Treatment of Skeletal Problems in Children and Preadolescents
PRINCIPLES IN TIMING OF GROWTH MODIFICATION
1 Timing in Relation to the Amount of Growth Remaining
TREATMENT OF TRANSVERSE MAXILLARY CONSTRICTION
TREATMENT OF CLASS III PROBLEMS
TREATMENT OF CLASS II PROBLEMS
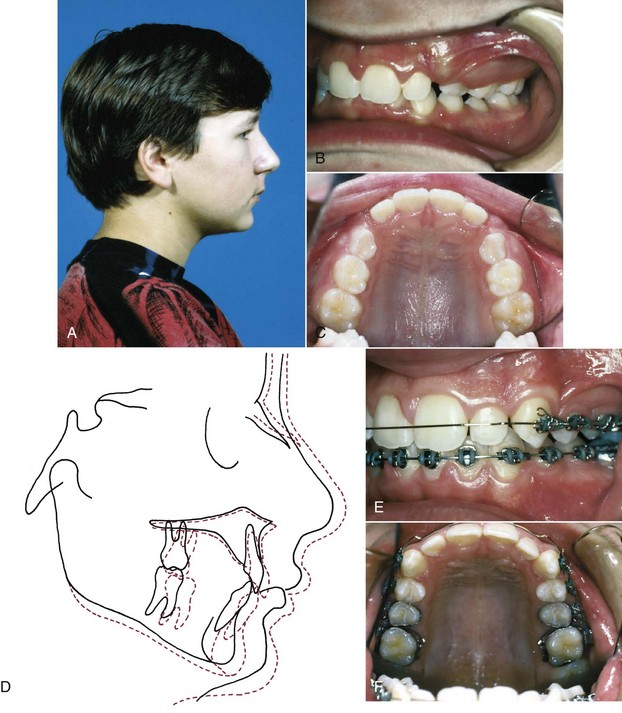
Whenever a jaw discrepancy exists, the ideal solution is to correct it by modifying the child’s facial growth, so that the skeletal problem is corrected by more or less growth of one jaw than the other (Figure 13-1). Unfortunately, such an ideal solution is not always possible, but growth modification for skeletal problems can be successful. Treatment planning for skeletal problems and what has been learned about the optimum timing of treatment have been discussed extensively in Chapter 7. This chapter briefly reviews the issues in treatment timing that were presented previously but focuses on clinical treatment aimed at growth modification. Usually this is accomplished by applying forces directly to the teeth and secondarily and indirectly to the skeletal structures, instead of applying direct pressure to the bones. Tooth movement, in addition to any changes in skeletal relationships, is unavoidable. It is possible now to apply force directly against the bone by using temporary implants, miniplates, or bone screws (see Chapter 10). This approach is likely to be used more and more in the future because the dental changes that accompany growth modification often (but not always) are undesirable. Excessive tooth movement, whether it results from a weakness in the treatment plan, poor biomechanical control, or poor compliance, can cause growth modification to be incomplete and unsuccessful.
Principles in Timing of Growth Modification
Timing in Relation to the Amount of Growth Remaining
It now is clear that a child with a jaw discrepancy can benefit from treatment during the preadolescent years if impaired esthetics and the resultant social problems are substantial. Another indication for treatment is a dental and skeletal profile highly susceptible to trauma like the increased overjet and protrusive incisors that often accompany Class II relationships (Figure 13-2). The data are clear that these individuals encounter more dental trauma.1 The type and extent of trauma is highly variable, and it has been difficult to document prevention of injuries with early treatment to reduce overjet because it is often accomplished following or concurrent with the period of most injury prevalence. Nonetheless, it is probably prudent to consider reducing overjet for the most accident-prone children. For each patient, the benefits of early treatment must be considered against the risk and cost of prolonging the total treatment period.
Different Timing for Different Planes of Space
Vertical facial growth is the last to stop. Interestingly, this growth has been detected in both males and females into the third decade. Vertical growth control is exceptionally difficult due to the extraordinary length of the growth period (see Chapters 3 and 4). So different timing for different problems is important. Palatal expansion is seemingly more urgent in earlier years, anteroposterior growth modification is more a midgrowth activity, and vertical control requires a later approach if it can be accomplished.
How one evaluates the growth stages and timing appears to make a difference, and different methods have advocates and detractors, based on the assessment approach. The cervical vertebral maturation staging (CVMS) method related to mandibular growth changes that is described in Chapter 3 may yield different results than timing based on hand–wrist radiographic estimation of skeletal maturation. In fact, differences of opinion exist on the appropriateness of each technique and even on how to apply the CVMS method. It may be that the most reliable, valid, and critical use of the CVMS method is differentiating the premandibular from postmandibular growth peak phases. Given the reduced radiation (because the images are available as part of the cephalometric radiograph), simplicity in learning, and excellent accuracy of the CVMS method among nonradiologist growth assessors like dentists and orthodontists, this method has a strong appeal and is certain to evolve.
Treatment of Transverse Maxillary Constriction
Skeletal maxillary constriction is distinguished by a narrow palatal vault (see Figure 6-71). It can be corrected by opening the midpalatal suture, which widens the roof of the mouth and the floor of the nose. This transverse expansion corrects the posterior crossbite that almost always is present (in fact, a narrow maxilla accompanied by a narrow mandible and normal occlusion should not be considered a problem just because the jaw widths are below the population mean). The expansion sometimes moves the maxilla forward a little (but is about as likely to lead to backward movement),2 increases space in the arch,3 and repositions underlying permanent tooth buds as they move along with the bone in which they are embedded. Palatal expansion can be done at any time prior to the end of the adolescent growth spurt. The major reasons for doing it sooner are to eliminate mandibular shifts on closure, provide more space for the erupting maxillary teeth, lessen dental arch distortion and potential tooth abrasion from interferences of anterior teeth, and reduce the possibility of mandibular skeletal asymmetry.4 The procedure is easiest when the midpalatal suture is not fused or has only minor initial bridging, so that extensive microfracturing is not needed to separate the palatal halves (i.e., when the expansion is done before adolescence).
Palatal Expansion in the Primary and Early Mixed Dentition
Because less force is needed to open the suture in younger children, it is relatively easy to obtain palatal expansion. In the early mixed dentition, all three types of expansion appliances produce both skeletal and dental changes.5 Despite that, the three approaches are not equally sensible to use.
Lingual arches of the W-arch and quad-helix designs (see Chapter 12) have been demonstrated to open the midpalatal suture in young patients (Figure 13-3). These appliances generally deliver a few hundred grams of force and provide slow expansion. They are relatively clean and reasonably effective, producing a mix of skeletal and dental change that approximates one-third skeletal and two-thirds dental change.2
In young children, in comparison with an expansion lingual arch, a fixed jackscrew appliance has two major disadvantages. First, it is more bulky and more difficult to place and remove. The patient inevitably has problems cleaning it, which lead to soft tissue irritation, and either the patient or parent must activate the appliance. Second, an appliance of this type can be activated rapidly, which in young children is a disadvantage, not an advantage. Rapid expansion should not be done in a young child. There is a risk of distortion of facial structures with rapid expansion (see Figure 7-8), and there is no evidence that rapid movement and high forces produce better or more stable expansion.
On balance, slow expansion with an active lingual arch is the preferred approach to maxillary constriction in young children in the primary and early mixed dentitions. A fixed jackscrew appliance is an acceptable alternative if activated carefully and slowly. It appears that anteroposterior dental changes in terms of overjet are not consistently correlated with maxillary expansion.6
Palatal Expansion in the Late Mixed Dentition
With increasing age, the midpalatal suture becomes more and more tightly interdigitated; however, in most individuals, it remains possible to obtain significant increments in maxillary width up to the end of the adolescent growth spurt (age 15 to 18). Expansion in adolescents is discussed in some detail in Chapter 14.
Even in the late mixed dentition, sutural expansion often requires placing a relatively heavy force directed across the suture to move the halves of the maxilla apart. A fixed jackscrew appliance (either banded or bonded) is necessary (Figure 13-4). As many teeth as possible should be included in the anchorage unit. In the late mixed dentition, root resorption of primary molars may have reached the point that these teeth offer little resistance, and it may be wise to wait for eruption of the first premolars before beginning expansion.
Although some studies have reported increases in vertical facial height with maxillary expansion, long-term evidence indicates this change is transitory.7 A bonded appliance that covers the occlusal surface of the posterior teeth may be a better choice for a preadolescent child with a long-face tendency because it produces less mandibular rotation than a banded appliance, but for younger patients this is not totally clear.8 Perhaps the best summary is that the older the patient when maxillary expansion is done, the less likely it is that vertical changes will be recovered by subsequent growth.
Rapid or Slow Expansion?
In the late mixed dentition, either rapid or slow expansion is clinically acceptable. As we have reviewed in some detail in Chapter 7, it now appears that slower activation of the expansion appliance (at the rate of about 1 mm/week) provides approximately the same ultimate result over a 10- to 12-week period as rapid expansion, with less trauma to the teeth and bones (see Figure 7-9).
Rapid expansion typically is done with two turns daily of the jackscrew (0.5 mm activation per day). This creates 10 to 20 pounds of pressure across the suture—enough to create microfractures of interdigitating bone spicules. When a screw is the activating device, the force is transmitted immediately to the teeth and then to the suture. Sometimes, a large coil spring is incorporated along with the screw, which modulates the amount of force, depending on the length and stiffness of the spring (Figure 13-5). The suture opens wider and faster anteriorly because closure begins in the posterior area of the midpalatal suture and the forces are transmitted to adjacent posterior structures.9 With rapid or semirapid expansion (one turn per day), a diastema usually appears between the central incisors as the bones separate in this area (Figure 13-6). When expansion has been completed, a 3-month period of retention with the appliance in place is recommended. After the 3-month retention period, the fixed appliance can be removed, but a removable retainer that covers the palate is often needed as further insurance against early relapse (Figure 13-7). A relatively heavy, expanded maxillary archwire provides retention and support if further treatment is being accomplished immediately. If not, a transpalatal lingual arch or a large expanded auxiliary wire (36 or 40 mil) in the headgear tubes will help maintain expansion while using a more flexible wire in the brackets.
Slow activation of the expansion appliance at the rate of 1 mm/week, which produces about 2 pounds of pressure in a mixed dentition child, opens the suture at a rate that is close to the maximum speed of bone formation. The suture is not obviously pulled apart on radiographs, and no midline diastema appears, but both skeletal and dental changes occur. After 10 to 12 weeks, approximately the same amounts of skeletal and dental expansion are present that were seen at the same time with rapid expansion. When bonded slow and rapid palatal expanders in early adolescents were compared, the major difference was greater expansion across the canines in the rapid expansion group. This translated into a predicted greater arch perimeter change but similar opening of the suture posteriorly.10 So by using slow palatal expansion (one turn every other day) in a typical fixed expansion appliance or by using a spring to produce about 2 pounds of force, effective expansion with minimal disruption of the suture can be achieved for a late mixed dentition child.
This really brings us to the question of early slower expansion or later rapid expansion as choices. Two studies that demonstrate age-appropriate approaches are instructive. One, with patients who averaged 8 years 10 months at the start, used a bonded acrylic splint and a semirapid approach of 0.25 mm expansion per day.11 The other, with patients averaging 12 years 2 months at the start, used a Haas-type rapid palatal expansion (RPE) turned twice for 0.5 mm expansion per day of treatment.12 Both followed the expansion with retention and ultimately the patients had full treatment without further purposeful expansion. At the long-term evaluation points (19 years 9 months and 20 years 5 months, respectively), the expansion across the molars and canines and the increase in arch perimeter were quite similar and seem to indicate equivalent long-term results.
Clinical Management of Palatal Expansion Devices
Most traditional palate expansion devices use bands for retention on permanent first molars and first premolars if possible. During the late mixed dentition years, the first premolars often are not fully erupted and are difficult to band. If the primary second molars are firm, they can be banded along with the permanent first molars. Alternatively, only the permanent first molars can be banded. With this approach, the appliance is generally extended anteriorly, contacting the other posterior primary and erupting permanent teeth near their gingival margins. This will provide similar posterior expansion, but less anterior changes.13 Expanders with hinged designs can differentially expand the anterior or posterior portions of the arch. For some patients, this may be an advantage (Figure 13-8). After crossbite correction is completed, band removal can be difficult because the teeth are mobile and sensitive. In those cases, sectioning the bands is appropriate.
An alternative approach is to use a bonded palatal expander (see Figure 13-4, B). Because there is no band fitting, the appliance is easier to place for both the patient and doctor, and during treatment it is manipulated like any other RPE appliance. Removal of this appliance is accomplished with a band remover engaged under a facial or lingual margin to flex the appliance and break the bond. In addition, the appliance usually needs to be sectioned or portions of the occlusal plastic removed for a direct purchase on the teeth so the band remover can effectively lift and separate the plastic from the teeth. Complete removal of the bonding agent (typically a filled resin that will adhere to etched tooth surfaces and to the appliance) can be laborious, so using only an adequate amount is crucial, but inadequate resin will lead to excessive leakage onto the nonbonded surfaces, which can result in decalcification or appliance loss. For these reasons, some clinicians use glass ionomer cement for retention. The strength of the material usually is adequate, and the short-term fluoride release may be beneficial.
Treatment of Class III Problems
Anteroposterior and Vertical Maxillary Deficiency
FR-III Functional Appliance
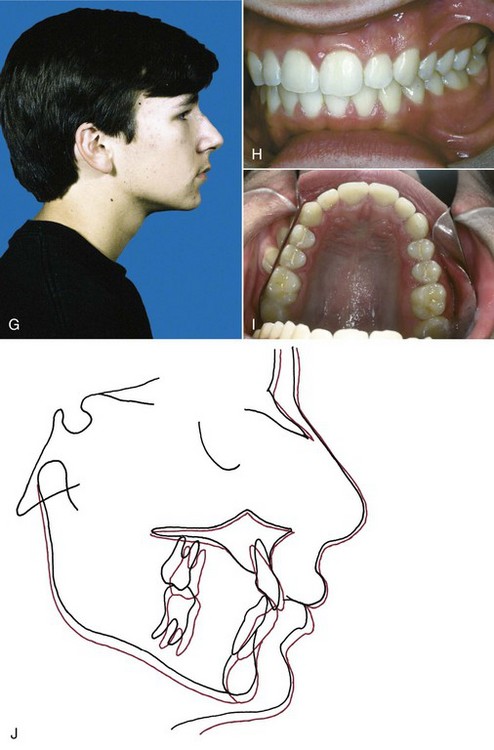
The FR-III appliance (Figure 13-9) is made with the mandible positioned posteriorly and rotated open and with pads to stretch the upper lip forward. In theory, the lip pads stretch the periosteum in a way that stimulates forward growth of the maxilla. In a review of cases selected from Frankel’s archives, Levin et al14 reported that in patients with Class III skeletal and dental relationships and good compliance who wore the FR-III appliance full time for an average of 2.5 years and then part time in retention for 3 years, there was significantly enhanced change over controls in maxillary size and position and improved mandibular position combined with more lingual lower incisor bodily position so that the patients had more overjet. This held up at the long-term follow-up over 6 years after active treatment.
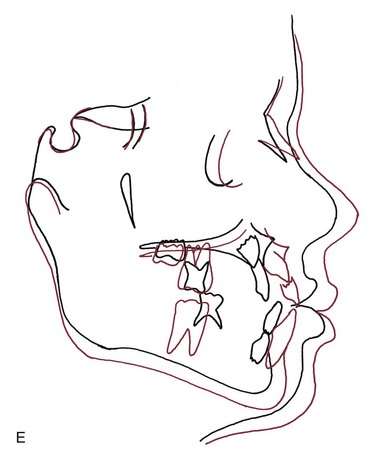
The available data from most other studies, however, indicate little true forward movement of the upper jaw.15 Instead, most of the improvement is from dental changes. The appliance allows the maxillary molars to erupt and move mesially while holding the lower molars in place vertically and anteroposteriorly and tips the maxillary anterior teeth facially and retracts the mandibular anterior teeth (Figure 13-10). Rotation of the occlusal plane as the upper molars erupt more than the lowers also contributes to a change from a Class III to a Class I molar relationship (Figure 13-11). In addition, if a functional appliance of any type rotates the chin down and back, the Class III relationship will improve because of the mandibular rotation, not an effect on the maxilla. In short, functional appliance treatment, even with the use of upper lip pads, has little or no effect on maxillary deficiency and, if considered, should be used only on extremely mild cases. If this appliance is used, there are long treatment and retention periods that require excellent compliance to maintain limited changes.
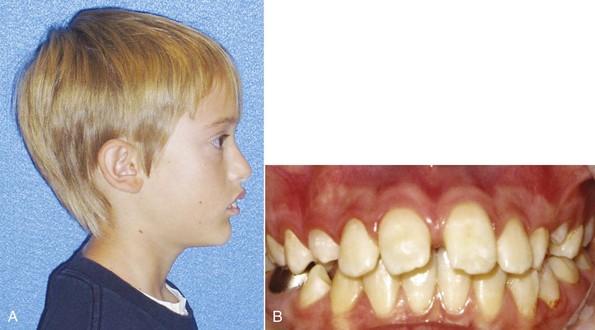
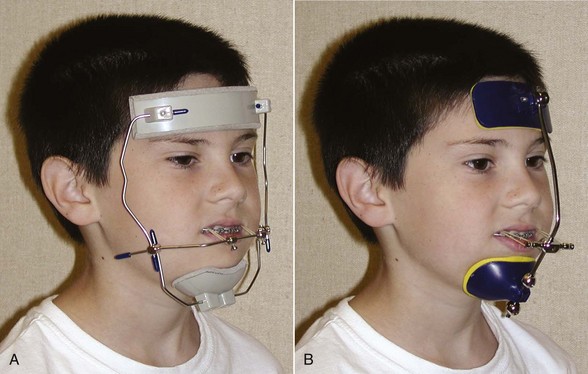
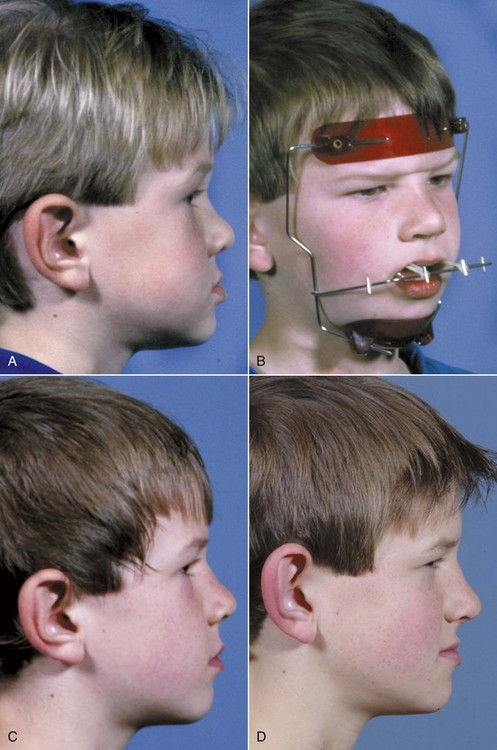
Reverse-Pull Headgear (Facemask)
After Delaire’s demonstration that a facemask attached to a maxillary splint could move the maxilla forward by inducing growth at the maxillary sutures, but only if it was done at an early age, this approach to maxillary deficiency became popular in the late twentieth century (Figure 13-12). The age of the patient is a critical variable. It is easier and more effective to move the maxilla forward at younger ages. Although some recent reports indicate that anteroposterior changes can be produced up to the beginning of adolescence, the chance of true skeletal change appears to decline beyond age 8, and the chance of clinical success begins to decline at age 10 to 11.16
When force is applied to the teeth for transmission to the sutures, tooth movement in addition to skeletal change is inevitable. Facemask treatment is most suited for children with minor-to-moderate skeletal problems, so that the teeth are within several millimeters of each other when they have the correct axial inclination. This type of treatment also is best used in children who have true maxillary problems, but some evidence indicates that the effects on mandibular growth during treatment go beyond simply changes caused by clockwise rotation of the mandible.17
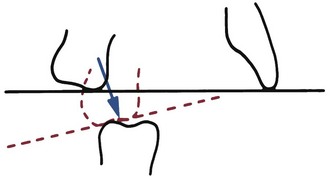
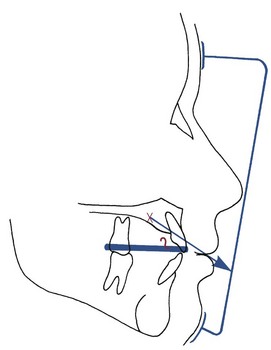
Generally, it is better to defer maxillary protraction until the permanent first molars and incisors have erupted. The molars can be included in the anchorage unit and the inclination of the incisors can be controlled to affect the overjet. Many clinicians use protraction with a facemask following or simultaneously with palatal expansion, but a randomized clinical trial has shown that simultaneous palatal expansion makes no difference in the amount of anteroposterior skeletal change.18 If the maxilla is narrow, palatal expansion is quite compatible with maxillary protraction and the expansion device is an effective splint; there is no reason, however, to expand the maxilla just to improve the protraction. Whatever the method of attachment (Figure 13-13), the appliance must have hooks for attachment to the facemask that are located in the canine–primary molar area above the occlusal plane. This places the force vector nearer the purported center of resistance of the maxilla and limits maxillary rotation (Figure 13-14).
For most young children, a facemask is as acceptable as conventional headgear. Contouring an adjustable facemask for a comfortable fit on the forehead is not difficult for most children. There are a variety of designs (see Figure 13-12).
Backward displacement of the mandibular teeth and forward displacement of the maxillary teeth also typically occur in response to this type of treatment (Figure 13-15).19 As children come closer to adolescence, mandibular rotation and displacement of maxillary teeth—not forward movement of the maxilla—are the major components of the treatment result.
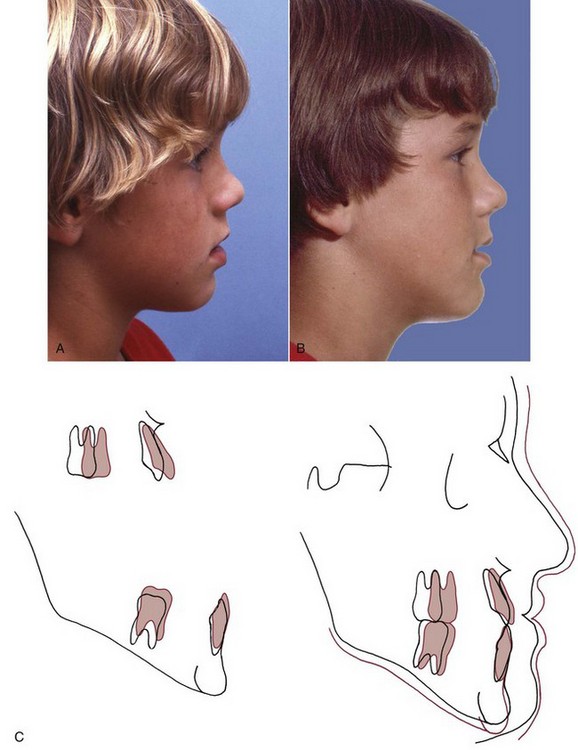
Application of Skeletal Anchorage
Clearly, a major negative side effect of maxillary protraction is maxillary dental movement that detracts from the skeletal change. Before bone screws and miniplates became available, Shapiro and Kokich deliberately ankylosed primary canines so they could be used as “natural implants.”20 With traction against a maxillary arch stabilized by these teeth, they were able to demonstrate approximately 3 mm of maxillary protraction in 1 year, with minimal dental change. If a child with maxillary retrusion has spontaneous ankylosis of primary molars, a splint can be fabricated to take advantage of these teeth as implants and gain the same biomechanical advantage.
For more routine use in clinical practice, it appears that the effects of treatment to change the deficient maxillary position can be magnified in one of two ways. First, the facemask can be applied to miniplates at the base of the zygomatic arch21 or in the anterior maxilla.22 With anchors above the incisors, 400 gm of force per side, and use of the facemask for a minimum of 16 hours per day, Sar et al22 reported 0.45 mm per month of anterior maxillary movement (compared to 0.24 mm with conventional facemask) without rotation of the maxilla. For patients approaching adolescence (i.e., about age 11 and old enough for good retention of bone screws), this appears to be promising.
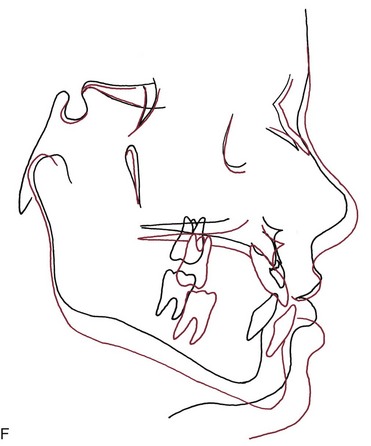
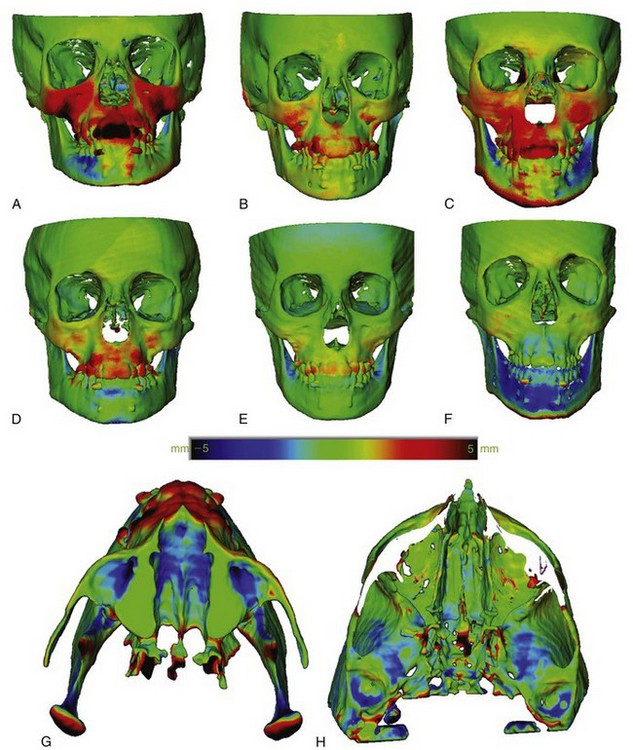
Alternatively, bone-supported miniplates can be placed bilaterally in the maxilla and the mandible, so that interarch force from Class III elastics is delivered to the jaws rather than the teeth (Figure 13-16).23 Three-dimensional (3-D) imaging of patients treated in this way has shown a variety of interesting responses (Figure 13-17) that include forward movement of the maxilla at a higher level than has been observed previously and displacement or remodeling in the temporomandibular (TM) fossae. In a sequence of 25 consecutive children treated in this way with full-time elastics delivering approximately 150 gm per side (about 5 ounces), the variety of changes seen in the 3-D images are summarized in Figure 13-18. More than 2 mm maxillary protraction was noted in 14 (56%) of the 25 patients.
This approach has two advantages: (1) it is clearly more effective than a facemask to a maxillary splint24 and also appears to produce more skeletal change than has been reported with facemasks to anterior miniplates and (2) wearing an extraoral appliance is not necessary and nearly full-time application of the force can be obtained. Compared to facemasks attached to a maxillary splint, it has the disadvantage of requiring surgical application and removal of the miniplates by a surgeon trained to do this, although this is not major surgery. Alveolar bone screws with Class III elastics would be simpler to place and remove than miniplates, but both the lower density of the bone in preadolescents and avoiding damage to unerupted permanent teeth pose substantial problems with their use (see Chapter 10). Miniplates attached to basal bone can be used at age 10-6 or 11. The minimum age for alveolar bone screws for this application appears to be approximately age 12, probably too late for an optimal skeletal effect.
Summary
There is no doubt that maxillary protraction at an early age usually produces clinical improvement in a Class III patient. Important concerns are the extent to which this will be maintained long-term and the chance that orthognathic surgery eventually will be necessary despite the early treatment. The answer to these issues, of course, requires recall 8 to 10 years after the initial treatment was completed. Three recent studies now show essentially the same thing: that 25% to 30% of their facemask patients ended up in anterior crossbite after adolescent growth and that the majority of these would require surgery for correction.25
Mandibular Excess
Functional Appliances in Treatment of Excessive Mandibular Growth
Functional appliances for patients with excessive mandibular growth make no pretense of restraining mandibular growth. They are designed to rotate the mandible down and back and to guide the eruption of the teeth so that the upper posterior teeth erupt down and forward while eruption of lower teeth is restrained. This rotates the occlusal plane in the direction that favors correction of a Class III molar relationship (see Figure 13-10). These appliances also tip the mandibular incisors lingually and the maxillary incisors facially, introducing an element of dental camouflage for the skeletal discrepancy. The only difference from a functional appliance for a maxillary deficiency patient is the absence of lip pads.
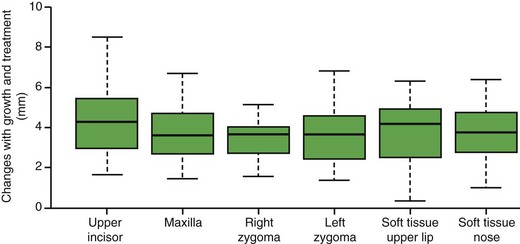
Chin-Cup Appliances: Restraint of Mandibular Growth?
In theory, extraoral force directed against the mandibular condyle would restrain growth at that location, but there is little or no evidence that this occurs in humans (see Chapter 7). What chin-cup therapy does accomplish is a change in the direction of mandibular growth, rotating the chin down and back, which makes it less prominent but increases anterior face height. The data seem to indicate a transitory restraint of growth that is likely to be overwhelmed by subsequent growth.26 In essence, the treatment becomes a trade-off between decreasing the anteroposterior prominence of the chin and increasing face height. In addition, lingual tipping of the lower incisors occurs as a result of the pressure of the appliance on the lower lip and dentition (Figure 13-19), which often is undesirable.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses