Early Stages of Development
Late Fetal Development and Birth
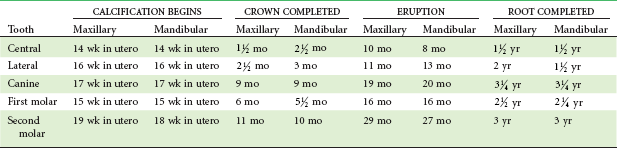
By the third trimester of intrauterine life, the human fetus weighs approximately 1000 gm and though far from ready for life outside the protective intrauterine environment, can often survive premature birth. During the last 3 months of intrauterine life, continued rapid growth results in a tripling of body mass to about 3000 gm. Dental development, which begins in the third month, proceeds rapidly thereafter (Table 3-1). Development of all primary teeth and the permanent first molars starts well before birth.
Although the proportion of the total body mass represented by the head decreases from the fourth month of intrauterine life onward because of the cephalocaudal gradient of growth discussed earlier, at birth the head is still nearly half the total body mass and represents the largest impediment to passage of the infant through the birth canal. Making the head longer and narrower obviously would facilitate birth, and this is accomplished by a literal distortion of its shape (Figure 3-1). The change of shape is possible because at birth, relatively large uncalcified fontanelles persist between the flat bones of the brain case. As the head is compressed within the birth canal, the brain case (calvarium) can increase in length and decrease in width, assuming the desired tubular form and easing passage through the birth canal.
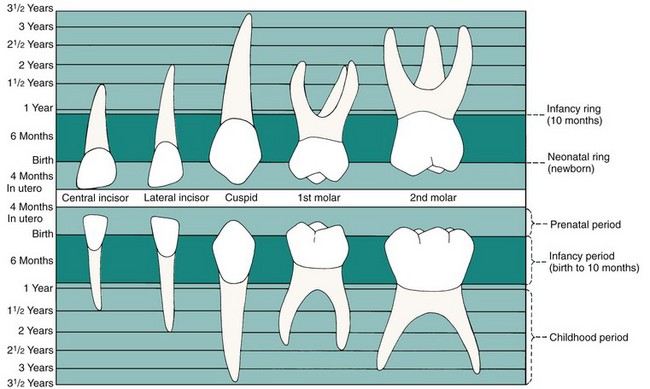
Teeth, on the other hand, are quite visible, and the extent of any growth disturbance related to birth can be seen in the enamel, which is not remodeled. Almost every child has a “neonatal line” across the surface of the primary teeth, its location varying from tooth to tooth depending on the stage of development at birth (Figure 3-2). Under normal circumstances, the line is so slight that it can be seen only if the tooth surface is magnified, but if the neonatal period was stormy, a prominent area of stained, distorted, or poorly calcified enamel can be the result.1
Infancy and Early Childhood: The Primary Dentition Years
Physical Development in the Preschool Years
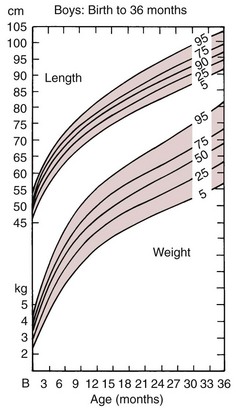
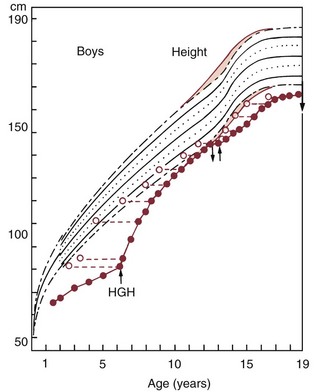
The general pattern of physical development after birth is a continuation of the pattern of the late fetal period: rapid growth continues, with a relatively steady increase in height and weight, although the rate of growth declines as a percentage of the previous body size (Figure 3-3).
The following three circumstances merit special attention:
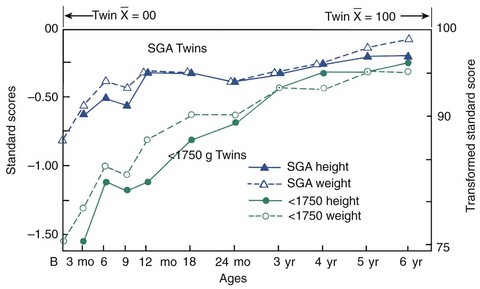
If a premature infant survives the neonatal period, however, there is every reason to expect that growth will follow the normal pattern and that the child will gradually overcome the initial handicap (Figure 3-4). Premature infants can be expected to be small throughout the first and into the second years of life. In many instances, by the third year of life premature and normal-term infants are indistinguishable in attainment of developmental milestones.2
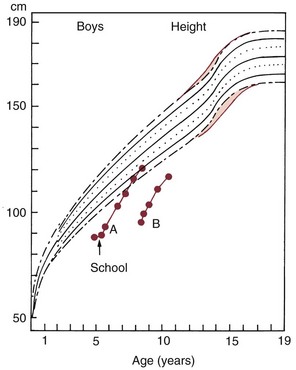
Chronic illness alters this balance, leaving relatively less of the total energy available to support growth. Chronically ill children typically fall behind their healthier peers, and if the illness persists, the growth deficit is cumulative. An episode of acute illness leads to a temporary cessation of growth, but if the growth interruption is relatively brief, there will be no long-term effect. The more chronic the illness, the greater the cumulative impact. Obviously, the more severe the illness, the greater the impact at any given time. Children with congenital hormone deficiencies provide an excellent example. If the hormone is replaced, a dramatic improvement in growth and recovery toward normal height and weight often occurs (Figure 3-5). A congenital heart defect can have a similar effect on growth, and similarly dramatic effects on growth can accompany repair of the defect.3 In extreme cases, psychologic and emotional stress affect physical growth in somewhat the same way as chronic illness (Figure 3-6).
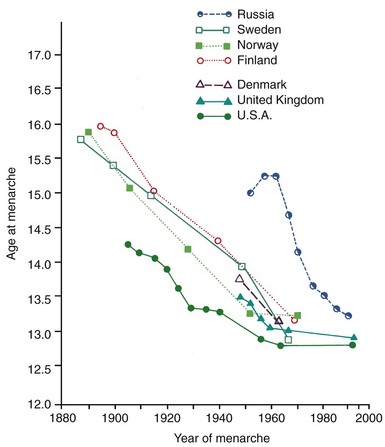
An interesting phenomenon of the last 300 or 400 years, particularly the twentieth century, has been a generalized increase in size of most individuals. There has also been a lowering in the age of sexual maturation, so that children recently have grown faster and matured earlier than they did previously. Since 1900, in the United States the average height has increased 2 to 3 inches, and the average age of girls at first menstruation, the most reliable sign of sexual maturity, has decreased by more than 1 year (Figure 3-7). This “secular trend” toward more rapid growth and earlier maturation has continued until very recently and may still be occurring,4 although there is some evidence that this trend is leveling off.5 Signs of sexual maturation now appear in many otherwise-normal girls much earlier than the previously accepted standard dates, which have not been updated to match the secular change.
Secular changes in body proportions, which presumably reflect environmental influences, also have been observed. It is interesting that skull proportions changed during the last century, with the head and face becoming taller and narrower.6 Some anthropologists feel that such changes are related to the trend toward a softer diet and less functional loading of the facial skeleton (see Chapter 5), but firm evidence does not exist.
Maturation of Oral Function
At birth, if the newborn infant is to survive, an airway must be established within a few minutes and must be maintained thereafter. As Bosma7 demonstrated with a classic radiographic study of newborn infants, to open the airway, the mandible must be positioned downward and the tongue moved downward and forward away from the posterior pharyngeal wall. This allows air to be moved through the nose and across the pharynx into the lungs. Newborn infants are obligatory nasal breathers and do not survive without immediate medical support if the nasal passage is blocked at birth. Later, breathing through the mouth becomes physiologically possible. At all times during life, respiratory needs can alter the postural basis from which oral activities begin.
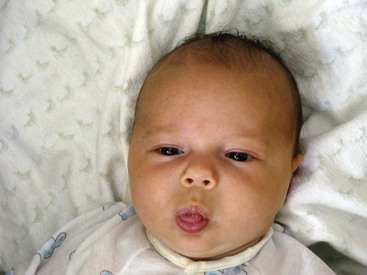
This sequence of events defines an infantile swallow, which is characterized by active contractions of the musculature of the lips, a tongue tip brought forward into contact with the lower lip, and little activity of the posterior tongue or pharyngeal musculature. Tongue-to-lower lip apposition is so common in infants that this posture is usually adopted at rest, and it is frequently possible to gently move the infant’s lip and note that the tongue tip moves with it, almost as if the two were glued together (Figure 3-8). The suckling reflex and the infantile swallow normally disappear during the first year of life.
Nearly all modern infants engage in some sort of habitual non-nutritive sucking—sucking a thumb, finger, or a similarly shaped object. Some fetuses have been reported to suck their thumbs in utero, and the vast majority of infants do so during the period from 6 months to 2 years or later. This is culturally determined to some extent, since children in primitive groups who are allowed ready access to the mother’s breast for a long period rarely suck any other object.8
Surveys of American children indicate that at age 8, about 60% have achieved an adult swallow, while the remaining 40% are still somewhere in the transition.9 After sucking habits are extinguished, a complete transition to the adult swallow may require some months. This is complicated, however, by the fact that an anterior open bite, which may well be present if a sucking habit has persisted for a long time, can delay the transition even further because of the physiologic need to seal the anterior space. The relationship of tongue position and the pattern of swallowing to malocclusion is discussed further in Chapter 5.
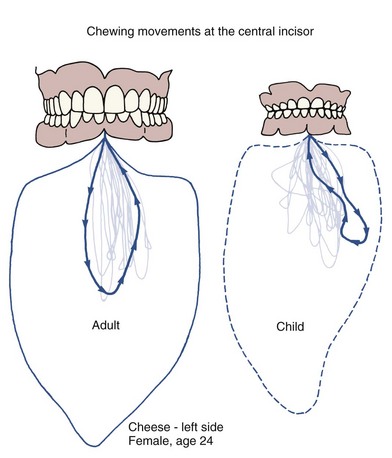
The chewing pattern of the adult is quite different from that of a typical child: an adult typically opens straight down, then moves the jaw laterally and brings the teeth into contact, whereas a child moves the jaw laterally on opening (Figure 3-9). The transition from the juvenile to the adult chewing pattern develops in conjunction with eruption of the permanent canines, at about age 12. Interestingly, adults who do not achieve normal function of the canine teeth because of a severe anterior open bite retain the juvenile chewing pattern.
Eruption of the Primary Teeth
The timing and sequence of eruption of the primary teeth are shown in Table 3-1. The dates of eruption are relatively variable; up to 6 months of acceleration or delay is within the normal range. The eruption sequence, however, is usually preserved. One can expect that the mandibular central incisors will erupt first, closely followed by the other incisors. After a 3- to 4-month interval, the mandibular and maxillary first molars erupt, followed in another 3 or 4 months by the maxillary and mandibular canines, which nearly fill the space between the lateral incisor and first molar. The primary dentition is usually completed at 24 to 30 months as the mandibular, then the maxillary, second molars erupt.
Spacing is normal throughout the anterior part of the primary dentition but is most noticeable in two locations, called the primate spaces. (Most subhuman primates have these spaces throughout life, thus the name.) In the maxillary arch, the primate space is located between the lateral incisors and canines, whereas in the mandibular arch, the space is between the canines and first molars (Figure 3-10). The primate spaces are normally present from the time the teeth erupt. Developmental spaces between the incisors are often present from the beginning but become somewhat larger as the child grows and the alveolar processes expand. Generalized spacing of the primary teeth is a requirement for proper alignment of the permanent incisors.
Late Childhood: The Mixed Dentition Years
Physical Development in Late Childhood
Late childhood, from age 5 or 6 to the onset of puberty, is characterized by important social and behavioral changes (see Chapter 2), but the physical development pattern of the previous period continues. The normally different rates of growth for different tissue systems, however, must be kept in mind. The maximum disparity in the development of different tissue systems occurs in late childhood (see Figure 2-2).
Assessment of Skeletal and Other Developmental Ages
In planning orthodontic treatment, it can be important to know how much skeletal growth remains, so an evaluation of skeletal age is frequently needed. A reliable assessment of skeletal age must be based on the maturational status of markers within the skeletal system. The ossification of the bones of the hand and the wrist was for many years the standard for skeletal development (Figure 3-11). A radiograph of the hand and wrist provides a view of some 30 small bones, all of which have a predictable sequence of ossification. Although a view of no single bone is diagnostic, an assessment of the level of development of the bones in the wrist, hand, and fingers can give an accurate picture of a child’s skeletal development status. To do this, a hand–wrist radiograph of the patient is simply compared with standard radiographic images in an atlas of the de/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses