15 INTERIM FIXED RESTORATIONS
REQUIREMENTS
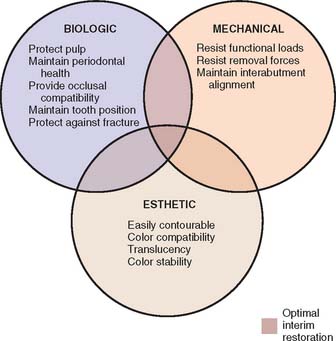
An optimum interim fixed restoration must satisfy many interrelated factors, which can be classified as biologic, mechanical, and esthetic (Fig. 15-1).
Biologic Requirements
Pulpal protection
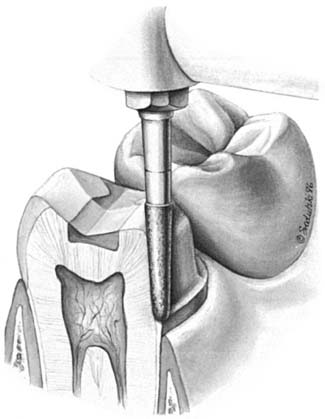
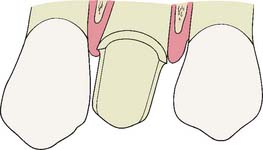
An interim fixed restoration must seal and insulate the prepared tooth surface from the oral environment to prevent sensitivity and further irritation to the pulp. A certain degree of pulp trauma is inevitable during tooth preparation because of the sectioning of dentinal tubules (Fig. 15-2). In health, each tubule contains the cytoplasmic process of a cell body (the odontoblast), whose nucleus is in the pulp cavity. Unless the environment around the exposed dentin is carefully controlled, adverse pulp effects can be expected.1 In addition, the pulp health of a tooth requiring a cast restoration is likely to be compromised before and after preparation (Table 15-1). In severe situations, leakage can cause irreversible pulpitis, with the consequent need for root canal treatment.2
| Past | Present (during fixed prosthodontic therapy) |
|---|---|
| Caries | Preparation trauma |
| Operative dentistry | Microbial exposure |
| Bruxism | Desiccation |
| Periodontal surgery | Chemical exposure |
| Prosthodontic therapy | Thermal exposure |
Periodontal health
To facilitate plaque removal, an interim fixed restoration must have good marginal fit, proper contour, and a smooth surface. This is particularly important when the crown margin is placed apical to the free gingival margin.3 If the interim fixed restoration is inadequate and plaque control is impaired, gingival health deteriorates.4
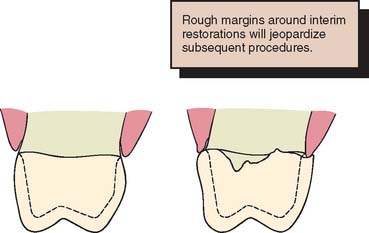
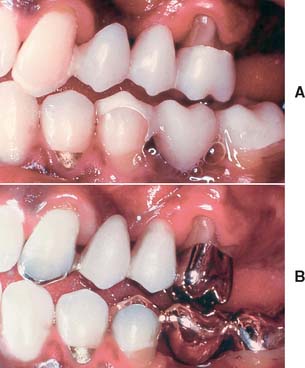
The maintenance of good gingival health is always desirable, but it has special practical significance when fixed prosthodontics is undertaken. Inflamed or hemorrhagic gingival tissues make subsequent procedures (e.g., impression making and cementation) very difficult. The longer the interim fixed restoration must serve, the more significant any deficiencies in its fit and contour become (Fig. 15-3). When gingival tissue is impinged upon, ischemia is likely to develop. This can be detected initially as tissue blanching. If it is not corrected, a localized inflammation or necrosis develops.
Occlusal compatibility and tooth position
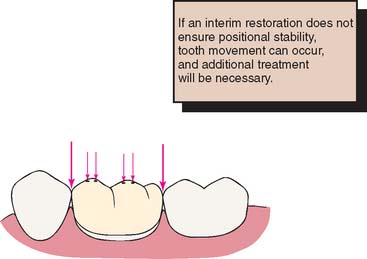
The interim fixed restoration should establish or maintain proper contacts with adjacent and opposing teeth (Fig. 15-4). Inadequate contacts allow supraeruption and horizontal movement. Supraeruption is detected at the evaluation appointment, when the definitive restoration makes premature contact. It is possible to correct this in the operatory, but the effort is time consuming and often leads to a restoration with poor occlusal form and function. Horizontal movement results in excessive or deficient proximal contacts. The former require tedious chairside adjustment; the latter involve a laboratory procedure to add metal or ceramic to the deficient site. In spite of these efforts, proximal crown contours are distorted. This, along with a resulting root proximity (Fig. 15-5), impairs oral hygiene measures.
Prevention of enamel fracture
The interim fixed restoration should protect teeth weakened by crown preparation (Fig. 15-6). This is particularly true with partial coverage designs in which the margin of the preparation is close to the occlusal surface of the tooth and could be damaged during chewing. Even a small chip of enamel makes the definitive restoration unsatisfactory and necessitates a time-consuming remake.
Mechanical Requirements
Function
The greatest stresses in an interim fixed restoration are likely to occur during chewing. Unless the patient avoids contacting the prosthesis when eating, internal stresses are similar to those occurring in the definitive restoration. The strength of polymethyl methacrylate resin is about one-twentieth that of metal-ceramic alloys,5 which makes fracture of the interim fixed restoration much more likely. Fracture is not usually a problem with a complete crown as long as the tooth has been adequately reduced. More frequently, breakage occurs with partial-coverage restorations and partial FDPs. Partial-coverage restorations are inherently weaker because they do not completely encircle the tooth.
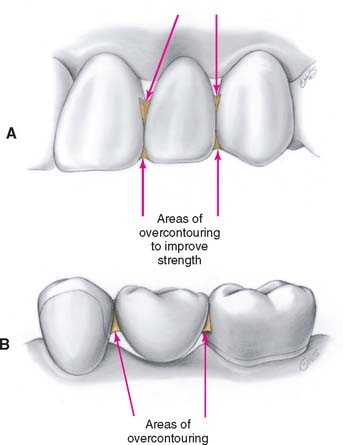
A partial FDP must function as a beam in which substantial occlusal forces are transmitted to the abutments. This creates high stresses in the connectors,6 which are often the site of failure. To reduce the risk of failure, connector size must be increased in the interim restoration in comparison with the definitive restoration (Fig. 15-7). Greater strength is achieved by reducing the depth and sharpness of the embrasures. This increases the cross-sectional area of the connector while reducing the stress concentration associated with sharp internal line angles. The biologic and sometimes the esthetic requirements place limits on just how much larger connectors can be made. To avoid jeopardizing periodontal health, they should not be overcontoured near the gingiva (Fig. 15-8). Good access for plaque control must have high priority.
In some instances, cast metal or heat-processed resin interim restorations can spare the practitioner and the patient inconvenience, lost time, and the expense of remaking a restoration (Box 15-1).
Esthetic Requirements
The appearance of an interim fixed restoration is particularly important for incisors, canines, and sometimes premolars. Although it may not be possible to duplicate exactly the appearance of an unrestored natural tooth, the tooth contour, color, translucency, and texture are essential attributes. When necessary, esthetic enhancement procedures are available to create personalized details; however, because these are not routinely called for, they are addressed on page 500, after the discussion of cementation and repair.
How well a material matches the color of adjacent teeth initially is easily recognized as an essential requirement of prosthodontics. However, some resins discolor with time intraorally,7 and thus color stability (along with the propensity for stain accumulation) governs the selection of materials when a long period of service is anticipated.
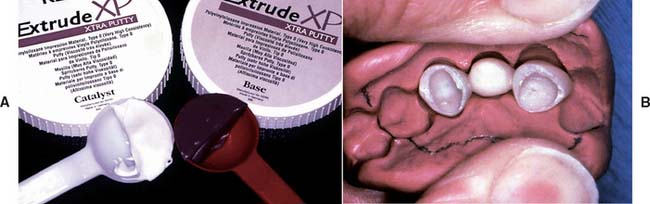
The interim restoration is often used as a guide to achieve optimum esthetics in the definitive restoration. In complete denture prosthodontics, it is customary to have a wax evaluation so that the patient can respond to the dentist’s esthetic interpretation before the denture is processed. Many dentists consider this essential because of the frequency of patients’ requests for changes and the ease with which such changes can be made. When fixed prosthodontics is performed in the anterior oral cavity, it greatly influences appearance, and the patient should be given an opportunity to voice an opinion. Beauty and personal appearance are highly subjective and difficult to communicate verbally, and a facsimile prosthesis can play a vital role in the patient’s consideration of esthetics and the effect that the prosthesis has on his or her self-image. Obtaining the opinions of others whose judgment is valued is also important. An accurate interim restoration is a practical way of obtaining specific feedback for the design of a definitive restoration. Word descriptions alone are often too vague and frequently cause overcorrections, which are difficult to reverse in the definitive restoration. The interim restoration is shaped and modified until its appearance is mutually acceptable to dentist and patient. When this is achieved, an impression is made of the interim restoration (Fig. 15-9) and a cast is poured. This cast accompanies the fixed prosthodontic definitive cast to the laboratory, where the contours are duplicated. This process is more efficient when it begins with diagnostic waxing procedures. Involving the patient in decision making results in greater patient satisfaction.
MATERIALS AND PROCEDURES
Many procedures involving a wide variety of materials are available to make satisfactory interim restorations (Fig. 15-10). As new materials are introduced, associated techniques are reported, and thus there is even more variety. It is a helpful principle that all the procedures have in common the formation of a mold cavity into which a plastic material is poured or packed. Furthermore, the mold cavity is created by two correlated parts: one forming the external contour of the crown or FDP, the other forming the prepared tooth surfaces and (when present) the edentulous ridge contact area. The terms external surface form (ESF) and tissue surface form (TSF) are suggested for these mold parts. This terminology is used in the ensuing discussions.
External Surface Form
There are two general categories of ESFs: custom and preformed.
Custom
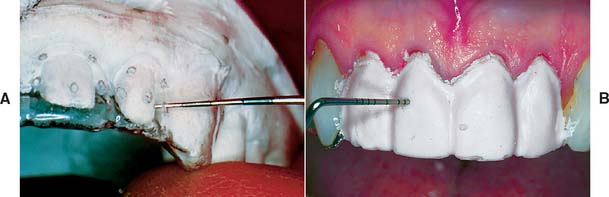
A custom ESF is a negative reproduction of either the patient’s teeth before preparation or a modified diagnostic cast. It may be obtained directly with any impression material. Impressions made in a quadrant tray with irreversible hydrocolloid or silicone are convenient. The higher cost of addition silicone may be offset by its ability to be retained for possible reuse at any future appointment. Accurate reseating of the ESF is easier and the mold cavity produces better results if thin areas of impression material (as may be found interproximally or around the gingival margin) are trimmed away (Fig. 15-11). The moldable putty materials are popular because they can be used without a tray and are easily trimmed to minimum size with a sharp knife. Also, their flexibility facilitates subsequent removal of the polymerized resin (Fig. 15-12).
A custom ESF can be produced from thermoplastic sheets, which are heated and adapted to a stone cast with vacuum or air pressure while the material is still pliable (Fig. 15-13). This produces a transparent form with thin walls, which makes it advantageous in the direct technique because of its minimum interference with the occlusion. It is filled with resin, placed in the mouth, and fully seated as the patient closes into maximum intercuspation. Little additional effort is required to adjust the occlusal contacts. The thinness of the material may also be a disadvantage in the direct technique, however. The material is a poor dissipater of the heat released during resin polymerization, and so care must be taken to remove it from the mouth before injury can occur. A thermoplastic ESF has other uses in fixed prosthodontic treatment, in both the clinical and the laboratory phase; for example, it can be helpful in evaluating the adequacy of tooth reduction8,9 (Fig. 15-14).
Although thermoplastic sheets have a number of advantages, a wide variety of other materials and methods can be used successfully. For example, some practitioners favor baseplate wax because it is convenient and economical (see Fig. 15-10B).
Preformed
Various preformed “crowns” are available commercially. On their own, they rarely satisfy the requirements of a interim restoration, but they can be thought of as ESFs rather than as finished restorations and thus must be lined with autopolymerizing resin. Most crown forms need some modification (internal relief, axial recontouring, occlusal adjustment) in addition to the lining procedure (Fig. 15-15). When extensive modification is required, a custom ESF is superior because it is less time consuming. Preformed crowns are generally limited to use as single restorations, because it is not feasible to use them as pontics for partial FDPs.
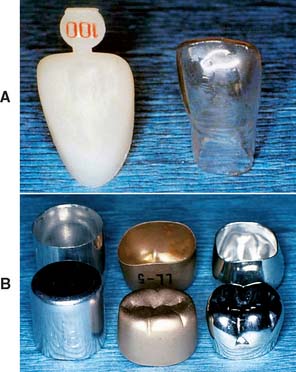
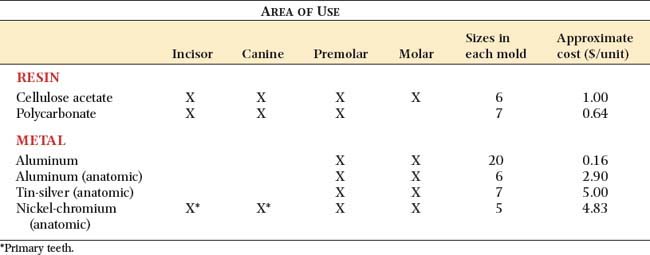
Materials from which preformed ESFs are made (Fig. 15-16) include polycarbonate, cellulose acetate, aluminum, tin-silver, and nickel-chromium. These are available in a variety of tooth types and sizes (Table 15-2).
Polycarbonate
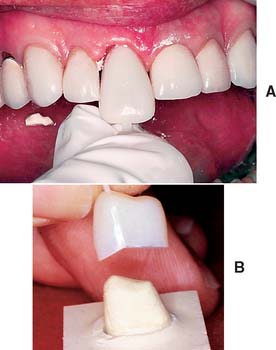
Polycarbonate (Fig. 15-17) has the most natural appearance of all the preformed materials. When properly selected and modified, it rivals in appearance a well-executed porcelain restoration. Although available in only a single shade, this can be modified to a limited extent by the shade of the lining resin. Polycarbonate ESFs are supplied in incisor, canine, and premolar tooth types.
Cellulose acetate
Cellulose acetate is a thin (0.2- to 0.3-mm) transparent material available in all tooth types and a range of sizes (see Fig. 15-16A). Shades are entirely dependent on the autopolymerizing resin. The resin does not chemically or mechanically bond to the inside surface of the shell; therefore, after polymerization, the shell is peeled off and discarded to prevent staining at the interface. Removing the shell has the disadvantage of necessitating the addition of resin to reestablish proximal contacts.
Aluminum and tin-silver
Aluminum (Fig. 15-18) and tin-silver are suitable for posterior teeth. The most elaborate crown forms have anatomically shaped occlusal and axial surfaces. The most basic and least expensive forms are merely cylindrical shells resembling a tin can (see Fig. 15-16B).
The nonanatomic cylindrical shells are inexpensive but require modification to achieve acceptable occlusal and axial surfaces. It is more efficient to use crowns that have been preformed as individual maxillary and mandibular posterior teeth. Care must also be taken to avoid fracturing the delicate cavosurface margin of the tooth preparation when a metal crown form is fitted. This is a greater risk if adaptation is carried out directly by having the patient forcefully occlude on the crown shell. The edge of the shell can engage the margin and fracture it under biting pressure. An even greater risk occurs when the crown has a constricted cervical contour. Tin-silver crowns are deliberately so designed (see Fig. 15-16B). This highly ductile alloy allows the crown cervix to be stretched to fit the tooth closely. Direct stretching on the tooth is practical only where feather edge margins are used. For other margin designs, cervical enlargement should be performed indirectly on a swaging block, which should be supplied with the crown kit.
Nickel-chromium
Nickel-chromium shells (Fig. 15-19) are used primarily for children with extensively damaged primary teeth. In that application, they are not lined with resin but are trimmed, adapted with contouring pliers, and luted with a high-strength cement. They may be applied to secondary teeth but are more suitable for primary teeth, where longevity is less critical. Nickel-chromium alloy is very hard and thus can be used for longer-term interim restorations.
Tissue Surface Form
Indirect procedure
An impression is made of the prepared teeth and ridge tissue and is poured in quick-setting gypsum or polyvinyl siloxane.10 The interim restorations are fabricated outside the mouth. This technique has several advantages over the direct procedures:

Fig. 15-20 Labial (A) and gingival (B) ulcerations after brief polymethyl methacrylate monomer exposure.
Indirect-direct procedure
The indirect-direct approach has these advantages:
Materials for Interim Fixed Restorations
Currently available materials
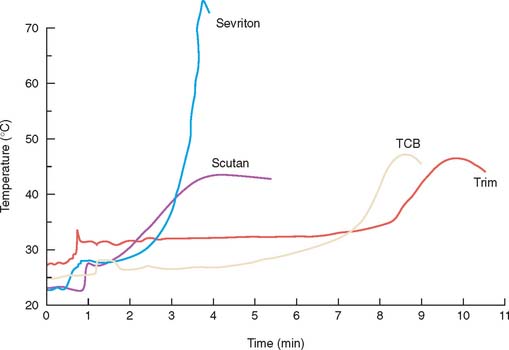
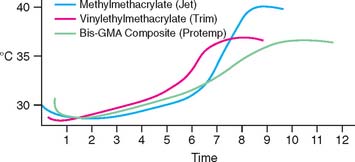
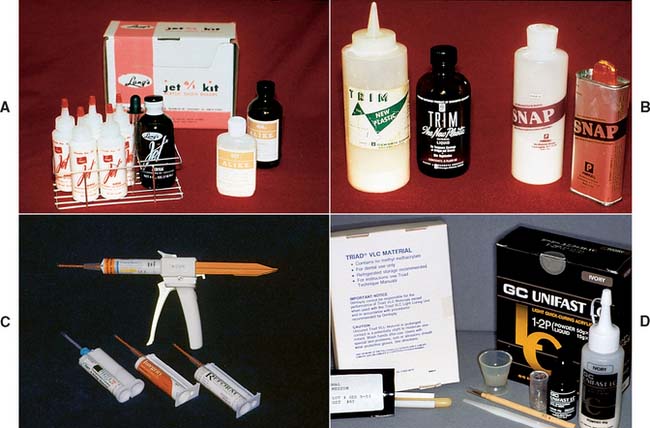
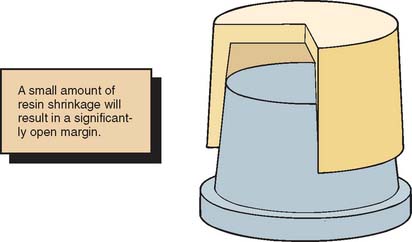
As yet, an ideal interim material has not been developed. A major problem still to be solved is dimensional change during solidification. These materials (Fig. 15-23) shrink and cause marginal discrepancy,20–22 especially when the direct technique is used (Fig. 15-24). Also, the resins currently employed are exothermic and not entirely biocompatible.
The materials can be divided into four resin groups:
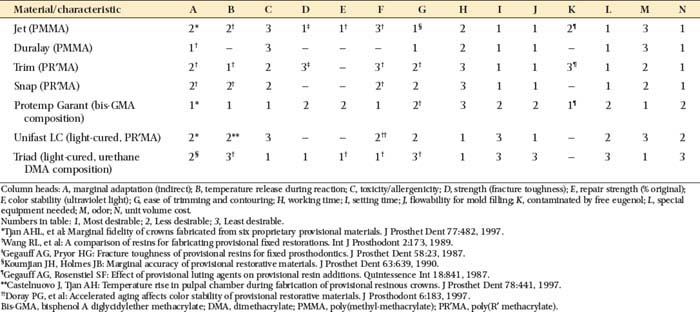
The properties of these resins are compared in Table 15-3. The overall performances of the groups are similar, with no material being superior in all categories. Choosing a material should be based on optimally satisfying the requirements or conditions crucial for the success of the treatment. For example, materials with the least toxicity and least polymerization shrinkage should be chosen for a direct technique. Alternatively, when a long-span prosthesis is being fabricated, high strength is an important selection criterion.
MATERIALS SCIENCE
The material used for fabrication of an interim restoration consists of pigments, monomers, filler, and an initiator, all combining to form an esthetic restorative substance. The pigments are incorporated by the manufacturer so that the set material appears as much like natural tooth structure as possible, with a variety of shades available. Although each of the other ingredients plays a role in the handling, setting, and final properties of the interim restoration, many important characteristics of the material are determined by the primary monomer. The ability of this monomer to convert to a polymer allows the material, after it has been formed as desired, to set into a solid that is durable enough to withstand the oral environment for the necessary interim period.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses