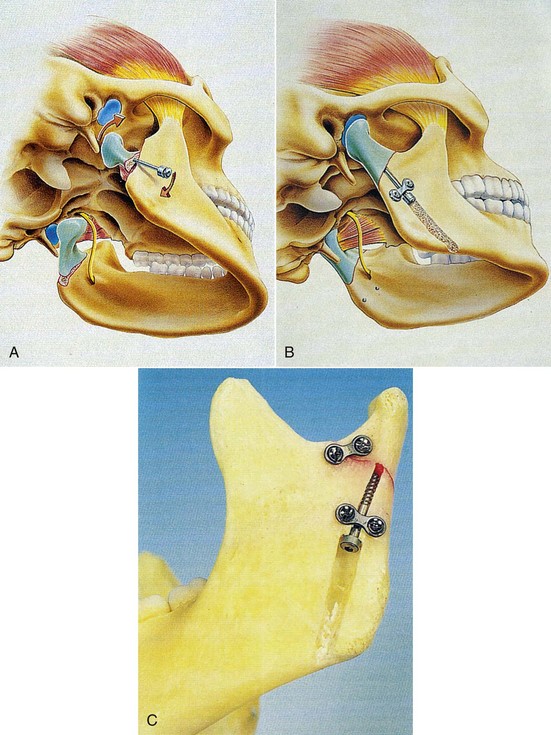
Osteosynthesis: Axial Anchor Screw
Visibility and Reduction.
Distract the distal segment using ligature wire at the gonial angle (see Fig. 15-9). Use a sigmoid notch retractor and condylar neck retractor to reflect soft tissues. Stabilize and reduce the proximal segment using a curved hemostat.
Direct Fixation.
Place a groove in the lateral cortex approximately 1 cm anterior to the posterior border and 1.5 to 2 cm inferior to the fracture line (see Fig. 15-9). A centering instrument is used to place the screw hole; a 2-mm drill is used to drill the pilot hole to the fracture line. The drill guide is placed and a 1.5-mm drill is used to penetrate beyond the fracture line into the proximal segment an additional 1 to 2 cm. Measure length and place and tighten titanium screw with biconcave washer.
Indirect Fixation.
This alternative method is indicated when the proximal condylar fragment is difficult to reduce (Fig. 15-10). First, place the positioning screw into the proximal segment. Then reduce the proximal segment using a biomechanically advantageous screw. Place a groove through the lateral cortex to the fracture line. Lock the screw into place using a two-hole miniplate locked against the proximal screw shaft.
Retromandibular Approach
Indications.
This is used for any fracture that is large enough to be reduced and stabilized by ORIF using plates and screws.37,38
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses