Temporomandibular joint
Learning objectives
Key terms
Anterior tympanic artery
Ascending pharyngeal artery
Auriculotemporal
Deep auricular artery
Deep temporal
Ginglymoarthrodial
Gliding action
Hinge action
Lateral ligament
Lateral pterygoid
Lingula
Masseter
Masseteric
Medial pterygoid
Sphenomandibular ligament
Stylomandibular ligament
Superficial temporal artery
Synovial membrane
Temporalis
Temporomandibular ligament
Overview
This chapter discusses articulation between the condyles of the mandible and temporomandibular fossa of the temporal bone. The temporomandibular joint (TMJ) allows the mandibular condyles to move in both gliding and hinge actions. Therefore, instead of being a stationary hinge, the joint slides along the inclined plane while functioning also as a hinge joint. The complex motion of the joint can be observed during mastication. TMJ problems can be associated with pain in the related muscles of the jaws and neck.
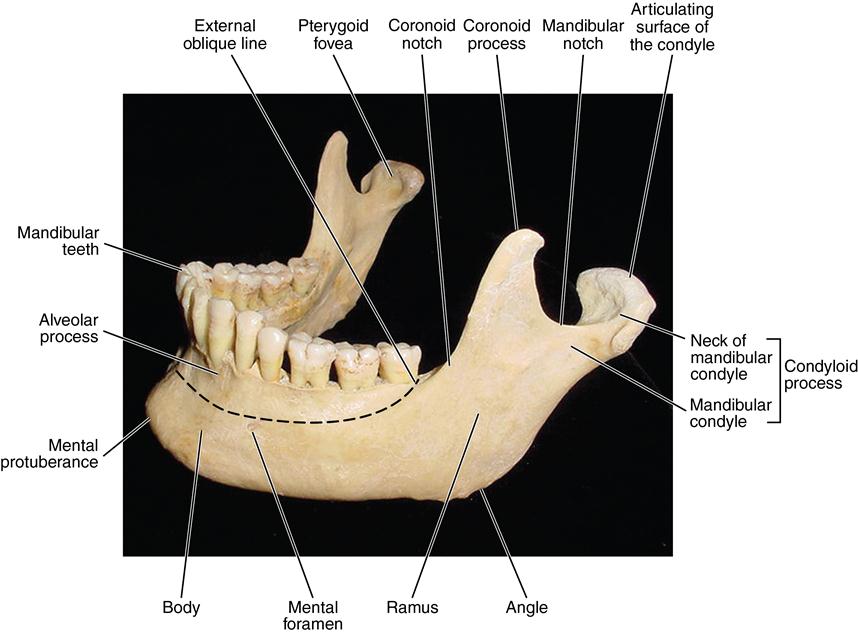
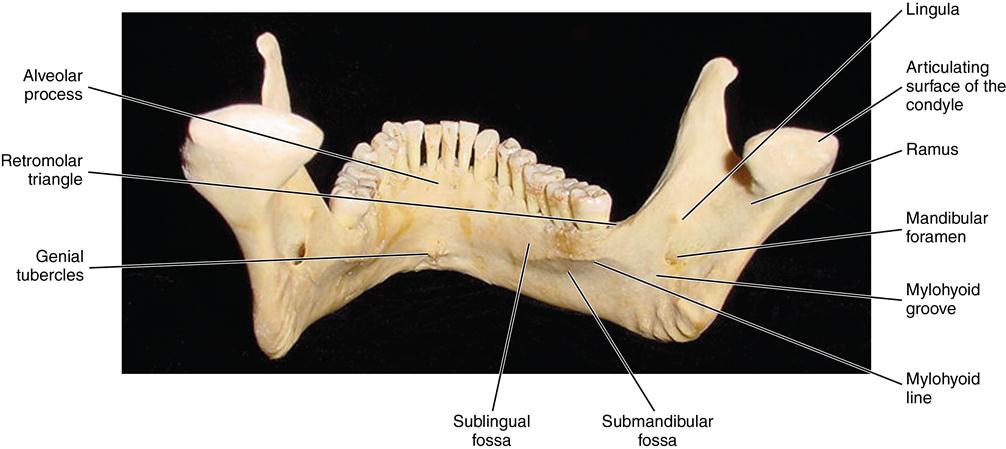
The anatomy, histology, and function of the various structures related to jaw function are described in this chapter. The TMJ includes (1) the right and left condylar heads of the mandible, (2) the articulating surfaces of the mandibular condyles and the temporal fossae, (3) a disk that intervenes between the fossa and condyle, and (4) a capsule and supportive ligaments. The capsule enclosing this joint serves as a stabilizer, making complex function possible (Fig. 13-1).
The fibrous articular disk divides the joint in two. The upper half is involved in sliding action, and the lower functions as a hinge action. The joint is supported anteriorly by a tendinous attachment of the capsule and the lateral pterygoid muscle, laterally by the lateral or temporomandibular ligament, medially by the sphenomandibular ligament, and posteriorly by the stylomandibular ligament. The TMJ functions as a ginglymoarthrodial joint, indicating that it moves as a sliding and hinge joint.
Myofascial pain dysfunction (MPD) is a syndrome that has received attention. It has been defined as a complex problem relating to neuromuscular concepts, occlusal concepts, muscle balance, tooth morphology, and guidance and psychophysiologic factors. Much remains to be learned about the normal and abnormal stomatognathic system.
Structure
Mandibular condyle
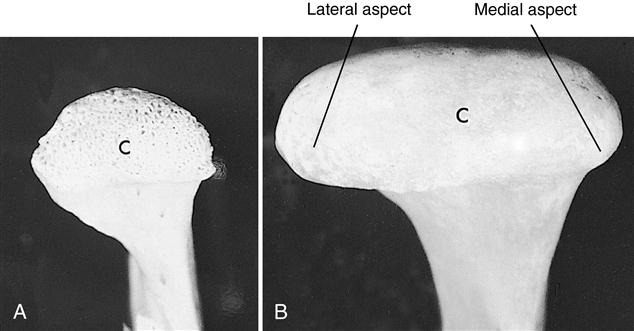
The right and left heads of the mandibular condyles articulate in the temporomandibular or glenoid fossae. At birth, the heads of the condyles are round and covered with a thick layer of cartilage. The cartilage front is uneven with spikes of cartilage projecting into the underlying marrow space. Bone forms around these spikes so the head of the condyle is porous (Fig. 13-2, A). During development, the condyle grows in a lateral direction, changing into an ovoid shape by maturity, which is attained at age 25 years (Fig. 13-2, B). The oval condyle consists of a smooth, bony surface, which is covered with a layer of fibrous connective tissue in the adult. The cartilage serves as a growth site in the condyle.
New cartilage cells arise from near the surface of the perichondrium, which covers the condyle. The cartilage cells grow and divide, and the cells deeper in the cartilage die as the cartilage that surrounds these cells calcifies (Fig. 13-3, A). The calcified cartilage is then replaced by bone from the underlying ramus (Fig. 13-3, B). This process continues during development with a gradual thinning of the cartilage layer, and at maturity the cartilage has been replaced by bone (Fig. 13-3, C).
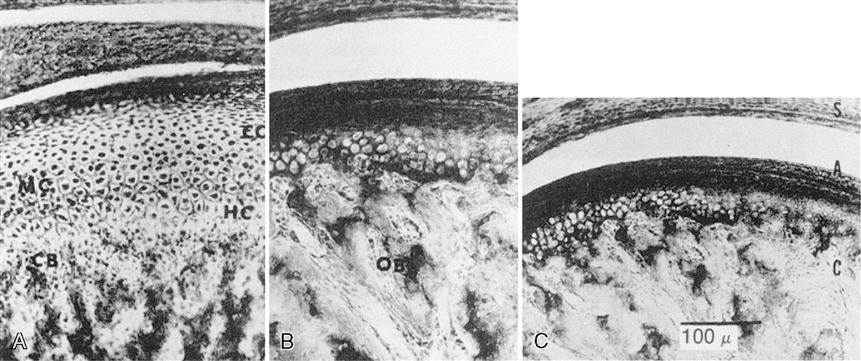
A, The wide band of cartilage that appears during the postnatal period. EC, Reserve cartilage zone; HC, hypertrophy cartilage zone; MC, multiplication cartilage zone. B, Cartilage has thinned considerably. OB, Bone formation. C, Thin cartilage zone underlying the perichondrium in an 18-year-old patient. (S, Synovial tissue; A, articular cartilage; C, cartilage.)
The heads of the condyles and the heads of the long bones differ in that long bones form secondary ossification centers (Fig. 13-4). Secondary ossification centers produce cartilage–bone junctions termed epiphyseal lines, where the lengthening of long bone occurs. No epiphyseal line is formed in the condyles. The heads of the condyles, however, accomplish growth much like that of long bones. Differentiation of new cartilage cells first appears, then cartilage matrix around these cells develops, which is then replaced by bone. Another difference in long bones is that the cartilage cells are organized in long rows as they approach the bony junction, whereas in the condyles the chondroblasts are scattered. The chondroblasts go through similar changes of cell enlargement, cartilage matrix calcification, and bony replacement (see Fig. 13-4). This ability to modify the shape of the condyles through cartilage–bone remodeling allows adaptation to functional stress.
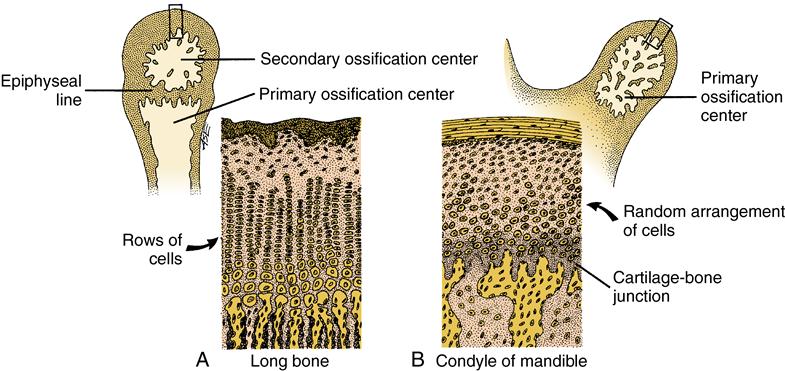
A, Cartilage of a long bone showing straight vertical rows of cartilage cells, young cells to maturing ones, top to bottom. Bone replaces cartilage at the junction of these two tissues. B, Random arrangement of cells in a condyle, which accomplishes same result as rows of cells. As in long bone, at the conclusion of this process in the condyle, bone replaces cartilage at the junction shown.
Temporomandibular fossa
The fossa is composed of an anterior part in the form of an eminence and a posterior part, a depression or cavity on the inferior part of the temporal bone. This fossa is located at the posterior medial aspect of the zygomatic arch (Fig. 13-5). The anterior wall of the fossa is smooth and forms a tubercle in which the condyles slide during articulation. On the posterior wall of the fossa is the petrotympanic fissure.
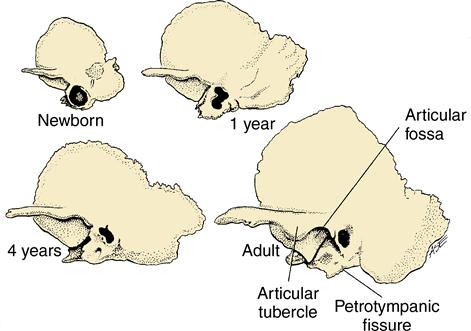
The articular fossa deepens during development to accommodate the growing condylar head as it enlarges laterally.
The contents of the fissure include communications of cranial nerves VII and IX to the infratemporal fossa. A branch of cranial nerve VII, the chorda tympani, runs through the fissure to join with the lingual nerve providing special sensory (taste) innervation to the tongue. The tympanic nerve branches off of cranial nerve IX to pass through the fissure as the lesser petrosal nerve, which passes through the foramen ovale and joins V3 of the trigeminal nerve, synapses in the otic ganglion, and provides parasympathetic innervation to the parotid gland.
This is the junction of the temporal and parietal bones. Some authors report that the origin of elastic fibers, which insert into the posterior part of the disk, is on the posterior wall of this fissure. These elastic fibers may function in retrac/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses