Chapter 15
Problem Solving in the Management of Painful Tooth Emergencies
Problem-solving challenges and dilemmas in the management of painful tooth emergencies addressed in this chapter are:
“To cure the Tooth-ache, Take a new Nail, and make the Gum bleed with it, then drive it into an Oak. This did Cure William Neal, Sir William Neal’s Son, a very stout Gentleman. When he was almost Mad with the Pain, and had a mind to have Pistoll’d himself.”< ?xml:namespace prefix = "mbp" />
The most important aspects of treating the endodontic emergency patient are accurate and expedient diagnosis of the problem and the ability to relieve the patient’s pain. Diagnoses must be based on the patient’s signs and symptoms, and because pain is always variable and subjective at times, filtering appropriate information during the subjective assessment is essential for all clinicians. Chief complaints are extremely valuable and offer a wide range of potential diagnoses, from mere hypersensitivity to irreversible pulpitis to potential periapical abscess:
Chief complaints also give the clinician clues as to the level of tissue damage if any in the pulp or periapical areas.
Many patients also believe they know which tooth is causing the problem, and here the clinician must be able to selectively filter useful information from information so subjective it should be discarded, such as “The pain hurts me in these three teeth.” It is highly unlikely that there are three problem teeth causing the patient’s symptoms, but in the case of hypersensitivity due to gingival recession, it is possible. The same is true when the patient indicates that a tooth hurts terribly when they drink something cold, and the clinician’s records and radiographs indicate there is a well-done root canal procedure on that particular tooth. The operative words in dealing with a patient’s painful situations are listening, understanding, integrating, analyzing, and synthesizing. Without this problem-solving approach, the clinician may very often jump to invalid conclusions and miss the real diagnosis.
The clinician must decipher from the patient’s own words approximately where the problem is located and how severe the problem has become (see
In reality, however, if the clinician has conducted a thorough examination and has presented the diagnostic dilemma in a compassionate manner, the patient will understand that the symptoms will localize in time to a specific tooth. It will then be possible to diagnose the problem accurately and provide definitive treatment. The solution to difficult diagnostic problems in endodontics is never found by guesswork. It is entirely inappropriate to initiate a root canal procedure with the attitude of “Let’s try this and see if it works.” This is especially true when one considers the many possible sources of nonodontogenic pain (see
Patients Presenting With Complaints of Hypersensitive Teeth
A perceived reason to see the dentist for a painful tooth can be anything from an occasional shooting sensation to a tingling or sensitivity when ingesting certain foods or drink to discomfort during tooth brushing or flossing. If the clinician is seen immediately upon the onset of the symptoms, more often than not there is no pulpal pathosis that requires significant intervention. However, if the patient does not seek help immediately and the problem continues or accentuates, often they are referred to a specialist for an in-depth evaluation or even root canal treatment. It is in these scenarios that a true differential diagnosis must be made—especially to determine whether this is an actual “painful” tooth emergency or merely an accentuated hypersensitivity that was not dealt with previously in a timely manner. The reader is referred to
Patients Presenting With Signs/Symptoms of Reversible Pulpitis
In this pulpal condition, patients will have transient pain of mild to occasionally moderate nature (see
The symptoms of thermal sensitivity do not prevent the patient from eating or drinking normally, although in more severe cases, there may be a history of avoidance of temperature extremes in specific areas of the mouth. In these situations, and in particular when thermal sensitivity is the patient’s chief complaint, the clinician must be able to distinguish between sensitivity and true pain. The interpretation of either by the patient and clinician may vary considerably. Too many cases of root canal treatment are done in the presence of an annoying sensitivity as opposed to a true pain that indicates the need for pulp removal, and too many patients are being overtreated for a minor inflammatory situation that may be handled in a much less aggressive way. The only way to manage these situations properly is to attempt to identify the etiology and remove it. If successful, the transient sensitivity will subside, and the patient will not only be comfortable but grateful to the clinician for the professional expertise in managing the problem.
If an etiology such as caries, exposed cervical margins of dentin, a fractured cusp, or a fractured restoration is discovered, the majority of cases will resolve by appropriate restorative treatment (

FIGURE 15-1 A, This 20-year-old female with slight sensitivity to temperature changes was sent for root canal treatment on the mandibular second molar. All tests were normal, and there were no radiographic changes. B, After caries excavation, a sedative restoration was placed. At the 2-week reassessment, the patient was symptom free.
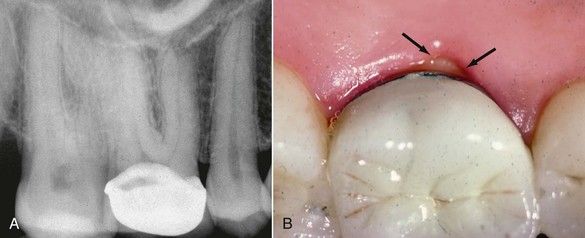
FIGURE 15-2 A, This 45-year-old patient complained of significant pain to cold on a tooth with a newly placed crown and was sent for root canal treatment. She used her finger to point to the palatal aspect of the first molar as her source of discomfort. B, Clinical examination revealed an exposed dentinal margin on the palatal, where the crown was short of the prepared tooth structure (arrows). The patient was advised to have the crown replaced without having root canal treatment.
On occasion, the patient might experience continued mild pulpal pain from a minimal restorative procedure (class I amalgam or class III composite restoration). However, this will not usually degenerate into an irreversible problem unless the pulp was already in a degenerative state prior to the restorative procedure. In these recalcitrant situations, if the pain does not subside after 2 weeks or so, removal of the restoration and placement of a base or sedative dressing may be helpful in alleviating the patient’s symptoms. However, in pursuing this approach, the clinician must remember that at some time the sedative restoration will have to be removed, and in the process all restorative procedures may add additional insult to the dental pulp. If all efforts have been made to maintain the dental pulp in a healthy state and symptoms continue or get progressively worse, a root canal procedure is indicated.
Patients in pain should be made aware that any type of restorative procedure, whether the removal of an existing amalgam, the removal of caries, or preparation of a crown prep or a class II inlay, has the potential to cause pulpal inflammation that may linger for various time periods. In most cases, the inflammation of the pulp is “reversible,” but the pulp is only able to withstand a given amount of insults or irritations before the inflammatory state becomes irreversible. This is a concept not always considered by the restorative dentist prior to extensive restorative procedures. Obvious changes may have occurred in the tooth: a narrowed pulp chamber, the presence of pulp stones or linear calcification in the root canal, hidden caries beneath an old restoration, the presence of various degrees of condensing osteitis, the presence of minor areas of root resorption, obvious crack lines on the margin ridges, and so forth (
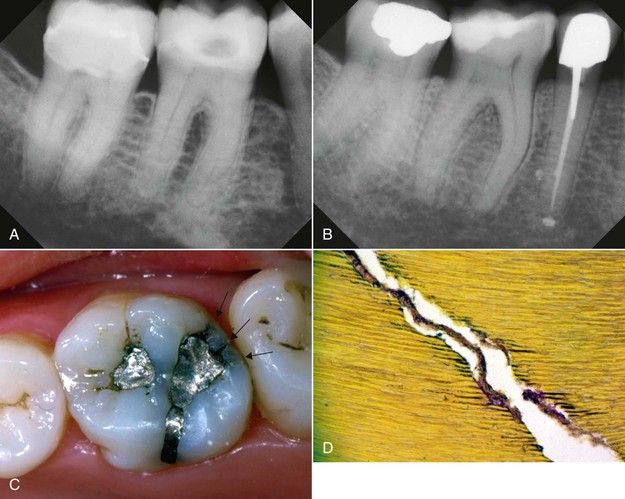
FIGURE 15-3 A, Mandibular first molar with significantly reduced pulp chamber, pulp stones, and condensing osteitis. Changes reflect degenerative pulpitis. No symptoms. B, Mandibular first molar showing a pulp chamber that is almost occluded with calcification and canals that also show the same. While teeth like this may register as “vital,” the pulps are not healthy, and this is where the diagnostic dilemma lies when it is difficult to determine the source of the patient’s distress. C, Occlusal surface that depicts questionable restorative margins and the presence of significant fractures on the distal margin (arrows). Patient was suffering from vague pain in the maxillary left quadrant. D, Crack in tooth dentin showing invasion of bacteria even into the dentinal tubules. In the presence of long-term defects of this nature, dental pulps can easily undergo degeneration and be symptomatic.
Patients Presenting With Signs/Symptoms of Irreversible Pulpitis
The diagnosis of irreversible pulpitis implies that there are sufficient signs and symptoms to indicate that the pulp tissue cannot respond favorably to any type of palliative treatment and must be removed, or the tooth must be removed (see
These findings are all valid indicators of an irreversible pulpitis and in some cases will indicate that the inflammatory response has already progressed through the apical foramen and affected the periapical tissues. This information can be obtained from a thorough history of the patient’s symptoms, and a definitive diagnosis can usually be made regarding the patient’s need for a root canal procedure. However, the true histopathologic status of the tissues cannot be ascertained at this point, so clinical tests must be performed to obtain a pulpal and periradicular diagnosis. The patient’s responses have only informed the clinician of an “irreversible situation” that is occurring but not whether the pulp is inflamed or necrotic. The use of thermal tests may provide a definitive but not entirely accurate diagnosis of the pulpal status.
Procedures to Manage Teeth With Irreversible Pulpitis
Once the diagnosis of irreversible pulpitis has been established, concise treatment will usually provide the patient with immediate relief. However, there are specific treatment modalities with respect to irreversible pulpitis that minimize the patient’s postoperative discomfort and enhance confidence in the treating clinician. The approach to treatment will depend upon two factors. The first is whether the irreversible inflammation is in a single-rooted/single-canal tooth or a multicanal tooth. The second factor is whether the tooth demonstrates sensitivity or pain to percussion. Once these two factors are known, the treatment can be rendered expediently and accurately with a high degree of success and minimal postoperative sequelae. While these two determinants for treatment are not “cast in concrete,” they will guide the clinician in the rapid problem-solving management of these painful situations.
Single-Rooted and Single-Canal Teeth
When a single-rooted or single-canal tooth has been diagnosed with irreversible pulpitis, the ideal treatment is to remove the pulp in its entirety (pulpectomy;
Some clinicians choose to do a pulpotomy because the procedure is virtually the same with respect to the amount of time required. It is more appropriate to perform a pulpectomy than a pulpotomy, however; the latter can leave a significant amount of inflamed pulpal tissue in the root canal system, and symptoms will continue. If the patient exhibits pain to percussion, pulpectomy is the preferred treatment. When the patient demonstrates periradicular inflammation, all of the pulpal tissue should be removed throughout the root canal system.
Multicanal Teeth
Most posterior teeth with irreversible pulpitis will require either a pulpotomy or pulpectomy for immediate pain relief

FIGURE 15-6 A, Mandibular molar with vague symptoms. The radiograph shows chronic focal sclerosing osteitis on the distal root end, indicative of a chronic degenerating pulp. When testing with cold, the tooth exhibited no response at first then gave a throbbing ache that lingered. B,
Mandibular molars with probable carious exposures. Both were painful to percussion and varying degrees of thermal stimulation.
The treatment of posterior teeth is not much different than that of anterior teeth. The canals of posterior teeth are significantly smaller than those of anterior teeth, and emergency procedures may require modification. Only the largest of canals in posterior teeth permit the use of broaches and one seldom sees the pulp as an intact tissue after removal. The removal of the pulp in typical small canals is virtually a by-product of the mechanical enlargement of the canal with rotary or hand files. Patients who are seeking treatment for acute problems on an emergency basis are often seen by dentists who do not have full appointment times immediately available. An emergency visit may be scheduled after normal hours or “squeezed” into an improvised time period during the day. For single canal teeth described above, thorough canal débridement is possible even in an abbreviated time period. For multi-canal teeth, the time commitment for complete preparation to the apices may not be available. Fortunately, in most emergency situations, symptomatic relief can be achieved without removal of all of the pulp to the apices even though this would be preferable. It is important to note the approximate length of the roots and penetrate at least into the apical third in each canal.
On the other hand, it is extremely important to remove pulp tissue from all canals. Patients who seek relief of acute thermal sensitivity can sometimes experience the same symptoms after emergency treatment if vital, acutely inflamed pulp remains intact in one of the canals. Persistent signs and symptoms of an acute apical abscess can also be due to failure to clean a root canal of its inflamed tissue (see
Patients with irreversible pulpitis usually present with a history of severe pain, either spontaneous in nature or stimulated by cold foods or liquids. At times the patient may identify a particular tooth they feel is causing the problem, but the clinician is unable to reproduce the symptoms, even with extensive and rigorous testing. Likewise, the radiographic presentation is often completely normal or at least thought to be normal. There are no signs of abnormal periapical changes, the lamina dura and periodontal ligament space all seem to be within normal limits, several teeth have large restorations or crowns present, but the clinician cannot elicit any pain to percussion or abnormal response to cold from the tooth the patient is convinced is the source of pain. Unfortunately, there is often a disparity between the symptomatic status of a tooth and the histologic picture of its pulp, which may explain the difficulties of diagnosis (
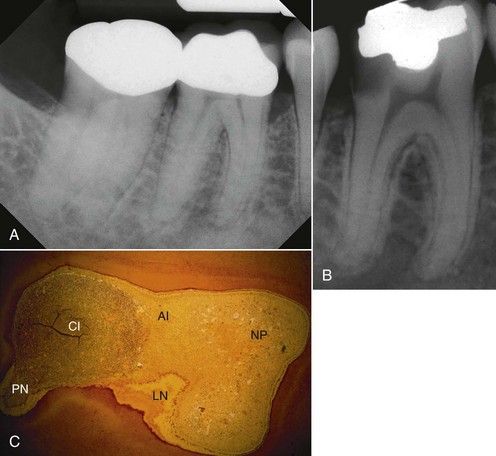
FIGURE 15-7 A, Mandibular molar that exhibits narrowed chamber and canals and the presence of condensing osteitis, indicative of a degenerating pulp. Symptoms are minimal, and tests could not reproduce the patient’s discomfort and chief complaint. B and C may very well provide an explanation of the changes and why it is difficult at times to make a diagnosis. B, Mandibular molar that was symptom free, and the patient had no recollection of any pain or discomfort to function. All tests were normal but because of the depth of the caries, she was advised that root canal treatment was likely to be needed along with a crown to maintain the tooth. Because of cost factors, she opted to have the tooth extracted. C, Histologic section of the coronal pulp. Note the wide variety of histologic findings in a tooth that was symptom free and had normal responses to cold, percussion, palpation, and electric pulp testing. (NP, Normal pulp; AI, acute inflammation; CI, chronic inflammation; PN, partial necrosis; LN, liquefaction necrosis (B&B stain ×4; no bacteria evident).

CLINICAL CHALLENGE
Clinical Challenge #1
In these not-so-rare instances, the clinician must not act based upon the patient’s insistence that a particular tooth is painful and the source of their problems, but rather must rely on the objective findings produced at the time of the emergency visit. If clinical findings are confusing and do not lend themselves to a rapid or logical diagnosis, it may be wise to not act upon meaningless data but wait until valid data can be obtained and an accurate diagnosis established.
In most cases, the symptoms will recur within a short time and the patient can be reexamined. It is always inappropriate for the clinician to begin root canal treatment without having a reasonable diagnosis. Patients have sometimes been subjected to treatment on multiple teeth in the hope of relieving pain only to discover, ultimately, that the pain was of non-dental origin. See
Clinical Challenge #2
It may be necessary to examine clinical findings more comprehensively: How extensive are the restorations that are present? How long have they been there? Are there marginal discrepancies that may be contributing to bacterial leakage? Are there fracture or significant craze lines? Are there changes in the size of the pulp canal spaces and chamber compared to other teeth? Are there pulp stones present? Is condensing osteitis present? Are there subtle changes in the root apex compared to others that may indicate some evidence of a low-grade resorptive process? These questions may or may not be helpful, but they provide a better assessment of the data available and help the clinician make interpretive judgments (see
Clinical Challenge #3
In securing the subjective data, important questions must be asked, and these are detailed in

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses




