Clinical Features of Gingivitis
Experimental gingivitis studies provided the first empiric evidence that the accumulation of microbial biofilm on clean tooth surfaces results in the development of an inflammatory process around gingival tissue.41,69 Research has also shown that the local inflammation will persist as long as the microbial biofilm is present adjacent to the gingival tissues and that the inflammation may resolve subsequent to a meticulous removal of the biofilm.69
The prevalence of gingivitis is evident worldwide. For example, epidemiologic studies indicate that more than 82% of adolescents in the United States have overt gingivitis and signs of gingival bleeding. A similar or higher prevalence of gingivitis is reported for children and adolescents in other parts of the world.7 A significant percentage of adults also show signs of gingivitis; more than half of the US adult population is estimated to exhibit gingival bleeding, and other populations show even higher levels of gingival inflammation.3,5,6,8,66 Whereas plaque remains the primary etiological factor that causes gingivitis, other factors may affect the development of periodontal diseases. Recent experimental gingivitis studies suggest an important role of the host response in the development and degree of gingival inflammation.81
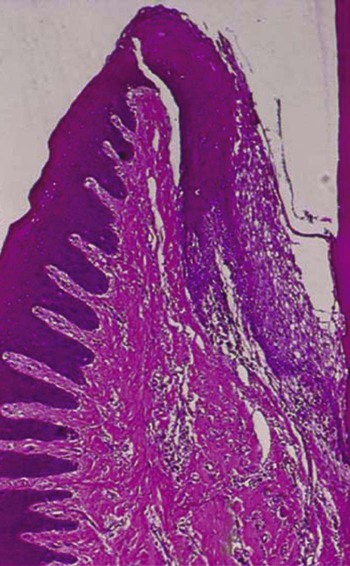
In general, clinical features of gingivitis may be characterized by the presence of any of the following clinical signs: redness and sponginess of the gingival tissue, bleeding on provocation, changes in contour, and the presence of calculus or plaque with no radiographic evidence of crestal bone loss.10 The histologic examination of inflamed gingival tissue reveals ulcerated epithelium. The presence of inflammatory mediators negatively affects epithelial function as a protective barrier. Repair of this ulcerated epithelium depends on the proliferative or regenerative activity of the epithelial cells. Removal of the etiologic agents that triggered the gingival breakdown is essential.
Course and Duration
Chronic gingivitis is slow in onset and of long duration. It is painless, unless it is complicated by acute or subacute exacerbations, and it is the type that is most often encountered (Figure 15-1). Chronic gingivitis is a fluctuating disease in which inflammation persists or resolves and in which normal areas become inflamed.30,36
Description
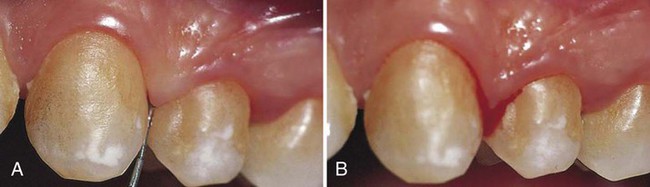
• Localized marginal gingivitis is confined to one or more areas of the marginal gingiva (Figure 15-2).

• Localized diffuse gingivitis extends from the margin to the mucobuccal fold in a limited area (Figure 15-3).
• Localized papillary gingivitis is confined to one or more interdental spaces in a limited area (Figure 15-4).
• Generalized marginal gingivitis involves the gingival margins in relation to all the teeth. The interdental papillae are usually affected (Figure 15-5).
• Generalized diffuse gingivitis involves the entire gingiva. The alveolar mucosa and the attached gingiva are affected, so the mucogingival junction is sometimes obliterated (Figure 15-6). Systemic conditions can be involved in the cause of generalized diffuse gingivitis and should be evaluated if they are suspected as an etiologic cofactor.
Clinical Findings
Gingival Bleeding on Probing
The two earliest signs of gingival inflammation that precede established gingivitis are as follows: (1) increased gingival crevicular fluid production rate; and (2) bleeding from the gingival sulcus on gentle probing (Figure 15-7). Chapter 13 discusses gingival crevicular fluid in detail.
Gingival bleeding varies with regard to severity, duration, and ease of provocation. Bleeding on probing is easily detected clinically and therefore is of value for the early diagnosis and prevention of more advanced gingivitis. It has been shown that bleeding on probing appears earlier than a change in color or other visual signs of inflammation36,37,46; in addition, the use of bleeding rather than color changes to diagnose early gingival inflammation is advantageous in that bleeding is a more objective sign that requires less subjective estimation by the examiner. For example, it is estimated that 53.2 million (50.3%) US adults who are 30 years old and older exhibit gingival bleeding.6 Probing pocket depth measurements by themselves are of limited value for the assessment of the extent and severity of gingivitis. For example, gingival recession may result in a reduction of the probing depth and thus cause an inaccurate assessment of the periodontal status.4 Therefore, bleeding on probing is widely used by clinicians and epidemiologists to measure disease prevalence and progression, to measure outcomes of treatment, and to motivate patients to perform necessary home care.24 Several gingival indices that are based on bleeding have been developed,2,16,53 as described in Chapter 4. (For further considerations of probing, see Chapter 29.)
In general, gingival bleeding on probing indicates an inflammatory lesion both in the epithelium and in the connective tissue that exhibits specific histologic differences as compared with healthy gingiva.25 Even though gingival bleeding on probing may not be a good diagnostic indicator for clinical attachment loss, its absence is an excellent negative predictor of future attachment loss.34 Therefore, the absence of gingival bleeding on probing is desirable and implies a low risk of future clinical attachment loss. Longitudinal findings revealed that sites with consistent bleeding (gingival index = 2) had 70% more attachment loss than sites that were noninflamed over a 26-year period in 565 males. Thus, persistent gingivitis can be considered as a risk factor for periodontal attachment loss that may lead to tooth loss.35
Interestingly, numerous studies have shown that current cigarette smoking suppresses the gingival inflammatory response, and smoking was found to exert a strong, chronic, dose-dependent suppressive effect on gingival bleeding with probing in the Third National Health and Nutrition Examination Survey.19 In addition, recent research reveals an increase in gingival bleeding with probing in patients who quit smoking.54 Thus, people who are committed to a smoking cessation program should be informed about the possibility of an increase in gingival bleeding associated with smoking cessation.
Gingival Bleeding Caused by Local Factors
Factors that contribute to plaque retention and that may lead to gingivitis include anatomic and developmental tooth variations, caries, frenum pull, iatrogenic factors, malpositioned teeth, mouth breathing, overhangs, partial dentures, lack of attached gingiva, and recession. In addition, orthodontic treatment and fixed retainers were associated with increased plaque retention and increased bleeding on probing.38,78
Chronic and Recurrent Bleeding.
The most common cause of abnormal gingival bleeding on probing is chronic inflammation.50 The bleeding is chronic or recurrent, and it is provoked by mechanical trauma (e.g., from toothbrushing, toothpicks, or food impaction) or by biting into solid foods (e.g., apples).
Histologic evaluations of animal specimens revealed that, during the early stages of gingivitis, the expression of the cytokines responsible for connective tissue breakdown—matrix metalloproteinases (MMPs)—is ubiquitous. Different MMPs play a role in this breakdown at different stages (e.g., a decrease of MMP-14 activity at 7 days of inflammation; an immediate increase in MMP-2, especially with fibroblastic stimulation). In addition, MMP-9 expression peaked 5 days after gingivitis occurrence, which was also regulated by macrophages and neutrophils. Thus, extracellular matrix remodeling was regulated with MMP-2 and MMP-9 production and activation by the host inflammatory response.42
The severity of bleeding and the ease of its provocation depend on the intensity of the inflammation. After the vessels are damaged and ruptured, interrelated mechanisms induce hemostasis.73 The vessel walls contract, blood flow diminishes, blood platelets adhere to the edges of the tissue, and a fibrous clot is formed that contracts and results in approximation of the edges of the injured area. Bleeding recurs when the area is irritated.
Gingival Bleeding Associated with Systemic Changes
With some systemic disorders, gingival hemorrhage occurs spontaneously or after irritation, and it is excessive and difficult to control. These hemorrhagic diseases represent a wide variety of conditions that vary with regard to etiologic factors and clinical manifestations. Such conditions have the common feature of a hemostatic mechanism failure and result in abnormal bleeding in the skin, the internal organs, and other tissues, including the oral mucosa.71
Hemorrhagic disorders in which abnormal gingival bleeding is encountered include vascular abnormalities (vitamin C deficiency, allergy [e.g., Henoch–Schönlein purpura]), platelet disorders27 (thrombocytopenic purpura), hypoprothrombinemia (vitamin K deficiency), other coagulation defects (hemophilia, leukemia, Christmas disease), deficient platelet thromboplastic factor as a result of uremia,47 multiple myeloma,12 and postrubella purpura.30 The effects of hormonal replacement therapy, oral contraceptives, pregnancy, and the menstrual cycle are also reported to affect gingival bleeding.43,65,79,80 In addition, in women, long-term depression-related stress exposure may increase concentrations of interleukin-6 in gingival crevicular fluid and worsen periodontal conditions with elevated gingival inflammation and increased pocket depths.32
In addition, changes in androgenic hormones have long been established as significant modifying factors in gingivitis, especially among adolescents. Several reports have shown notable effects of fluctuating estrogen and progesterone levels on the periodontium, starting as early as puberty.1,55 Among pathologic endocrine changes, diabetes is an endocrine condition with a well-characterized effect on gingivitis.78 In diabetes, marked inflammation affects both the epithelial and connective tissues, which leads to the degeneration of the dermal papilla, an increase in the number of inflammatory cells, the destruction of reticulin fibers, and an accumulation of dense collagen fibers that causes fibrosis.70
Several medications have also been found to have adverse effects on the gingiva. For example, anticonvulsants, antihypertensive calcium channel blockers, and immunosuppressant drugs are known to cause gingival enlargement (see Chapter 16), which secondarily can cause gingival bleeding. The American Heart Association has recommended over-the-counter aspirin as a therapeutic agent for cardiovascular disease, and aspirin is often prescribed for rheumatoid arthritis, osteoarthritis, rheumatic fever, and other inflammatory joint diseases.28 Thus, it is important to consider aspirin’s effect on bleeding during a routine dental examination to avoid false-positive readings, which could result in an inaccurate patient diagnosis.67 (Chapter 11 discusses periodontal involvement in hematologic disorders.)
Color Changes in the Gingiva
Color Changes with Gingivitis.
Change in color is an important clinical sign of gingival disease. The normal gingival color is “coral pink,” and it is produced by the tissue’s vascularity and modified by the overlying epithelial layers. For this reason, the gingiva becomes red when vascularization increases or when the degree of epithelial keratinization is reduced or disappears. The color becomes pale when vascularization is reduced (in association with fibrosis of the corium) or when epithelial keratinization increases. Thus, chronic inflammation intensifies the red or bluish-red color as a result of vascular proliferation and a reduction of keratinization. In addition, venous stasis will contribute a bluish hue. The gingival color changes with increasing chronicity of the inflammatory process. The changes start in the interdental papillae and the gingival margin and then spread to the attached gingiva (see
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses