Chapter 15
Cosmetic Rhinoplasty
Most experienced cosmetic facial surgeons regard rhinoplasty as the most challenging and demanding of cosmetic facial procedures. The anatomy is too complex, variable, and diverse for a single surgical approach. There is no one standardized rhinoplasty procedure that can be applied to all noses; each surgery is unique, tailored to the patient’s anatomy and desires. The nose is the most prominent feature on the face and the results are highly visible. Also, the surgeon must be cognizant of how changes in the form of the nose impact the function of the nose, and that one should not sacrifice function while enhancing the appearance. Functions of the nose include olfaction, resonation of speech, humidification, warming or cooling, and filtering of inhaled air. The nasal deformity may be associated with nasal obstruction that needs to be addressed, including a deviated or thickened septum, turbinate hypertrophy, and nasal polyps.
Rhinoplasty is not only the most rewarding but also the most humbling of the cosmetic facial procedures. Since the results are highly subjective, it is most important to perform surgery only on those patients who have realistic expectations. One should be aware of patients who are demanding, secretive about their surgery, or have minimal deformities that have a low benefit-to-risk ratio. One should remember that the preoperative course is finite, but the post-operative visits are infinite, so you must choose your patients wisely.
Rhinoplasty is the ultimate three-dimensional artistic procedure. The surgery should result in balanced, proportional, and natural-appearing facial features. The nose should blend in and enhance the other areas of the face, with the focal point being the eyes. While all aspects of the nose should be symmetrical and aesthetic, the proportional relationship of the nose to the rest of the face is essential for a true cosmetic result.
Applied Surgical Anatomy of the Nose
As the form and function of the nose are intimately related, the surgeon must ensure that the aesthetic change in form does not disrupt the function of the nose. The patient’s nasal airway should not be compromised, if not improved after the surgery. Sheen describes how optimal respiration depends on maintaining functional nasal anatomy with controlled inspiratory and expiratory resistance.1 The nose contributes to the total airway resistance during resting respiration. This resistance has the benefit of improving the distribution of inhaled air over the turbinates, with increased warming and humidification of the inspired air. Increased expiratory resistance increases the pressure within the alveoli and extends the time the alveoli are exposed to oxygen, thereby increasing arterial oxygenation. The resistance of air through the nose results in a smooth transition between the inspiratory and expiratory phases of breathing. One must manage the internal nasal valve, the upper and lower nasal cartilages, the nostrils, and the alar muscles effectively during rhinoplasty as each structure contributes to this controlled airway resistance.
The nose can be divided into three functional parts: upper bony, upper cartilaginous, and lower cartilaginous vaults. The nasal septum supports these parts and creates two separate airways.2,3
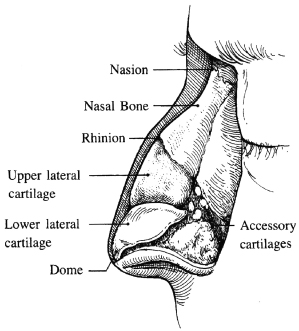
The bony vault is composed of the paired nasal bones that are fused in the midline (Figure 15.1). The nasal bones articulate laterally with the frontal processes of the maxilla and superiorly and posteriorly with the nasal process of the frontal bone. The lateral nasal wall widens inferiorly, becomes thick at its junction with the maxilla and frontal bones, and thins at the caudal margin. The caudal border of the bony vault (the rhinion) forms an arch that articulates with the upper lateral cartilages. This is known as the keystone area as it was once believed to be the center of support for the nasal septum. The anatomical configuration of the bony vault must be considered when planning the lateral osteotomies.4,5
Figure 15.1 Lateral view of the nasal anatomy.
(From Johnson CM Jr., To WC. A Case Approach to Open Structure Rhinoplasty. Philadelphia: Elsevier Saunders, 2005, p. 2.)
The upper cartilaginous vault is composed of the paired triangular upper lateral cartilages that are fused at the dorsal septum to form the cartilaginous bridge of the nose. The cephalic border of these cartilages is secured by fibrous attachments to the underside of the nasal bones. This firm attachment of upper lateral cartilages to the nasal bones, together with the fusion to the nasal septum, gives stability to these cartilages.
The bilateral internal nasal valves are composed of the caudal margin of the upper lateral cartilages, medially by the cartilaginous nasal septum, the inferior turbinates, and the nasal floor. The nasal valve area is the narrowest portion of the nasal airway and is therefore the major contributor to airflow resistance. The edge of the cartilaginous dorsal septum where it meets the upper lateral cartilages is flat and narrows inferiorly. This relationship of the septum to the upper lateral cartilages maintains the proper angle of the lateral cartilages to the nasal septum. The space between the upper lateral cartilages and septum comprising the internal nasal valve can therefore resist the negative inspiratory pressures and remain open during inspiration. In order to maintain a patent nasal airway, there must be a 10–15-degree angle formed by the attachment of the upper lateral cartilages to the septum.6 Spreader grafts (to be described later in this chapter) are frequently utilized to maintain this angle greater than 10 degrees and prevent postoperative nasal valve collapse. Incisions violating the internal nasal mucosa must be avoided to prevent scarring and vestibular stenosis, which also threaten the patency of the internal nasal valve.
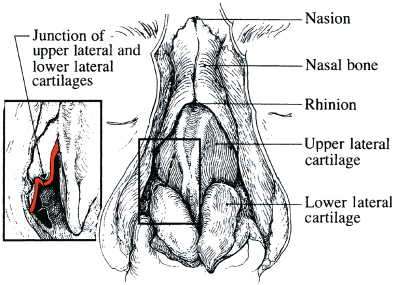
The lower cartilaginous vault forms the nasal base and is composed of all tissues caudal to the upper lateral cartilages. The lower lateral alar cartilages support and give shape to the nasal tip (Figure 15.2). An interdomal ligament connects the lower lateral cartilages at the anterior septal angle, lending support to the nasal tip. Each of the paired lower lateral cartilages consists of a medial, middle, and lateral crus. The medial crura are contained within the columella, with which they form a supportive pillar for the nasal base. At the base of the columella, each medial crus diverges to form footplates that are bound to the caudal septum by fibrous tissue. The depressor septi muscles insert onto the footplates and upon contraction pull down the nasal tip. Each medial crus extends to the apex of the nostril where it joins the middle crus. At this point, the middle crura angle toward the nasal tip, with their direction and length giving shape to the tip lobule. Both lateral crura connect with the middle crus, which is narrowest at the dome and widens laterally to support the ala. The caudal border of the medial half of the lateral crus is parallel to the alar rim and then angles superiorly and laterally. The cephalic margin of the lower lateral cartilages overlaps the caudal edge of the upper lateral cartilages and the cartilages are attached at this junction by an S-shaped recurvature of fibrous tissue (Figure 15.3). The caudal margin of the upper lateral cartilage forms a portion of the internal nasal valve, with the S-shaped recurvature maintaining the lower lateral cartilage lateral to the upper lateral cartilage.4,7 This anatomical relationship contributes to the patency of the internal nasal valve. The lateral crus can be convex, flat, or concave. It attaches to the piriform aperture by a fibrous sesamoid cartilage connection.
Figure 15.2 Basal view of the nasal cartilages.
(From Johnson CM Jr., To WC. A Case Approach to Open Structure Rhinoplasty. Philadelphia: Elsevier Saunders, 2005, p. 6.)
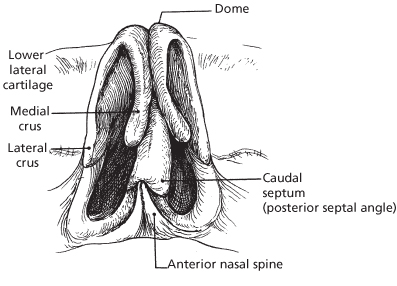
Figure 15.3 Recurvature of the upper lateral cartilages at the fibrous attachment with the lower lateral cartilages.
(From Johnson CM Jr., To WC. A Case Approach to Open Structure Rhinoplasty. Philadelphia: Elsevier Saunders, 2005, p. 5.)
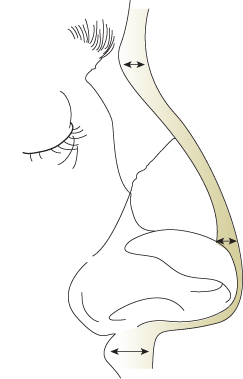
The thickness and quality of the skin–soft tissue envelope (S-STE) directly influence the appearance of the nasal tip. Thick, sebaceous skin will hide the contours of the underlying lower lateral cartilages, whereas a thin S-STE will show the definition of the cartilages. The nasal skin is relatively thick at the radix due to the muscle tissue of the procerus and relatively thin overlying the rhinion due to minimal subcutaneous fat (Figure 15.4). The nasal skin becomes thick again in the supratip area just cephalad to the lower lateral cartilages and tends to thin again over the domes, where it is tightly bound down to the underlying nasal tip cartilages. The supraperichondrial plane is relatively avascular and is the preferred plane of dissection when elevating the S-STE off the nasal cartilages.2,5,6
Figure 15.4 Varied thickness of the overlying skin–soft tissue envelope (S-STE).
(From Johnson CM Jr., To WC. A Case Approach to Open Structure Rhinoplasty. Philadelphia: Elsevier Saunders, 2005, p. 49.)
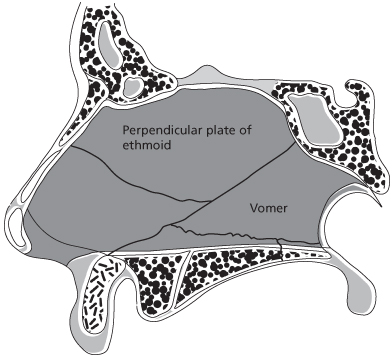
The nasal septum is composed of cartilage anteriorly and thin bone posteriorly (Figure 15.5). The bony parts include the perpendicular plate of the ethmoid, the vomer, the nasal crest of the maxilla, and the nasal crest of the palatine bone. It is bilaterally lined with nasal mucosa and divides the nose into two separate airways. The septum supports the middle vault where it forms the medial portion of the internal nasal valve. The anterior septal angle supports the nasal tip. The quadrangular cartilage that forms the anterior septum can be paper-thin or millimeters thick.2,3 Inferiorly, the nasal septum is set into the vomer, which articulates with the maxillary and palatal crests. The inferior portion of the caudal septum articulates with the anterior nasal spine at the posterior septal angle. The caudal septum is freely movable and forms a gentle curve that gives shape to the columella and supratip. The medial crura and soft tissue columella are attached to the caudal nasal septum by a membranous septum. The nasal septum is frequently used as a donor site for cartilage grafts. Septal deviation can be asymptomatic but if causing an obstruction can lead to crusting, turbinate hypertrophy, and mucosal hyperplasia.5,6
Figure 15.5 Anatomy of the nasal septum.
(From Zide M. Applied surgical anatomy of the nose. Oral Maxillofac Surg Clin North Am 1990; p. 295.)
Of the three nasal turbinates, the inferior turbinate is the principal temperature and humidity regulator of the nose. It has a large surface area, anatomically allows for laminar air flow, is well vascularized, and has an erectile response to a wide array of stimulants, including alcohol, pollen, smoke, and rapid temperature change. Inferior turbinate hypertrophy can lead to chronic hyperplasia and chronic airway obstruction. Resection of the anterior portion of the inferior turbinate usually addresses this obstruction.6
The structures that support the nasal tip include the dense fibrous attachment of the footplates of the medial crura to the caudal septum, the fibrous attachment between the upper and lower lateral cartilages (the scroll area), the interdomal ligament of the lower lateral cartilages that courses over the anterior septal angle, and the attachment of the S-STE to the underlying cartilages.
Nasal Aesthetics
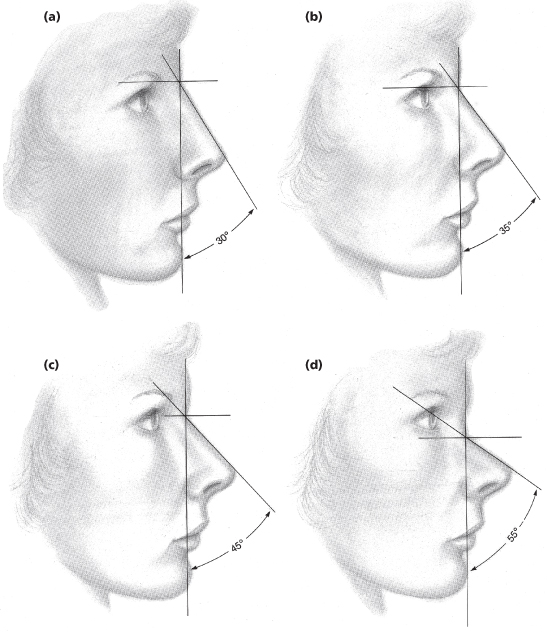
In planning the aesthetic changes of rhinoplasty, one should make the tip fit the dorsum.1,4,7 Planning begins with establishing the ideal position of nasion, the deepest part of the nasofrontal angle, as this is the set point for all aesthetic angles and the starting point of the nose with regard to nasal length. Nasion is ideally set between the lash and crease line of the upper eyelid. The nasion height is ideally 11 mm measured from the corneal plane or 4 mm posterior to the glabella. The radix area, centered at the nasion, extends inferiorly to the level of the lateral canthus and superiorly to a comparable distance. From a lateral view, the radix affects the overall character of the nose (Figure 15.6). With the head positioned at the Frankfort horizontal, the nasofacial angle is formed from a vertical line perpendicular to the Frankfort horizontal through the nasion (vertical facial plane) and the dorsal line drawn from the nasion to the nasal tip-defining points, which represent the junction of the middle and lateral crura of the lower lateral cartilages. The dorsal line is usually slightly concave in females and straight in males. The nasofacial angle signifies the perceived projection of the nose from the face. As the nasofacial angle decreases, the nasal base will appear to become disproportionately larger and more projecting. The higher the nasal dorsum, the smaller the nasal base appears. The ideal nasofacial angle, as defined by Western culture, is 34 degrees for females and 36 degrees for males.7
Figure 15.6 Perception of nasal tip projection with the changing position of the radix. The nasal base is unchanged in each diagram.
(From Sheen JH, Sheen AP. Aesthetic Rhinoplasty, 2nd ed. St. Louis, MO: Mosby, 1987, p.73.)
From the anterior view, two symmetrical divergent concave lines should extend from the supraorbital ridges through the radix to the lateral margins of the dorsum and end at the tip-defining points (Figure 15.7). The width of the tip-defining points should measure 6–8 mm for females and 8–10 mm for males. This closely corresponds to the width of the philtral columns.1,5
Figure 15.7 Aesthetic dorsal line on frontal view.
(From Sheen JH, Sheen AP. Aesthetic Rhinoplasty, 2nd ed. St. Louis, MO: Mosby, 1987, p. 75.)
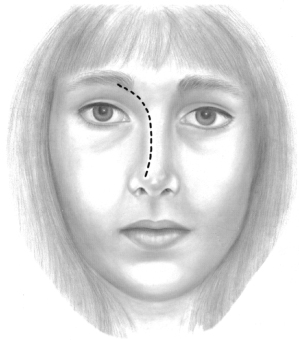
Nasal tip definition will depend on the thickness of the overlying S-STE and the size and position of the lower lateral cartilages. In the anterior view, the dorsum should have sufficient height to give the eyes the appearance of proportional intercanthal width. If the dorsum is too low, the eyes will appear too far apart.
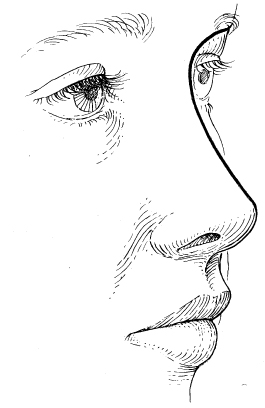
From an oblique view, there should be an unbroken line extending from the supraorbital ridge to the radix and along the dorsal line to the nasal tip (Figure 15.8). The columella should be parallel to and 2–3 mm lower than the alar rims.
Figure 15.8 Aesthetic dorsal line on oblique view.
(From Sheen JH, Sheen AP. Aesthetic Rhinoplasty, 2nd ed. St. Louis, MO: Mosby, 1987, p. 81.)
A pseudo dorsal hump is usually due to an inferiorly positioned nasion. Radix augmentation can place the nasion superiorly, thereby increasing nasal length. By augmenting the radix, the dorsal reduction will be less or may not be indicated. Deep temporal fascia is the preferred augmentation material, although morselized nasal septal or conchal cartilage can be used. Due to settling and resorption of the temporal fascia graft, you should plan on a 25% overcorrection.7
Tip projection is measured in the lateral view from a line drawn from the vertical facial plane at the alar crease to the nasal tip. The tip projection is ideally two-thirds the distance of the dorsum length, which is two-thirds of the ideal midfacial height. The tip angle measures the amount of tip rotation. This is the angle formed from the vertical facial plane at the alar crease through the tip. The ideal tip angle is 105 degrees in females and 100 degrees in males.1,7
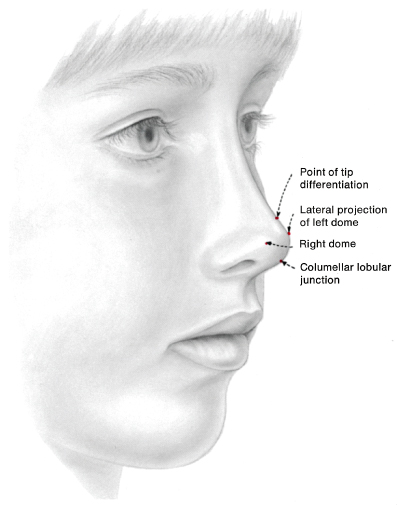
The alar base width should approximate the intercanthal distance. The ideal alar base width is 70% of the nasal length. The columella-alar complex in frontal view has the appearance of gull wings in flight. In profile view, the columella should be displayed no more than 3–4 mm inferior to the alar rims and should be parallel to the rims. Two lines, one tangent to the columella and the other tangent to the tip lobule, form the angle of rotation of the nasal tip. This angle should be approximately 50 degrees. The tip-defining point is the most dorsal portion of the lower lateral cartilage at the columella, corresponding to the junction of the middle and lateral crus (Figure 15.9). The infratip lobule corresponds to the junction of the middle and medial crus. The nasolabial angle should be approximately 90 degrees in men and 110 degrees in women.1,7
Figure 15.9 Landmarks of the aesthetic nasal tip.
(From Sheen JH, Sheen AP. Aesthetic Rhinoplasty, 2nd ed. St. Louis, MO: Mosby, 1987, p. 84.)
From a basal view, the nares are pear-shaped, with the nostril width being no greater than 50% of the nostril length. The columella should be two-thirds of the nasal height and the nasal lobule should be one-third of the nasal height. The soft tissue triangle denotes the soft tissue of the nasal tip that occupies the space between the medial and lateral crura of the lower lateral cartilage.
Preoperative Evaluation
It is important to spend time consulting with patients to determine if they are acceptable candidates for cosmetic rhinoplasty. Patients should discuss with their doctors what they dislike about their noses, what has motivated them to undergo surgery, and their expectations for acceptable results. Much of this information can be obtained through consultation utilizing video imaging. Video imaging allows the patient to visualize the proposed changes and to accept or reject treatment options. There is increased dialogue between the patient and the surgeon, with an opportunity to determine if the patient may be a poor candidate due to unrealistic expectations. Imaging leads to accurate treatment planning and is most useful in assessing nasal and facial proportional relationships. For example, the intimate relationship between the projection of the nose and the chin can be evaluated, as can the nasion and dorsal line, nasolabial angle, and tip projection and rotation. Most importantly, video imaging allows doctors to critically examine their postsurgical results when compared with the planned treatment. Of course, the surgeon must use the imaging conservatively and not to propose overly optimistic modifications that would be difficult to achieve. Patients should sign a disclaimer form prior to video imaging to state their understanding that the proposed imaging does not guarantee the surgical result.
At the initial consultation, a detailed examination is performed of the external and internal nose. The nose is evaluated for the presence of a septal deviation and asymmetries involving the nasal bone and upper and lower lateral cartilages. The thickness and character of the nasal tip skin is determined, as is the strength or weakness of the domal cartilages. The dorsal hump is examined for the percentage of cartilage versus bony tissue. The position of the nasion is noted and the length of the nose is compared with the base of the nose. Internally, the nasal valve competency should be noted and any septal deviations, bony spurs, or polyps identified. Any history of allergies, epistaxis, nasal obstructive breathing, and chronic sinusitis should be noted. The clinical exam should be performed prior to and after administration of a nasal vasoconstrictor spray to shrink the nasal mucosa.
The anatomy of the nose is complex and the healing phase is variable and can be unpredictable. The anatomical limitations of the patient’s nose should be identified and a treatment plan developed that permits the most predictable aesthetic and functional results. This is most important in patients who present with thick skin in the nasal tip with underlying thin and pliable lower lateral cartilages.8,9 The overlying thick, sebaceous skin will not conform to changes made in the cartilages. And if the tip skin is too thin, then definitions of the underlying structures, including irregularities, will tend to show. Ideally, the overlying skin should be />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


