Retention and stability: A perspective
Longitudinal changes in the untreated person, as well as in the treated orthodontic patient, remain a fascinating area of study. Moreover, the stability following orthodontic treatment has been a topic of interest and great discussion since the inception of the orthodontic specialty. Hence, retention regimens have become an essential part of the contemporary orthodontic treatment plan. Ultimate success depends on a compilation of steps, including appropriate planning, well-controlled treatment mechanics, retention compliance and, in general, an appreciation of the biological limits of tooth movement. This chapter provides an overview of the retention versus stability concept, defines relapse and stability, provides a perspective on the management of stability, shows the difficulty in achieving stability or the lack thereof and ultimately endeavours to elicit discussion and encourage further investigation into this important area of the orthodontic discipline.
The need to obtain developmental and morphologic homeostasis following orthodontic treatment, or in orthodontic terms, the pursuit to understand the fine balance that exists between stability and relapse has resulted in many attempts to identify some significant factor(s) responsible for posttreatment relapse.1–30 Every time an orthodontist treats a patient with a malocclusion, it is assumed that the outcome will favour success. The possibility of failure is, however, very real and thus the quest for some form of long-term stability has become one of the most significant challenges in orthodontics. Notwithstanding many research efforts, a workable concept that takes into account the complex circumstances dealing with equilibrium and stability versus imbalance and relapse is lacking. At the present time, no mechanical instrument is available to determine or to predict the stability of a dentition. Although attempts in this regard have been reported in the literature, no method presently exists to predict accurately the future status of the posttreatment orthodontic occlusion.1–5 Taken into account the multifactorial nature of long-term stability, the multivariate regression model (standardized coefficients) is probably at this time the closest to provide an indication of the factors involved in stability.6
Fortunately, efforts to improve knowledge and treatment methods in orthodontics have resulted in many excellent investigations into aspects of relapse.6,14,15,27–29 Despite these important studies, many causes of orthodontic relapse are not fully understood.20 Many pitfalls that lead to treatment problems exist, and no orthodontist is immune to them.25,26
Given the recognized problems associated with orthodontic treatment, certain relapse changes may be anticipated. The patient’s original problem, unfavourable cooperation and poor growth are the factors that may forewarn that relapse is a possibility. At other times, relapse will occur unexpectedly and for no obvious reason. Moreover, the fact that a malocclusion is corrected, or for that matter left untreated, is also no guarantee that no further changes will occur as normal untreated occlusions show longitudinal changes. Occlusal stability after orthodontic treatment should be considered a primary goal for every orthodontist.15 In the search for postorthodontic treatment stability, it may be necessary for an orthodontist to review the diagnosis, consider the potential growth and developmental changes expected, change the treatment regimen or even vary the overall treatment philosophy en route to attain acceptable clinical outcome (Fig 14.1).

Figure 14.1 Clinical goals for good treatment, according to Tweed,32 should display an aesthetic, healthy, functional and stable occlusion following treatment. The keys of occlusion described by Andrews11,12 emphasize these parameters.
This chapter provides a summary overview of long-term changes and management of these changes to show where the discipline of orthodontics finds itself in respect to contemporary retention and stability; in addition, it shows the difficulty in achieving stability or the lack thereof, elicits discussion and encourages further investigation into this important area of the orthodontic discipline.
Requirements for retention and stability
Retention, according to Joondeph and Riedel,33 is the holding of teeth in ideal aesthetic and functional positions. Retention is thus the action or fact of holding, retaining or keeping the teeth in a fixed place or position; that is, the condition of being retained.34 Retention is accomplished by a variety of mechanical appliances (Fig 14.2).
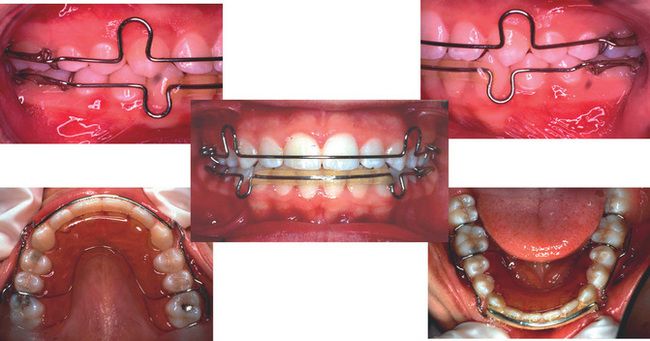
Figure 14.2 The removable retainer is still a popular choice and the favourite retaining appliance used by the author of this chapter.
It is important to ensure that the retention protocol is in physiological harmony with the function of the masticatory system. The goal of physiological stability seems to be the practical outcome of successful treatment versus a rigid set of treatment parameters that do not ensure long-term stability. Retention requirements thus should be decided at the diagnosis and planning stage of treatment; the following are important to consider at this stage:
Terms that are commonly used and others less universally known to define or describe relapse or posttreatment changes include relapse, physiologic recovery, developmental changes, growth recovery, rebound, postretention settling, recidief, crowding or recrowding, imbrication, stability, retention, metaposition, compensation, adaptation, iatrogenic changes and physiologic stability.36
Definition of stability
Stability is the condition of maintaining equilibrium.34 This refers to the quality or condition of being stable. Some orthodontists may be reluctant to evaluate their patients in the postretention phase of treatment. However, it is only through a retrospective view of treatment that factors, which cause undesirable postretention changes can be identified. Such discoveries could lead to greater occlusal stability after orthodontic treatment. It is important to recognize that stability is not retention. Therefore, it is necessary to distinguish between relapse, physiologic recovery and developmental changes. The term relapse has been used, perhaps erroneously, when referring to all posttreatment changes.37 This word is usually sensed a failure. However, physiologic stability is a term defined by Rossouw36 and appears to encompass the acceptable changes a clinician can expect; it also includes the normal ageing changes of the dentition, which take place irrespective of treatment outcome. That is; physiologic stability refers to events such as growth and development, occlusal settling, physiologic influences, rebound effects as a result of the elasticity of the tissues and the more difficult to control neuromuscular influences.
Relapse occurs when the corrected malocclusion slips back or falls back to a former condition, especially after improvement or seeming improvement. Riedel38 believed that the word was too harsh a description of the changes that follow orthodontic treatment, and he preferred the term posttreatment adjustment for these changes. However, poor clinical treatment should not be conducted or condoned under the designation of relapse or under the auspices of one of the other terms noted as part of the long-term stability problem. It is imperative to be cognizant of the different descriptions of long-term change to enable the clinician to interpret stability of the finished result and also provide adequate communication of possible posttreatment changes to prospective patients. Thus, all orthodontic patients should be well-informed of the expected long-term changes and the need to conform to retention protocol.
The retention process can thus be seen as an another phase of orthodontic care – a phase where the occlusion is observed as it accommodates to a new environment – in addition, minor adjustments can be made in order to facilitate this settling and wean the patient away from the retaining devices as maturity of the adolescent is attained or when the desired outcome goals have been established. However, some occlusions may necessitate permanent retention either to maintain a patient’s objective or to negate the influences of aberrant neuromuscular influences. The finalization process should include both active stabilization and passive guidance procedures, rather than rigid fixation of teeth, which after treatment could be in unphysiologic positions. The purist orthodontist or the true occlusionist endeavours to produce a healthy, functional, aesthetic and physiologic stable occlusion that will last for the patient’s lifetime (Fig 14.3).
Normal changes in the untreated dentition
One of the most often cited treatment requests is that of the correction of lower incisor crowding, needless to say that it is probably also the most often complaint in respect to changes following orthodontic treatment; that of late lower incisor irregularity. The focus of many studies has been on the mandibular arch, the assumption being that alignment of the lower arch serves as a template around which the upper arch develops and functions. The following questions: ‘Why is retention necessary?’ ‘When can retainer use be discontinued, and will significant change follow?’ are answered in the most objective manner by observing the long-term changes occurring as a result of normal ageing.
Measurement of lower incisor irregularity
Data from the National Health and Nutrition Survey (NHANES) conducted between 1988 and 1991 in respect to the oral health in the United States shows that 54.5% of children between age 8 and 11 years possess well-aligned lower incisors.39 A common measurement tool to show the degree of irregularity of the lower incisors is the Little Irregularity Index.31 This index provides a millimetre number to indicate the discrepancy in contact points between the lower anterior teeth and canine-to-canine (Fig 14.4).
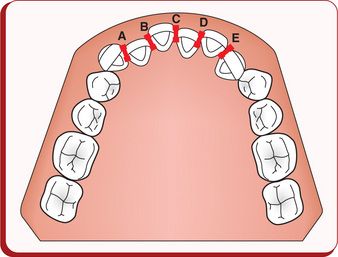
Figure 14.4 Irregularity Index.31 The aggregate of the millimetre measurements of the discrepancy of the contact points (A + B + C + D + E) provides the score of the Index. Less than 3.5 mm is clinically acceptable, 3.5–5.5 mm indicates moderate irregularity and greater than 5.5 mm indicates severe irregularity.
An adult sample from the NHANES III study (19881994) was investigated by Buschang and Shulman40 in respect to their mandibular incisor irregularity. Buschang and Shulman40 compiled the clinically relevant information from the evaluation of untreated subjects, 15–50 years of age, from the NHANES III study that is portrayed in Figure 14.5. Note that approximately 39.5% of this sample showed moderate to severe irregularity, thus the group that definitely requires some form of orthodontic treatment. Approximately 50% fall in the clinically acceptable range and may or may not require treatment depending on the compilation of factors.
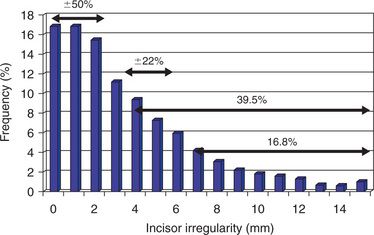
Figure 14.5 Mandibular incisor irregularity in untreated US subjects, 15–50 years of age. The subjects who showed moderate to severe irregularity were 39.5%. Using the irregularity index from Figure 14.4,31 the various categories of irregularities for the sample is shown. Modified from Buschang PH, Shulman JD. Angle Orthod 2003; 73:502–508.
A study from the Burlington Growth Center at the University of Toronto by Eslambolchi et al41 provided information as to longitudinal changes that can be expected from an untreated sample. Longitudinal or long-term change is mostly recorded as the difference(s) between two intervals, preferably over a long period of time. Time point 1 (T1) represents the beginning of the assessment (in treated evaluations this will be the beginning of treatment), and time point 2 (T2) normally represents the end of an age interval in untreated measurements or in treatment change evaluation that indicates the end of treatment (posttreatment interval). The third time point (T3) merely indicates another time interval or age interval, and in a treatment change assessment this mostly indicates the postretention interval. In the above-noted study, longitudinal changes in untreated children (at T1C = 13y, T2c = 19,6y and T3c = 42,4y) and their untreated parents (at T1p = 36,1 and T2p = 69,4y) were compared to determine when the tempo of irregularity changes. Parameters that have become measurement standards in long-term studies included intercanine width, interfirst premolar width, arch length, anterior space and total space. All these measurements showed a decrease from T1 to T2, from T2 to T3 and overall from T1 to T3. Interestingly, the lower incisor irregularity index continued to increase. However, an important observation was made regarding the rate of change. In children, this index was slower between T2 and T3 compared to T1and T2. The parent sample showed an even slower change compared to the children; in particular after age 40 (Fig 14.6). This rate impacts retention decisions; it is apparent that retention time may be significantly reduced as an individual ages due to this slow down in longitudinal changes.
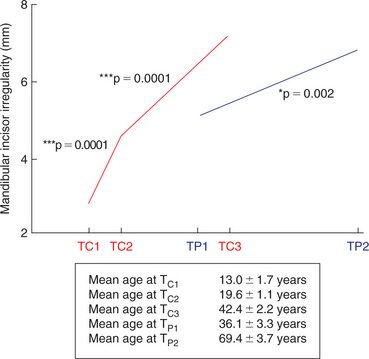
Figure 14.6 Combined changes in the Little Irregularity Index in a sample of untreated children and their parents (Eslambolchi41).
A comparison of the rate of change in crowding in various longitudinal samples presented by Buschang and Shulman40 also showed a continual change in irregularity of lower incisors in the long-term. Moreover, the data also confirmed that this continual tempo of increase in the irregularity in the long-term appears to decrease with ageing from approximately the middle of the second decade onwards with some hope of long-term stability.
The latter information thus shows that the untreated dentition appears to show continual changes into adulthood, even into the seventh decade; a fact also confirmed by Behrents42 in his assessment of longitudinal changes in individuals of the Bolton-Brush growth study. Not only does the dentition change over time but also the entire craniofacial environment including the soft tissues undergo continual changes (Figs 14.7 and 14.8).
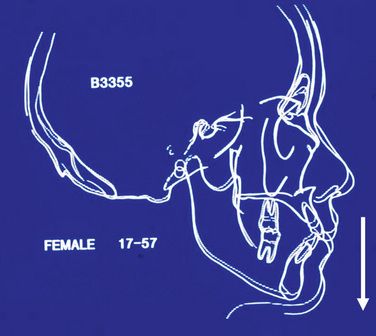
Figure 14.7 Female long-term changes. Note the vertical changes occurring from 17 to 57 years of age. From Kaplan RG. Am J Orthod 1974; 66:411–130.
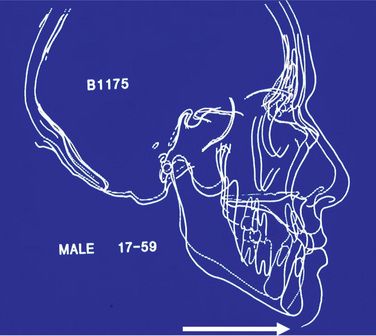
Figure 14.8 Male long-term changes. Note the horizontal changes occurring from 17 to 59 years of age. From Behrents RG. Ann Arbor: University of Michigan; 1985.
Bolton-Brush Growth Sample (Figs 14.7 and 14.8) shows the following general longitudinal changes (Behrents42):
The treated dentition is no more or less susceptible to the above-noted changes. Thus, there is no surprise when authors recommend permanent life-time retention.19,44,45 It is important to have an understanding of how the untreated dentition behaves as it can be extrapolated to that of the posttreatment orthodontic occlusion.
Changes in alignment in the untreated lower arch occur at various developmental stages. On average, crowding decreases between 7 and 12 years (mixed dentition development) and increases thereafter (loss of Leeway and eventually E-space). According to Richardson,45 the maximum increase occurs in the teenage years between 13 and 18, little or no change occurs in the third decade and small increases occur later in life. As mentioned previously,40,41 it appears that the increase in lower incisor irregularity increases rapidly into the third and fourth decades followed by a decrease in the velocity of change after 40 years of age.
Overbite and overjet changes
Other changes may also influence the stability of the occlusion and thus the retention phase of the posttreatment occlusion. Overbite and overjet increase significantly from the mixed to the permanent dentition. During the maturation of the permanent dentition (13–20 years), these changes were reversed, and decreases in overbite and overjet were observed by Barrow and White,46 Bjork,47 Moorrees,48 and Sinclair and Little.49
Other dental arch changes
Intermolar width remains relatively stable in untreated individuals.41,48–52 Arch length decreases over time.41,46,48,49–52 Moreover, longitudinal data show that changes in arch dimensions, as well as lower incisor crowding occur as part of the normal ageing process.41,42,46,48–52
One could refer to these changes as the wrinkling of the teeth. Late mandibular incisor crowding, thus, may be unrelated to any previous orthodontic treatment. There is no doubt that normal untreated occlusions provide valuable insight into longitudinal changes and thus management of tooth alignment.
Natural space for lower incisor alignment
After eruption of the lower permanent incisors, it appears that there is little or no skeletal growth in the anterior part of the lower jaw at this time.3,7,32–34 An important means of creating space for incisor alignment is the fact that the lower incisors procline relative to the mandibular plane by an average of 13° between 5 and 11 years.13 This gain in space is enhanced by an increase in arch width across the canines caused by alveolar growth, just before and during the eruption of the permanent incisors.2,4,35
In addition, Leeway space or ultimately E-space provides space for the larger permanent incisors; that is the excess space by which the primary molars and canine is larger compared to their permanent successors.51–60 Any disturbance in establishing the normal occlusion as described could have a detrimental impact on the alignment of the lower incisors.
Anterior component of force resulting in mesial migration of teeth
The cause of increased crowding in the intact lower arch is not fully understood. It is obviously multifactorial, and for this reason, it is difficult to show a cause and effect relationship. Mesial migration of human teeth has been recognized since the late eighteenth century, when it was described by John Hunter,61 and is shown as the forward movement of the posterior teeth during adolescence. There is evidence to support the view that it is largely responsible for the increase in crowding during the teenage years. Mesial migration may be caused by physiological mesial drift, by the anterior component of the force of occlusion on mesially inclined teeth, by the mesial vectors of muscular contraction or by the contraction of the transseptal fibres of the periodontal ligament.50,51,53,55,58,62,63
Role of third molars in the development of mandibular incisor crowding
Third molar agenesis and extraction studies63–66 suggest that mesial migration is greater in the presence of a developing third molar. This suggestion is strongly reinforced by second molar extraction studies.67,68 Removal of the second molar effectively isolates the third molar from the rest of the arch. The reduction in crowding and the distal movement of first molars in patients whose second molars have been extracted compared with the increase in crowding and mesial movement of first molars in nonextraction subjects67,68 provide convincing evidence of the effects of developing third molars on the anterior part of the arch. Other studies on patients treated by extraction of second molars69–72 reported similar results. It is a mistaken impression that it is only impacted third molars that cause the problem. A third molar that erupts is likely to exert more pressure on the dental arch than the one that remains impacted, and some impacted third molars may exert more pressure than others.73,74
Decisions relative to the timing of third molar extraction should be made on the basis of potential development of pathosis, technical considerations of the surgical procedure and long-term periodontal implications rather than potential impact on mandibular incisor crowding.75 Although erupting mandibular third molars probably exert some force on the dentition,76–80 most of the scientific studies81–83 have found no significant correlation between the presence or absence of mandibular third molars and developmental incisor crowding. The effect of mandibular third molars on the dentition, particularly the lower incisors, remains unclear according to Bishara and Andreasen.84
Mandibular growth and its effect on late mandibular incisor crowding
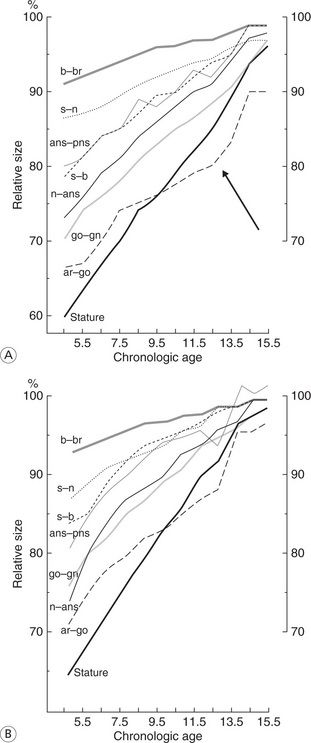
Changes in mandibular growth direction and rotation during the posttreatment and postretention periods have also been implicated in the aetiology of late incisor crowding.85–87 In addition, the vertical development of the mandibular ramus continues until late adolescence (Fig 14.9A and B : Buschang et al88). Crowding of the mandibular incisors was observed in vertical growers as a result of chronic airway obstruction.89,90
Changes in the treated dentition
Role of extraction or nonextraction treatment on the stability of the treated occlusion
Orthodontists routinely are faced with the dilemma of attaining aesthetic soft tissue profiles versus long-term stability. Moreover, a controversy exists as to which treatment decision, extraction or nonextraction, will eventually lead to orthodontic stability. Extraction of teeth as an aid in the treatment of malocclusion is one of the oldest and most controversial subjects in the history of orthodontics. Dr Edward H Angle’s9 nonextraction influence dominated the discipline of orthodontics for many years; however, a change was eminent when Dr Charles H Tweed,10,91,103 one of Angle’s most ardent supporters, became so discouraged by postretention relapse that he deemed it necessary to include extractions into his treatment regimen to meet his original orthodontic objectives; that being stable, healthy, functional and aesthetic. Tweed91 subsequently investigated 100 extraction and 100 nonextraction subjects, 25 years postretention and concluded that the extraction cases were more stable than were the nonextraction cases. However, as extraction spaces are closed and the teeth are moved together orthodontically, the adjacent teeth do not move through the gingival tissue but appear to push the gingivae in front of them into a fold of epithelial and connective tissue. This excess tissue can result in the opening of the extraction space that constitutes a common form of relapse of orthodontically treated occlusions. Edwards92 recommended to remove this tissue surgically so that relapse could be alleviated.
The presence of mandibular incisor crowding indicates that there is a space shortage somewhere in the dental arches. The incisor position93–96 and facial profile, in combination with a tootharch size analysis, provide clues that can help to make a decision whether an extraction or non-extraction treatment protocol must be followed.
Glenn et al95 studied 28 nonextraction treatment cases, an average of 8 years out of retention. In these patients, who were treated by the same orthodontist, they found that slight incisor irregularity occurred postretention. Sinclair and Little49 noted that relapse patterns were similar to, but more severe than, those seen in a study conducted in an untreated normal population. The changes in the normal population were only one half as severe as those observed in studies carried out by Little et al.19,44
An evaluation of long-term posttreatment orthodontic changes after at least 1019 or more years,44 which included premolar extractions, 97,98 lower incisor extractions,99 non-extraction cases with generalized spacing and patients treated with arch expansion provided further insight into treated occlusions. Observations from the results of the noted studies were made in comparison to changes occurring in untreated normal control subjects.5,14 Similar physiologic changes were reported in all the groups, which also conform to other long-term studies published. The changes observed included the following:
The question thus arises as to what effect the orthodontic technique or appliance management may have on the long-term dental changes. According to Little et al,19 when lower incisors, measured to the point A-pogonion (APo) line, were proclined an average of 1.4 mm during treatment, they tended to remain stable postretention. Sandusky15 reported on the postretention stability of 83 extraction cases treated by Tweed and Tweed foundation members. Using Little’s Irregularity Index to grade the results, Sandusky15 found less than 10% relapse of the lower incisors. The general orthodontic treatment philosophy appears to play a role in the long-term occlusal outcome. This was illustrated by Woodside et al102 in a comparison of serial extraction not followed by active treatment (driftodontics) with that of extraction treatment followed by active treatment and concluded that the actual orthodontic treatment appears to influence the long-term changes. The untreated occlusions showed less change.
Tweed103 suggested that mandibular incisors should, as is found in normal individuals, always be positioned upright over the medullary bone of the jaw. Relapse of orthodontically treated dentitions may be influenced by apical base differences, the subject’s age, the time of retention, incisor positions relative to basal bone, posttreatment growth, third molar development, periodontal fibres, habits, occlusal functioning, Bolton discrepancies, continued decrease in arch length and other unknown factors.19
A tendency exists in contemporary orthodontics to pursue a completely nonextraction philosophy; that is a dependency on growth and ‘arch development’. Friel104 showed that natural expansion does, however, occur as a result of normal growth and development. It could be incorrect to assume that the appliances used during this growth period were the cause of the expansion. The results of a number of cephalometric studies dealing with the treatment effects of functional appliances on Class 11 division 1 malocclusions concluded that overjet reduction occurred predominantly as a result of dentoalveolar changes.105 Dentoalveolar changes also appeared to be largely responsible for overjet relapse, especially when incisors were proclined during treatment.106–108 Anteroposterior or lateral increase in the mandibular archform usually fails with the dental arch typically returning to the pretreatment size and shape.109 Haas110 showed that malocclusions treated by means of rapid maxillary expansion (RPE), however, remained stable, 8 years posttreatment. Haas110 maintained that his success can be ascribed to a combination of the RPE and to the duration of the retention which he uses.
Moreover, the extraction versus nonextraction debate is still with us as the incidence of nonextraction treatment has shown an increase similar to the 1920s. Based on the available literature, arch expansion as a space-gaining procedure must be approached with caution.111 Mandibular intercanine width is regarded as a fixed entity, and the early literature recommends that it should not be expanded if stability is an objective of treatment.112–115 Expansion of the maxillary arch can be achieved with RPEs93,110,116–121 and to a lesser extent with archwires.28,121–124 Postretention, relapse percentages vary after archwire expansion28,123,124; average relapse after RPE treatment is approximately 20%.94,120 Similar to the maxillary arch, expansion of the mandibular arch has been achieved with expansion appliances, such as the lip bumper,93,124–127 and again, to a lesser extent with archwires.94,122,123 Postretention arch dimensional changes appear to occur regardless of the treatment modality, although more arch width is lost after expansion with archwires alone.93,95,118,123,124 Blumber et al128 reported on the short-term postretention stability of the transverse dimension in patients with Class I malocclusion, treated with the Damon System (Ormco, CA). All of the treatment increases in transverse arch dimensions were significant (maxillary arch 2.0–5.6 mm and mandibular arch 2.4–4.6 mm) and greater than expected when compared to untreated controls. Postretention decreases for many of the measurements were significant; however, often less than expected when compared with untreated controls. Moreover, significant net gains remained, especially in the mandibular arch. Occlusal settling occurred following active treatment causing significant improvement in posttreatment outcomes. Retention was for an average of 2.1 ± 0.9 years, followed by no retention for an average of 2.3 ± 0.9 years.
Simons and Joondeph129 have reported that irrespective of whether individuals were treated with or without extractions, relapse of overbite, as well as relapse of lower incisor alignment, still occurs after the removal of the appliances. Only about 30% of occlusions treated with first premolar extraction therapy retained good anterior mandibular alignment while two-thirds of the sample relapsed.19 In comparing the results of a sample showing minimal incisor relapse130 with a sample showing about two-thirds relapse,19 Gorman131 concluded that the orthodontic technique used plays an important role in achieving stability of the post-treatment orthodontic result.
Conlin132 recalled 1000 subjects and valuated their long-term dental stability and facial aesthetics. He found that there was no real need for extraction cases to appear flat or for nonextraction cases to appear full. Thus, one of the greatest challenges in orthodontics is the need to make a sound diagnosis. No cookbook recipe is available with respect to extraction or nonextraction treatment. Various strategies are used to aid orthodontists in their extraction decisions, including the use of visual treatment objectives.133,134
With above 28 years of orthodontic experience, Gorman131 explained that his perspective on retention has changed from an expectation of universal stability following bicuspid extraction and 2 years of retention to the realization that individual retention plans must be developed for each patient irrespective of the treatment regime (extraction or nonextraction) used. The extraction of teeth, or for that matter nonextraction of teeth, do not necessarily assure long-term stability of the corrected malocclusion, especially lower incisors; however, clinically stable results can be achieved.102,111,135,136
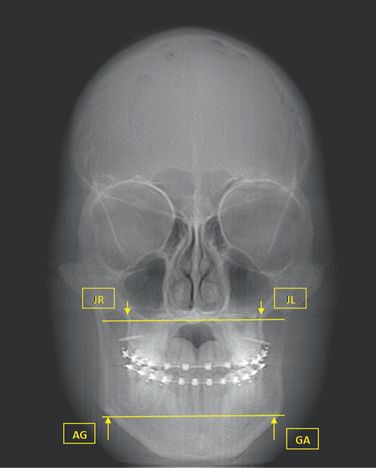
Stability of archform has been considered to be one of the most elusive goals of treatment. Diagnosis and treatment of the transverse dimension are important steps on the way to attain a stable treatment outcome. Vanarsdall137 emphasizes the critical importance of utilizing the Ricketts138 analysis on the frontal cephalogram (Fig 14.10) to determine the skeletal differential between the width of the maxilla and the width of the mandible (Table 14.1) irrespective of following an extraction or nonextraction treatment. He refers to this differential as measured on a posteroanterior cephalogram (PA) and emphasizes that undiagnosed transverse discrepancy leads to adverse periodontal response, unstable dental camouflage and less than optimal dentofacial aesthetics. The normal (maxillary and mandibular) values for the Caucasian race (values for all racial and ethnic groups and even genders will vary), but the differential between the width of the maxilla and width of the mandible, is the critical evaluation for the individual patient.
Table 14.1
The mean normal maxillomandibular differentials from Vanarsdall (1999).137
Larger values indicate that the mandibular width is much larger compared with the maxillary width, and thus the maxilla requires expansion. Clinical opinion will justify whether surgical, RPE, arch wire only or a combination of these will provide adequate expansion for long-term stability.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses