The Second Stage of Comprehensive Treatment
Correction of Molar Relationship and Space Closure
At the beginning of the second stage of treatment, the teeth should be well aligned, and any excessive or reverse curve of Spee should have been eliminated. The objectives of this stage of treatment are to correct molar and buccal segment relationships to provide normal occlusion in the anteroposterior plane of space, close extraction spaces or residual spaces in the arches, and correct excessive or negative overjet. This is possible only if the jaw relationships are reasonably correct, which means that orthognathic surgery must be considered for the most severe problems. Indications for surgical treatment and the orthodontist–surgeon interaction are discussed in Chapter 19.
Correction of Molar Relationship
Differential Growth in Adolescent Class II Treatment
The use of extraoral force or functional appliances to influence jaw growth is discussed in some detail in Chapter 13. The different timing of skeletal growth in males and females must be kept in mind when this approach is used. During adolescence, the mandible tends to grow forward more than the maxilla, providing an opportunity to improve a skeletal Class II jaw relationship. Girls mature considerably earlier than boys and are often beyond the peak of the adolescent growth spurt before the full permanent dentition is available and comprehensive orthodontic treatment can begin. Boys, who mature more slowly and have a more prolonged period of adolescent growth, are much more likely to have a clinically useful amount of anteroposterior growth during comprehensive treatment in the early permanent dentition.
When either extraoral force (headgear) or a functional appliance is used to modify growth in Class II patients, a favorable response includes both restraint of maxillary growth and differential forward mandibular growth. In skeletally immature patients with a permanent dentition, there is nothing wrong with a first phase of functional appliance treatment, even though the permanent teeth have erupted, and then a fixed appliance to obtain detailed occlusal results, but headgear is more compatible with the fixed appliances needed for comprehensive treatment. A removable functional appliance alone is unlikely to provide a satisfactory result in the early permanent dentition, and it will have to be modified or discontinued when the fixed appliance treatment begins. Many clinicians would like to believe that Class II elastics (or fixed springs that have the same effect) can influence growth, as well as move teeth. Unfortunately, the evidence indicates that growth modification in adolescent patients is unlikely with elastics or flexible spring devices.1,2 In an adolescent in the early permanent dentition, a rigidly coupled fixed functional appliance like the Herbst appliance effectively corrects Class II molar relationships (with varying combinations of differential growth and forward displacement of mandibular teeth), but headgear can be quite effective in a cooperative patient and does not introduce a Class II elastics effect.
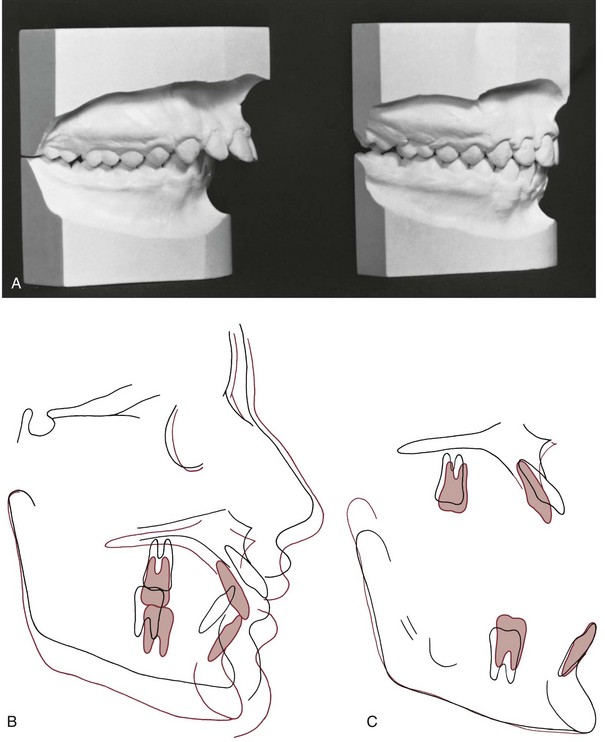
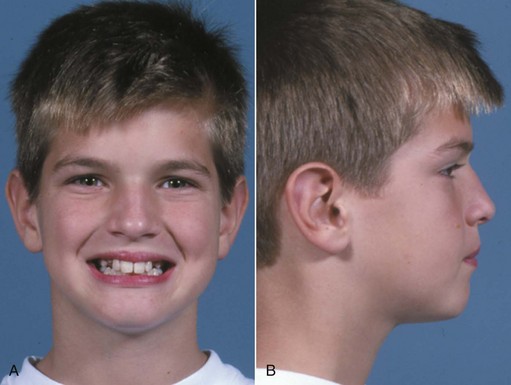
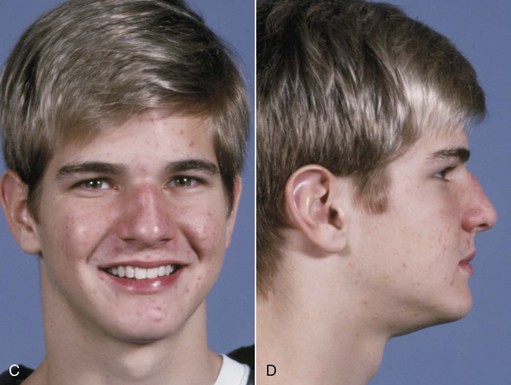
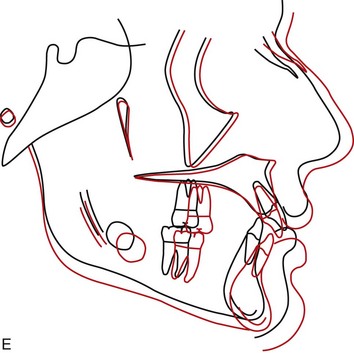
An ideal patient for headgear in the early permanent dentition is a 12- to 14-year-old boy with a Class II problem, whose skeletal maturity is somewhat behind his stage of dental development, and who has good growth potential (Figure 15-1). Boys at age 13, it must be remembered, are on the average at the same stage of maturation as girls at 11, and significant skeletal growth is almost always continuing. On the other hand, girls at age 13 are, on the average, at the same developmental stage as boys at 15, and by this time, clinically useful changes in jaw relationship from growth guidance are unlikely.
Although the main purpose of headgear is growth modification, some tooth movement in all three planes of space inevitably accompanies it when the extraoral force is delivered to the teeth. With headgear for Class II correction, when there is good vertical growth and the maxillary molars are allowed to elongate, the maxillary teeth erupt downward and backward, and spaces may open up in the maxillary arch. Even though the extraoral force is applied against the first molar, it is unusual for space to develop between the first molar and second premolar. Instead, the second and, to a lesser degree, the first premolars follow the molars. The result is often a space distal to the canines, along with a partial reduction of overjet as the jaw relationship improves (Figure 15-2).
In the early permanent dentition, space opening within the maxillary arch rarely occurs when a Herbst appliance or some of its modern variants (see Figure 10-7) are used. Bonding the teeth that are available (canines and incisors in both arches, maxillary premolars) allows alignment and stabilization of the lower incisors while molar correction is occurring and facilitates the transition to a regular fixed appliance, which usually occurs after about 12 months of Herbst treatment. With a lingual appliance (now increasingly used in adolescents as well as adults), a Herbst appliance also can be an effective way to correct a Class II molar relationship. The precisely fitting lingual archwire controls the inclination of the lower incisors quite well.3
Class II Correction by Distal Movement of Upper Molars
The concept of “distal driving” the maxillary posterior teeth has a long orthodontic history.4 After early cephalometric studies in the 1940s showed that little or no distal movement of upper molars was produced by the Class II elastic treatment of that era, headgear was reintroduced as a means of moving the upper molars back. Palatal anchorage also has been used to create distal movement of upper molars and to create a space into which the anterior teeth can be retracted, and skeletal anchorage (bone screws or bone anchors) now offers a more effective way to accomplish distal movement.
Although the modern methods discussed below have improved the situation, Class II correction by distal movement of upper molars has definite limits that are important to understand and respect. With headgear, it is now clear that significant distal positioning of the upper posterior teeth relative to the maxilla occurs primarily in patients who have vertical growth and elongation of the maxillary teeth (see Figure 15-1). Without this, it is difficult to produce more than 2 to 3 mm of distal movement of the upper molars, unless the upper second molars are extracted (see later). Appliances based on palatal anchorage are somewhat more successful in moving upper molars back, but complete Class II correction by this mechanism is unlikely. With skeletal anchorage above the roots of the teeth, 4 to 6 mm of distal movement is quite possible, but moving molars back requires space behind them, and second molar extraction may be required for major distalization. If second molars are to be distalized, early removal of third molars is advised—otherwise they may become significantly impacted and difficult to extract.
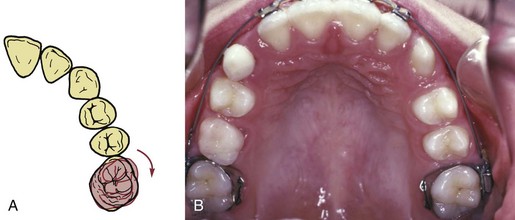
Molar Rotation as a Factor in Distalization
In patients with mild-to-moderate skeletal Class II malocclusion, the upper molars are likely to have rotated mesially around the lingual root, and merely correcting the rotation changes the occlusal relationship in a Class I direction (see Figure 15-2). This can be done with a transpalatal lingual arch, an auxiliary labial arch, or the inner bow of a facebow. Sometimes upper molars are so mesially rotated that it is difficult or impossible to insert a facebow until the rotation has been partially corrected with a more flexible appliance (such as a heavy labial arch, typically 36 mil steel, inserted into the headgear tubes and tied over an initial alignment archwire). Correction of rotated maxillary first molars is the first step in Class II treatment of almost every type.
Anchorage Systems for Distal Movement of Molars
Palatal Anchorage: The relative stability of the anterior palate, both the soft tissue rugae and the cortical bone beneath them, is one possibility for obtaining this additional anchorage. Although removable appliances contact the palate, they are not effective in moving molars back, probably because they do not fit well enough. A fixed appliance that stabilizes the premolars and includes a plastic pad contacting the rugae is needed. Fortunately, most patients tolerate this with minimal problems, but contacting the palatal tissue has the potential to cause significant tissue irritation, to the point that the appliance has to be removed.
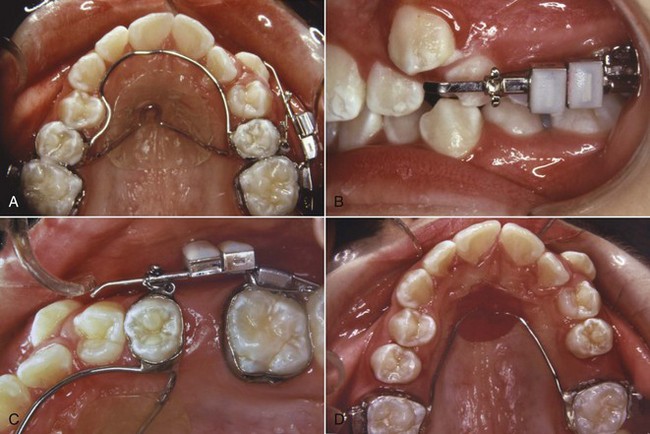
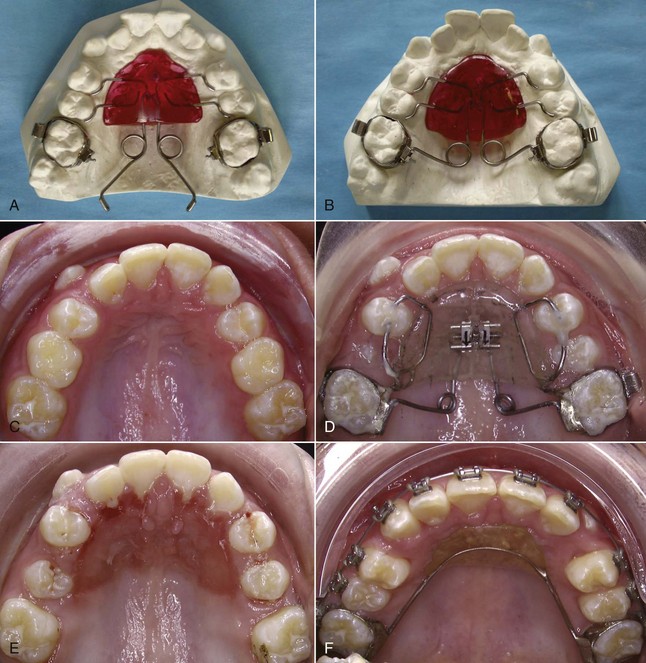
Once palatal anchorage has been established, there are several possibilities for generating the molar distalizing force. Austenite nickel–titanium (A-NiTi) coil springs compressed against the molars (from an anterior anchorage unit) produce an effective and nearly constant force system for the distal movement. Magnets in repulsion also can be used (Figure 15-3), but the amount of force changes markedly as tooth movement occurs. A-NiTi springs have the additional advantage of being less bulky and usually are a better choice. The pendulum appliance (Figure 15-4) uses beta-titanium (beta-Ti) springs that extend from the palatal acrylic and fit into lingual sheaths on the molar tube, which gives greater control of these teeth
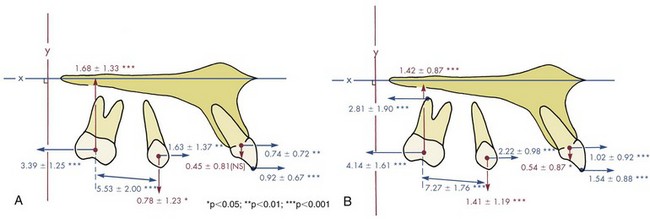
In a small but well-characterized sample of patients who were treated to a super-Class I molar relationship with the pendulum appliance activated to produce 200 to 250 gm, Byloff et al found that molar movement averaged just over 1 mm/month (1.02 ± 0.68), with a considerable degree of distal tipping of the crown and an elevation of the molar (Figure 15-5, A).5 As one would expect, despite the contact of the appliance with the palate, the premolars and incisors were tipped anteriorly, but the molar moved distally 2 to 3 times as far as the anchor teeth. When the appliance was modified to minimize distal tipping of the molar, the distal movement of the molar crown was similar, but greater distal movement of the roots was obtained at the cost of increased treatment time and some additional forward movement of the incisors (Figure 15-5, B).6
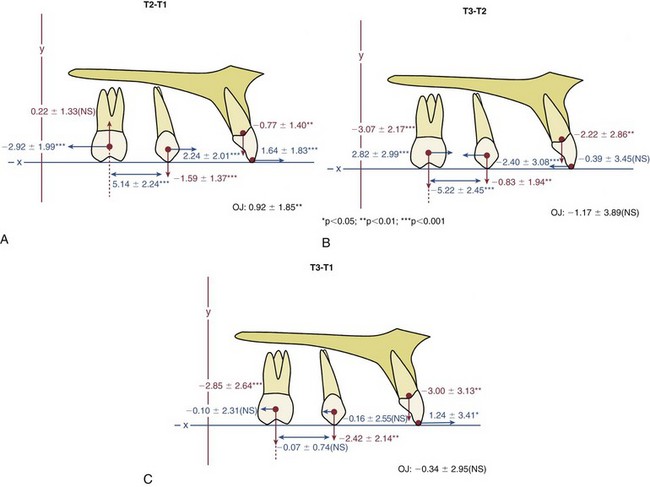
However the molars were moved distally, they must be held there while the other teeth are then retracted to correct the overjet (see Figure 15-3). It is one thing to move molars back, and something else to maintain them in that position. Simply leaving the distalization appliance in place for 2 to 3 months leads to distal movement of the premolars by stretched gingival fibers, but as soon as the original premolar-based lingual arch and palatal pad are removed, a new lingual arch and pad from the distalized molars must be placed. Even so, especially if the molar tipped distally, it will tip mesially again as the space closes. Placing a tipback in the distalizing springs will keep the molar more upright and minimize relapse, but this increases the extrusive tendency, so as with headgear, the most successful molar distalization with the pendulum appliance occurs in patients who have vertical growth during their treatment. Even so, data show that on the average, much of the original distalization is lost during the second phase of treatment with a complete fixed appliance (Figure 15-6).
Headgear or Class II Elastics: The problem with headgear for this type of tooth movement always has been that force of moderate intensity with long duration is needed, while headgear tends to supply relatively high force with only medium duration even in cooperative patients. Unless second molars are extracted (see below), significant distal movement of first molars (>2 mm) with headgear occurs only when the molar is extruded simultaneously, which is acceptable in a patient with substantial growth in height of the ramus, but otherwise leads to unfavorable downward-backward rotation of the mandible. High-pull headgear is not very effective in distalizing molars.
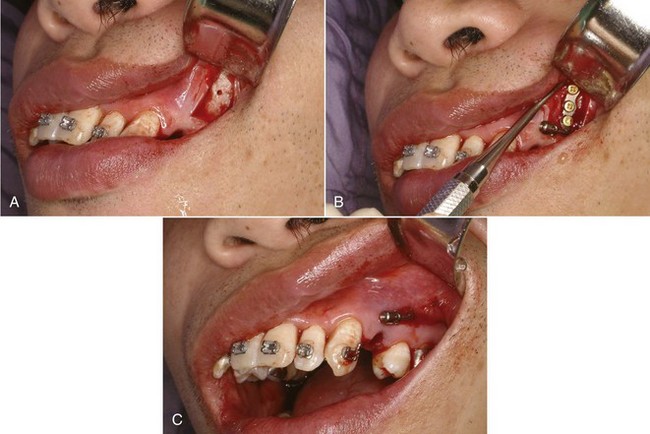
Skeletal Anchorage: At this point, the advantage of skeletal anchorage for distalization of molars is so great that it is rapidly replacing the previous methods. With miniplates or a long bone screw at the base of the zygomatic arch (Figure 15-7)7 or bone screws in the palate to stabilize a lingual arch with springs for distalization,8 all the maxillary teeth can be moved back simultaneously (see Figure 18-47). Alveolar bone screws also are a possibility, but if they are between tooth roots, they block mesiodistal changes in tooth position, so using them for distalization requires changing screw position during treatment. With skeletal anchorage of any type, a fixed appliance with NiTi coil springs provides the best force system for distal movement.
Distalization of First Molars After Second Molar Extraction
With skeletal anchorage, greater distalization of first and second molars is possible, but extraction of the upper second molars should be considered if the third molars are reasonably well formed. The same 75% to 80% chance that third molars would be satisfactory replacements for the second molars presumably would apply with use of skeletal anchorage, as it did with headgear for distalization.9
Occasionally, unilateral molar distalization is indicated, typically when a unilateral Class II malocclusion is present and there is a dental midline discrepancy. Extraction of one second molar facilitates this treatment, and the third molar usually replaces the missing second molar quite satisfactorily (Figure 15-8). Unilateral cervical headgear can be used for this treatment plan, but skeletal anchorage is definitely preferred now.
Differential Anteroposterior Tooth Movement Using Extraction Spaces
There are two reasons for extracting teeth in orthodontics, as discussed in detail in Chapter 7: (1) to provide space to align crowded incisors without creating excessive protrusion and (2) to allow camouflage of moderate Class II or Class III jaw relationships when correction by growth modification is not possible. A patient who is both Class II (or III) and crowded is a particular problem because the same space cannot be used for both purposes. The more extraction space is required for alignment, the less is available for differential movement in camouflage, and vice versa.
Class II Camouflage by Extraction of Upper First Premolars
In the late 1980s, it was claimed by some dentists that extraction of upper first premolars would lead to later temporomandibular dysfunction (TMD) problems. The theory, to the extent that the proponents of this claim had one, was that retracting the upper incisors would inevitably lead to incisor interferences, and this would cause TMD. The claim was never supported by any evidence, and research data have refuted it.10,11 It is important to limit first premolar extraction for camouflage of Class II malocclusion to the appropriate patients and not to retract the incisors too much, but if this is done, it can be an excellent treatment method.
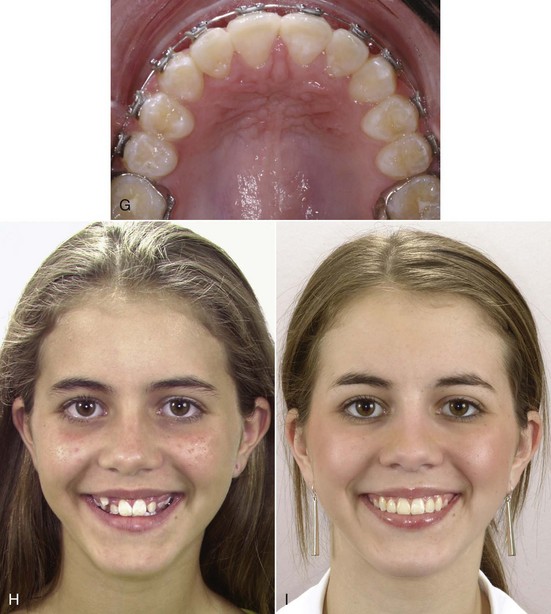
With this approach, the objective is to maintain the existing Class II molar relationship, closing the first premolar extraction space largely by retracting the protruding incisor teeth (Figure 15-9). Anchorage must be reinforced, but one method, Class II elastics from the lower arch, is specifically contraindicated unless the lower incisors need to be moved forward (which rarely is the case). The remaining possibilities are extraoral force to the first molars, a stabilizing lingual arch, retraction of the maxillary anterior segment with extraoral force directly against these teeth, or skeletal anchorage.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses