15 The Temporomandibular Joints, Teeth, and Muscles, and Their Functions
The masticatory system is comprised of joints, muscles, teeth, and nerves that are integrated in the act of mastication. However, that is not to say that other functions and parafunctions are not performed by the components of this system (e.g., speech, yawning, singing, bruxism, clenching, and so on). In addition, when disorders occur in any component of the system, symptoms may be reflected to adjacent and associated structures (e.g., temporomandibular joint and muscle disorders) with pain (myalgia). Dysfunction of one or more of the masticatory muscles (e.g., lateral pterygoid muscle) can lead to pain and dysfunction of muscles not usually considered to be masticatory muscles (e.g., neck muscles), and such conditions are sometimes referred to as craniomandibular disorders. Also to be considered in the diagnosis of orofacial pain are possible associations between the symptoms of toothache, headache, and joint and muscle disorders. In addition, the role of mandibular movements and movements related to yawning and opening of the eustachian tubes in subjective hearing problems (stuffiness of the ears) is considered.1 This chapter provides the necessary anatomical and functional basis for further study into disorders of the masticatory system.
Temporomandibular Articulation
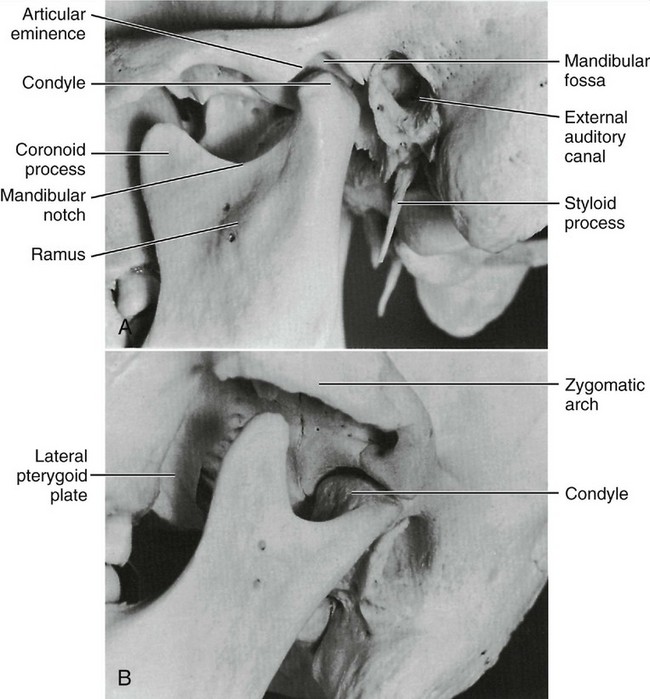
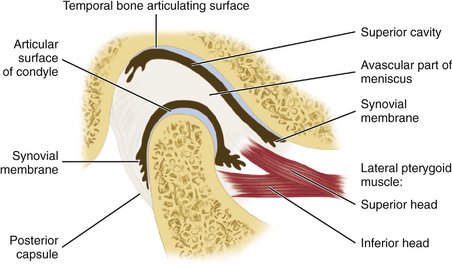
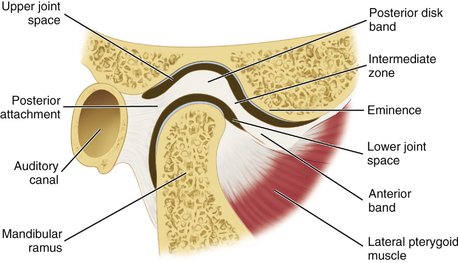
The temporomandibular joint (TMJ) is an example of ginglymoarthrodial articulation, and its movements are a combination of gliding movements and a loose hinge movement. The osseous portions of the joint are the anterior portion of the mandibular (glenoid) fossa and articular eminence of the temporal bone, and the condyloid process of the mandible (Figure 15-1). The functional surfaces of both the condyle and the eminence, along with the anterior aspects of the condyle, are the functional articular surfaces, not the mandibular fossa. Interposed between the condyle and temporal bone is the articular disk. It consists of dense collagenous connective tissue that, in the central area, is relatively avascular, hyalinized, and devoid of nerves (Figure 15-2). The disk is not seen on radiographs, but the bony structures in one plane can be viewed by a transcranial projection (Figure 15-3).
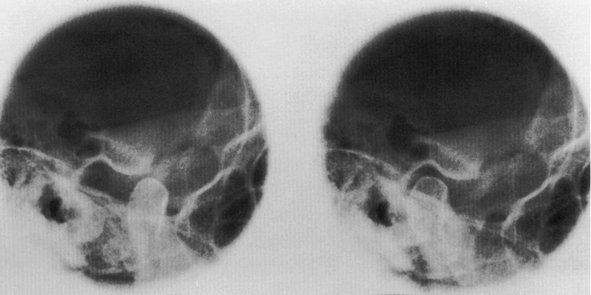
Figure 15-3 Radiograph showing the temporomandibular joint in open (left) and closed (right) position of mandible.
MANDIBULAR FOSSA
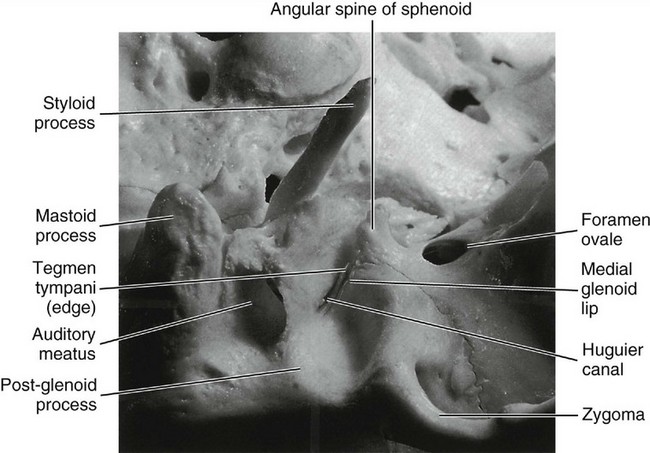
The mandibular fossa is an oval or oblong depression in the temporal bone just anterior to the auditory canal (Figure 15-4). It is bounded anteriorly by the eminentia articularis (articular eminence), externally by the middle root of the zygoma and the auditory process, and posteriorly by the tympanic plate of the petrous portion of this bone (see Figure 14-1). The shape of the mandibular fossa conforms to some extent, although not exactly, to the posterior and superior surfaces of the condyloid process of the mandible.
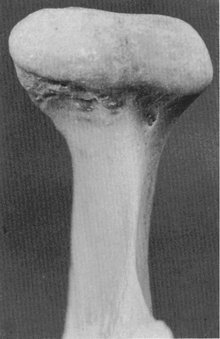
CONDYLOID PROCESS
The condyloid process of the mandible is convex on all bearing surfaces, although somewhat flattened posteriorly, and its knoblike form is wider lateromedially than anteroposteriorly (Figure 15-5). It is perhaps two and one half times as wide in one direction as in the other. Although the development of the condyle differs in individuals, the functional design remains the same. The long axes of the condyles are in a lateral plane, and at first sight, they seem to be out of alignment, because the long axes, if the lines were prolonged, would meet at a point anterior to the foramen magnum at an angle of approximately 135 degrees. The condyle is perpendicular to the ascending ramus of the mandible (see Figure 15-5).
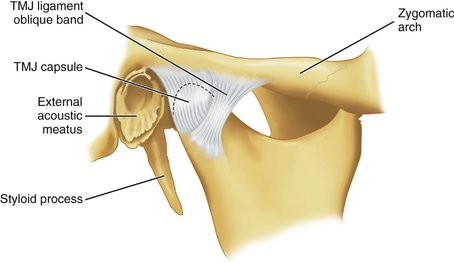
JOINT CAPSULE
The TMJ is enclosed in a capsule (Figure 15-6) that is attached at the borders of the articulating surfaces of the mandibular fossa and eminence of the temporal bone and to the neck of the mandible. The anterolateral side of the capsule may be thickened to form a band referred to as the temporomandibular ligament. It is not always so thickened, but when clearly distinguishable as a ligament, it appears to originate on the zygomatic arch and to pass backward to attach on the lateral and/or distal surfaces of the neck of the mandible.
The capsule consists of an internal synovial layer and an outer fibrous layer containing veins, nerves, and collagen fibers. The innervation for the capsule arises from the trigeminal nerve, and several kinds of receptors have been described, including free nerve endings.2 The vascular supply arises from the maxillary, temporal, and masseteric arteries.
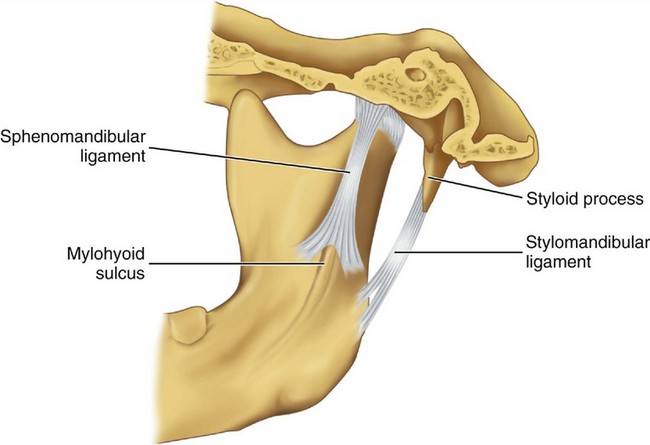
MANDIBULAR LIGAMENTS
Accessory ligaments, including the stylomandibular and sphenomandibular ligaments, are considered a part of the masticatory apparatus (Figure 15-7). These ligaments do not have a direct relationship with mandibular articulation, although they may stabilize the articular system during jaw movements.
The sphenomandibular ligament arises from the angular spine of the sphenoid bone and from the petrotympanic fissures and ends broadly at the lingula of the mandible. In some instances, a continuation of ligament fibers is evident through the petrotympanic fissure via the Huguier canal (see Figure 15-4) to the middle ear, where they attach to the malleus.
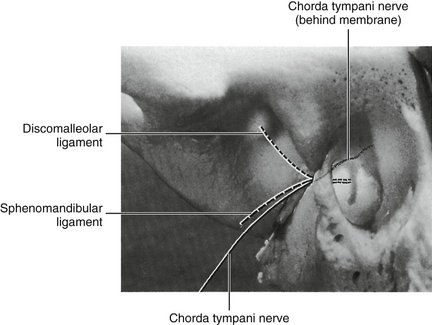
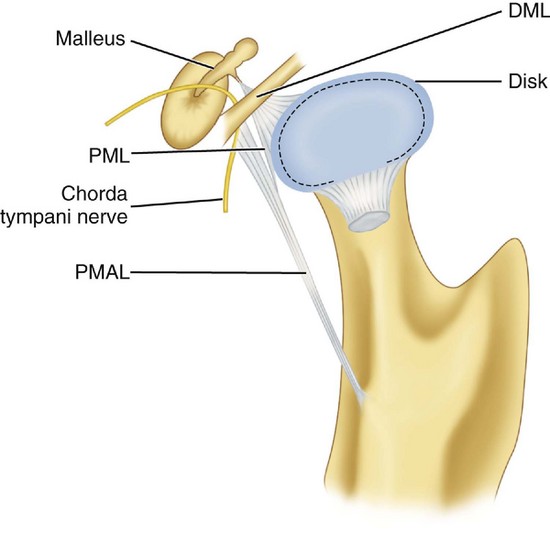
Otomandibular ligaments connect the middle ear and the TMJ. These small ligaments, the discomalleolar and tympanomandibular (sphenomandibular), have been described as connecting the malleus to the TMJ disk and to the sphenomandibular ligaments (Figures 15-8 and 15-9). The role of these ligaments as causal factors in subjective TMJ-mediated auditory symptoms remains to be substantiated.3
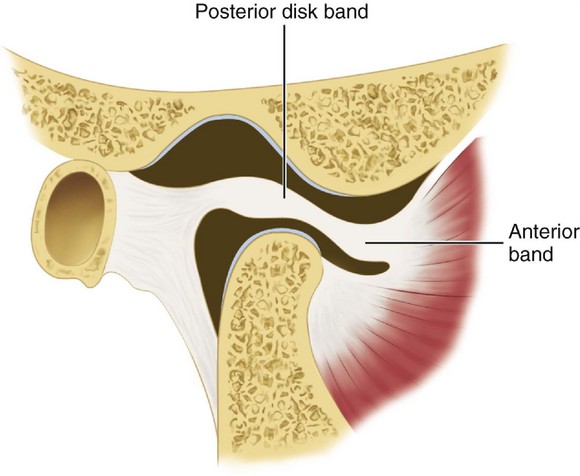
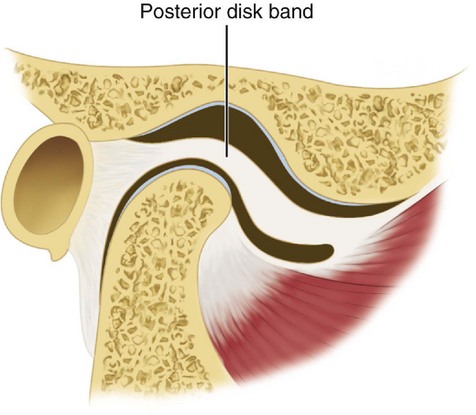
ARTICULAR DISK
The interarticular disk (see Figure 15-2) consists of fibrous tissue shaped to accommodate the shape of the condyle and concavity of the mandibular fossa. Thicker anterior and posterior bands and a thin central zone are evident4 (Figure 15-10). The superior and inferior heads of the lateral pterygoid muscle both insert into the pterygoid fovea of the mandible with a part of the superior head inserting into the disk and capsule. The disk divides the articulating surfaces into upper and lower compartments that provide for smooth gliding function. As the jaw opens and moves forward, the intermediate zone of the disk is interposed between the anterior slope of the articular eminence and the condyle, and the bilaminar region of the disk fills in the mandibular fossa (Figure 15-11). The upper head of the lateral pterygoid muscle, which does not appear to be active during mandibular opening movement, stabilizes the relationship of the disk to the eminence. Continued anterior displacement of the disk (Figure 15-12) with the posterior band in an anterior position with the jaw closed can prevent the jaw from opening normally (i.e., locking). The cause of disk derangement is multifactorial but may include acute and chronic trauma.
MANDIBULAR POSITIONS
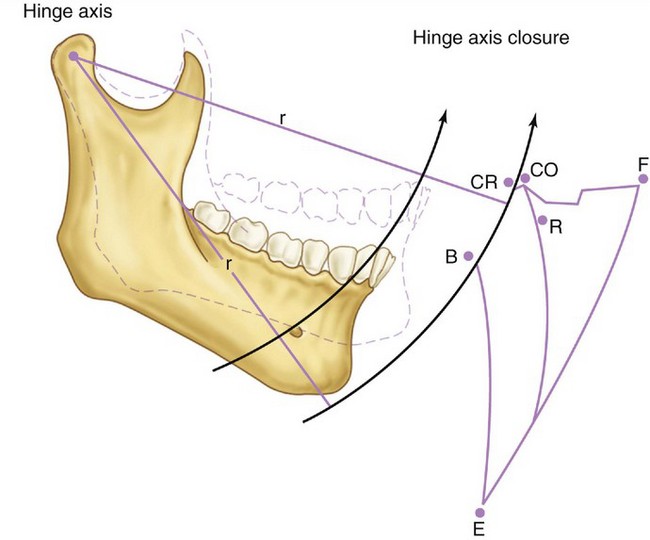
Basic jaw positions are usually described as centric occlusion, intercuspal position, centric relation, retruded contact position, and rest position of the mandible.5 Centric occlusion or intercuspal position is defined as maximum intercuspation of the teeth. Centric relation is a position of the mandible (or path of opening and closing without translation of the condyles) in which the condyles are in their uppermost position in the mandibular fossae and related anteriorly to the distal slope of the articular eminence (see Figure 16-44). Because the mandible appears to rotate around a transverse axis through the condyle in centric relation movement, guidance of the jaw by the clinician (see Figure 16-42) in opening and closing movements that do not have translation is referred to as hinge axis movement (Figure 15-13). In this position, the condyles are considered to be in the terminal hinge position. Under physiological conditions of the masticatory system, centric relation is used to transfer the position of the mandible (in relation to the maxilla) to an articulator.
In the natural dentition, centric occlusion is, in the majority of people, anterior to centric relation contact on the average by approximately 1 mm.6 Centric occlusion (or acquired or habitual centric as it is sometimes called) is a tooth-determined position, whereas centric relation is a jaw-to-jaw relation determined by the condyles in the fossae. Closure into occlusion occurs usually anterior to centric relation; however, a coincidence of centric relation contact and the intercuspal position is evident in about 10% of the population.
MANDIBULAR MOVEMENTS
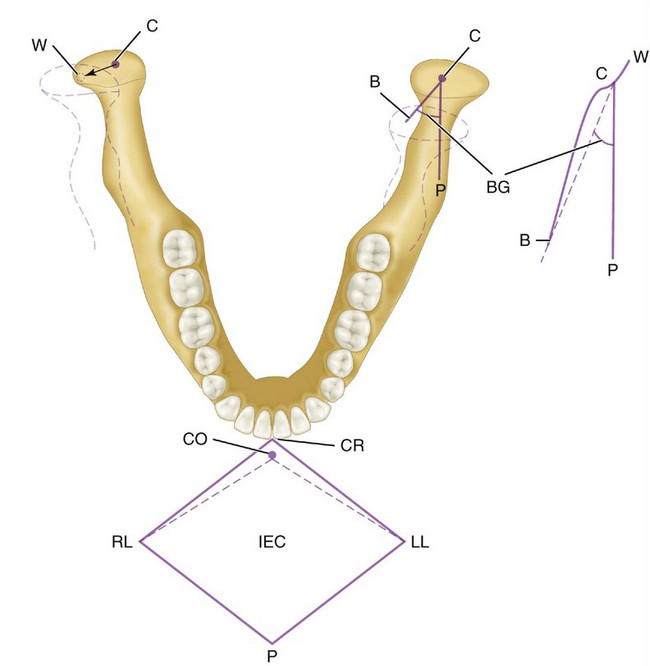
In lateral movements (Figure 15-14), the condyle appears to rotate with a slight lateral shift in the direction of the movement. This movement is called the Bennett movement and may have both immediate and progressive components. By the use of recording equipment such as a pantograph or kinesiograph, it is possible to record mandibular movements in relation to a particular plane of reference (e.g., sagittal, horizontal, or frontal planes). If a point (the incisive point) located between the incisal edges of the two mandibular central incisors is tracked during maximal lateral, protrusive, retrusive, and wide opening movements, such movements are seen to take place within a border or envelope of movements.6 Functional and parafunctional movements occur within these borders. However, most functional movements such as those associated with mastication occur chiefly around centric. Border movements in the horizontal plane are shown in Figure 15-14.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses