13
Interdisciplinary Collaboration Between Orthodontics and Periodontics
Introduction
Periodontal diagnosis
History taking, clinical and radiographic examination
History taking
Clinical examination
Radiographic examination
Screening for periodontal disease
Local factors predisposing to periodontal therapy
Timing of ortho-perio treatment
Periodontal therapy
Preventive therapy
Non-surgical mechanical therapy
Local and systemic antimicrobial therapy
Surgical therapy
Surgical elimination or reduction of deep pockets
Mucogingival and aesthetic surgery
Augmentation of attached gingiva and root coverage
Regeneration and reconstruction of the interdental papilla
Gingivectomy and clinical crown lengthening
Frenectomy (frenulectomy)
Fibrotomy
Exposure of impacted teeth according to periodontal concepts
Regenerative surgical therapy
Supportive periodontal treatment
Ortho-perio and multidisciplinary clinical cases
Case 1
Case 2
Case 3
Case 4
Conclusion
Acknowledgements
References
Introduction
When treating adult patients, the periodontist’s awareness of the benefits of orthodontics is as important as the orthodontist’s ability to recognize which of his or her patients requires a referral, a periodontic diagnosis and possible periodontal therapy. It is necessary to identify the periodontal problems that must be kept under control throughout the orthodontic treatment phase. Each orthodontic patient with a healthy periodontium must undergo periodic professional hygiene maintenance sessions. Hence, interdisciplinary collaboration is necessary to achieve an optimal functional and aesthetic therapeutic result.
Advances within periodontal therapy have greatly broadened the horizons of orthodontic treatment, and similarly, the latter has improved the prospects of the results achievable solely with periodontics. This chapter provides an overview of the fundamental principles necessary for the understanding of the periodontist’s role in interdisciplinary treatment, followed by some examples illustrating the range of possible combined treatments in which interdisciplinary work resulted in a more efficient and/or aesthetically satisfying therapeutic outcome.
It is obvious, however, that often there is no choice: the collaboration may prove to be indispensable in cases in which overlooking this is associated with the risk, if not the certainty, of further compromising previously reduced periodontal support of some teeth. When considering a combined treatment plan, it is important to standardize the procedures that allow for correct planning, independent of whether the patient has first been seen by the orthodontist or by the periodontist (Melsen and Milano 1993a,b). At the appointment when the treatment decision is to be made, it is essential that all the team members are involved and the patient too, within the teamwork approach. This could be an ideal moment to explain to the patient the necessity of supportive periodontal treatment before, during and after orthodontic therapy.
Periodontal Diagnosis
Periodontitis is defined as a multifactorial disease that is initiated by microbial dental plaque accumulation but whose progression and form are influenced by specific interactions between genetic susceptibility and environmental factors (Tonetti 1998; Kinane 1999). The periodontal status of each individual undergoing an orthodontic check-up or therapeutic visit must be evaluated and kept under control.
History Taking, Clinical and Radiographic Examination
History Taking
During the periodontal visit, data regarding general medical condition, dental and periodontal data must be collected in order to correctly establish the periodontal diagnosis and determine any subsequent therapy required. In addition a subjective analysis of the patient is performed compiling a ‘problem list’ and evaluating his/her capacity for compliance.
A comprehensive collection of data may reveal the presence of risk indicators with either a high or a low predictive value. The predictive value of some risk factors, such as diabetes, smoking and the presence of certain types of bacteria found in dental plaque – Porphyromonas gingivalis, Tannerella forsythensis (Bacteroides forsythus) and Actinobacillus actinomycetemcomitans – is supported by evidence. Other variables, such as age, race, environment, stress, nutrition, genetic predisposition, systemic disease, and immunodepression, are considered to be probable risk factors (Offenbacher 1996; Zambon 1996; Tonetti 1998; Kinane 1999; McGuire and Nunn 1999; Taylor 2001; Meisel et al. 2002; Ezzo and Cutler 2003; Nunn 2003).
Clinical Examination
The clinical examination evaluates:
- Number, status and position of present teeth
- Level of oral hygiene, plaque index and bleeding score
- Probing depth and furcation probing
- Presence of hypertrophy and/or gingival recession
- Presence and degree of tooth mobility and migration.
A probe is inserted in the gingival sulcus of each tooth with approximately 20–25 g of pressure. In absence of inflammation, the application of this pressure should not result in the probe penetrating the connective tissue (Polson et al. 1980; Caton et al. 1981; Sild et al. 1987a,b). Probing thus demonstrates the loss of clinical attachment and furcation involvement and is a measure of periodontal pocket depth and gingival recession.
Deep pockets increase the risk of the progression of periodontitis (Armitage 1996). The bleeding score, if repeatedly positive during periodic probing, has a high predictive value for the risk of further attachment loss. If on the contrary, it is repeatedly negative, it is a valid confirmation of stable periodontal health. The absence of supragingival plaque is highly indicative of stable periodontal health (Armitage 1996).
Physiological tooth mobility is about 0.2 mm (more or less 50%). Tooth mobility is expressed using the following mobility index:
0 = normal mobility
1 = horizontal mobility up to 1 mm
2 = horizontal mobility >1 mm
3 = horizontal and vertical mobility
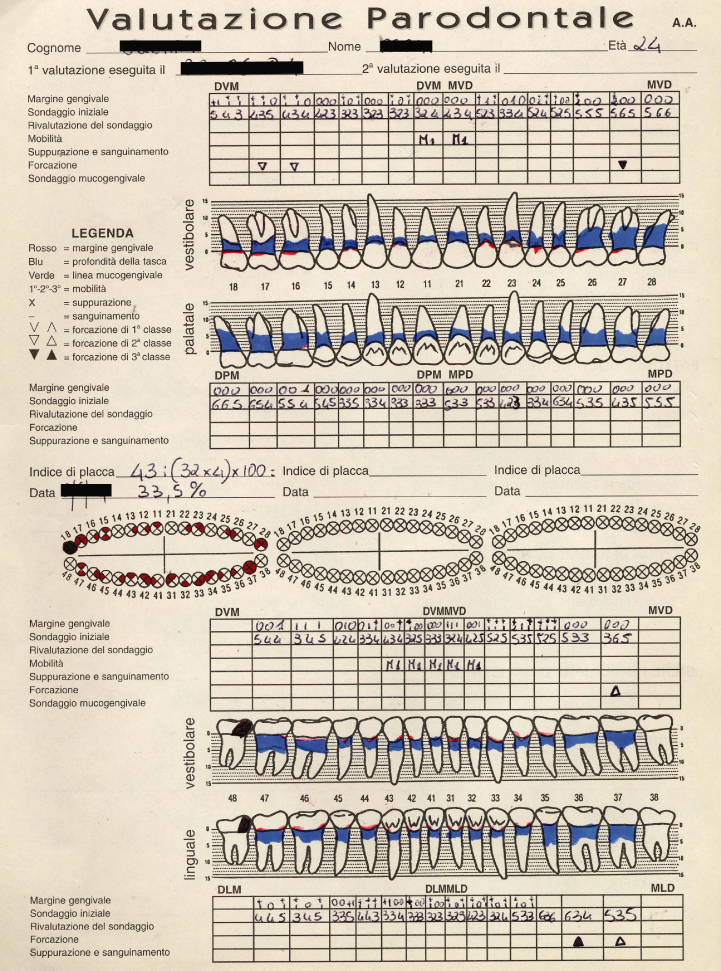
Tooth mobility and migration can be provoked by occlusal trauma, presence of edentulous spaces, unbalanced intraoral forces, such as altered tongue and/or lip pressure, and/or significant loss of supporting periodontal tissue. All information collected must be transferred to the periodontal clinical chart (Fig. 13.1).
Fig. 13.1 Example of a periodontal chart.
Radiographic Examination
A complete periapical radiographic examination using the Rinn centring device is usually undertaken to evaluate the level of alveolar bone and the presence of root resorption. This examination also indicates the space occupied by the periodontal ligament, the lamina dura, the periapical region and the excessive proximity of roots.
The radiographic examination should always be correlated with the clinical examination, which in itself is insufficient for a diagnosis, given its low sensitivity and the lack of correlation between the measurement of the level of clinical attachment and the radiographic height of the bone. This leads to an underestimation of the severity of the periodontal defects (Hammerle et al. 1990; Akesson et al. 1992).
Screening for Periodontal Disease
Even if it may not seem relevant to describe probing techniques at this point, it is useful to remind the orthodontist of the screening test suggested by the American Academy of Periodontology (AAP) and the American Dental Association (ADA) (Anon 1993; 1996); The PSR logo (Periodontal Screening and Recording) is a registered mark of the American Dental Association. This simple, fast test can be implemented routinely in order to immediately differentiate subjects who are periodontally healthy from those who are not, and to periodically monitor their periodontal condition throughout the orthodontic treatment phase.
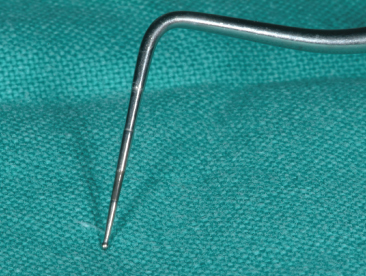
PSR is a simplified method of recording information collected during probing using a special probe (Fig. 13.2) with coloured areas ranging from 3.5 to 5.5 mm. The mouth is divided in six segments as shown in Table 13.1. Only the highest measurement of severity is recorded in each sextant utilizing a series of codes:
- 0: the coloured portion of the probe is completely visible
- 1: the coloured portion of the probe is completely visible but detects bleeding upon probing
- 2: the coloured portion of the probe is completely visible but it detects the presence of calculus and/or restoration overhang, either with or without bleeding
- 3: the coloured portion of the probe is only partially visible at the maximum probing point of the sextant, indicating the presence of a pocket between 3.5 and 5. 5 mm in depth
- 4: the coloured portion of the probe disappears completely at the maximum probing point of the sextant, indicating the presence of a pocket >5 mm in depth.
Table 13.1 The six dental arch segments for periodontal recording
| 1.8–1.4 | 1.3–2.3 | 2.4–2.8 |
| 4.8–4.4 | 4.3–3.3 | 3.4–3.8 |
Fig. 13.2 PSR probe: the coloured portion of the probe facilitates immediate reading.
An asterisk (*) is placed next to the code for each sextant, when there is:
- furcation involvement
- dental hypermobility
- mucogingival pathologies
- recessions >3.5 mm.
Patients in whom code 0 in recorded for all areas should commence with a, or continue their previous, prevention programme. Patients with areas in which codes between 1 and 2 without asterisks (*) are recorded, should proceed with a prevention programme including oral hygiene instruction, and removal of sub- and supragingival plaque, calculus deposits and restorations with marginal overhang. Patients presenting areas with codes between 3 and 4 or areas with asterisks (*) require a more detailed periodontal examination, including a comprehensive periodontal chart recording and a complete evaluation of the periapical status. In more complex cases, laboratory investigations should be requested: microbiological and/or haematological, or investigations useful for identifying genetic susceptibility to periodontitis (Cortellini et al. 1999).
Local Factors Predisposing to Periodontal Therapy
Local factors, relating to either the anatomy and morphology of teeth or dental restorations which are considered as a predisposing to periodontal disease, are as follows:
- Factors relating to tooth anatomy and morphology:
- proximity of the roots, particularly between upper molars
- close proximity between the cementoenamel junction (CEJ) and the roof of the furcation area
- ectopic enamel at the furcation
- ridges of dentine covered with a thin layer of cement at the level of the furcation
- reduced divergence of the roots (Fig. 13.3)
- lingual grooves in the anterior teeth (Fig. 13.4)
- severe crowding (Fig. 13.5)
- Factors relating to dental restorations:
- overhanging fillings
- porous restorative materials capable of holding greater amounts of plaque
- incongruous prosthetic restorations (Fig. 13.6).
Fig. 13.3The mesial and distal buccal roots of 26 are slightly divergent, creating a situation that is anatomically favourable for rapid destruction of the deep bone once periodontitis sets in.
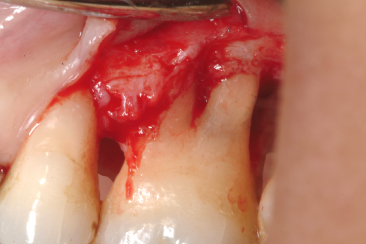
Fig. 13.4 A palatal sulcus that extends beyond the cementoenamel junction favours the accumulation of plaque and the formation of defects of the deep bone. The presence of a bone defect is evident once a flap is raised.

Fig. 13.5Severe crowding in the lower arch creates an anatomical environment that is favourable for plaque accumulation and makes maintenance of hygiene more difficult and laborious. A raised flap showing severe loss of deep bone in a patient who neglected practising dental hygiene at home and professionally.

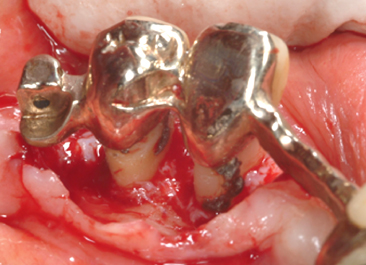
Fig. 13.6The thick and irregular edges of the prosthetic crowns constitute an obstacle for oral hygiene maintenance and facilitate the accumulation of plaque and formation of calculus.
Timing of Ortho-Perio Treatment
While establishing the treatment plan, it is important to define the treatment to be performed by the periodontist prior to starting orthodontic treatment as well as during and after orthodontic treatment. This should be done both to be able to perform tooth movement in a healthy environment and to optimize the function of the existing periodontal support and to enhance the final aesthetic result (Mathews and Kokich 1997).
Procedure Performed Prior to Orthodontic Treatment
- Oral hygiene motivation
- Prophylaxis or therapy to control inflammation
- Surgery to eliminate deep pockets
- Augmentation of attached gingiva
- Frenulectomy (frenectomy) and frenulotomy (frenotomy)
- Elimination of gingival clefts
Procedures Performed During Orthodontic Treatment
- Prophylaxis to control inflammation
- Surgical exposure of impacted teeth according to periodontal concepts
- Fibrotomy and curettage during forced eruption
Procedures Performed During And/or Post Orthodontic Treatment
- Prophylaxis to control inflammation
- Clinical crown lengthening
- Gingivoplasty
- Root coverage
Procedures Performed Post Orthodontic Treatment
- Supportive therapy.
The above outline is only indicative, as all decisions depend on the individual diagnosis and tailoring the timing of treatment to each patient’s unique situation to achieve both the functional and aesthetic therapeutic goals. When labial orthodontic movement is planned, if needed a periodontal surgical procedure to increase the thickness of the attached gingiva prior to initiating orthodontic treatment can serve to optimize the final result. The same holds true for cases where tooth migrations have resulted in spaces opening and loss of the papilla and eventually a reduction or total lack of attached gingiva. In these cases surgery is performed before orthodontic closure of the spaces. If only the orthodontic closure or only surgical procedures are performed, the aesthetic and/or functional result will be compromised (Figs. 13.7–13.9).
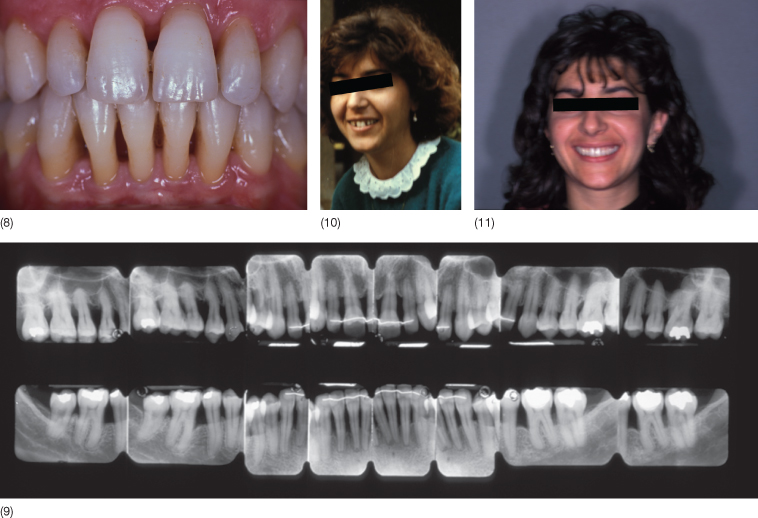
Fig. 13.7 (1,2) A 22-year-old woman with a midline diastema, treated in 1982. The patient had extremely poor oral hygiene with plaque and calculus, specially in relation to the lower incisors. Three upper premolars were missing and the space on the right side was partially closed. The patient stated that the midline diastema was increasing in size. (3,4) Motivation, scaling and root planing have led to a distinct improvement in the oral hygiene. There is gingival recession in relation to the lower incisors with loss of attachment and interdental alveolar bone, and reduction of the interdental papilla height. (5,6) With orthodontic treatment, space was opened for one tooth in the upper right premolar region with closure of the medial diastema. After prosthetic rehabilitation, the upper and the lower incisors were splinted. The gingival recession on 31 and 41 with loss of interdental periodontal tissue was still present, as was the lack of attached gingiva and the presence of a frenulum. (7,8) An autogenous free soft tissue graft was placed in order to eliminate the frenulum and to increase the thickness and the quantity of the attached gingiva. (9) Now the case is finished. (10) At 10 year follow up the overall status is still mantained. (11) The clinical situation 22 years later.
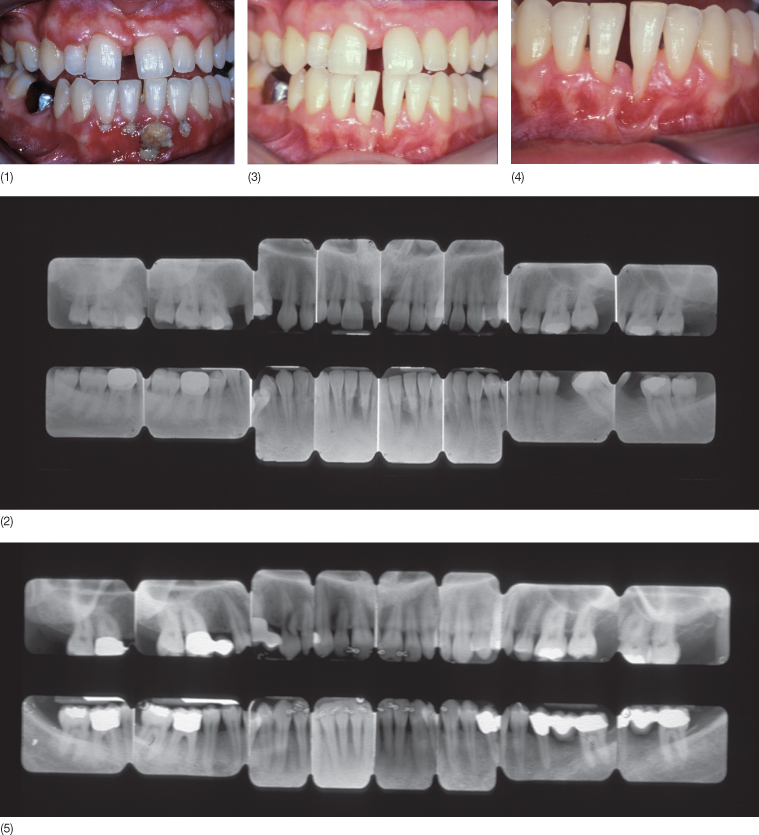
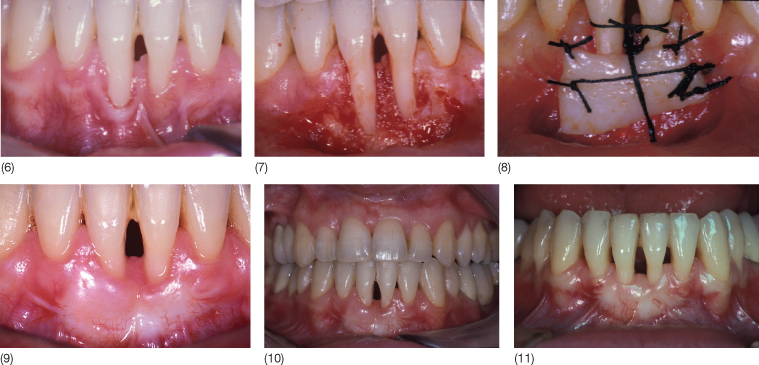
Fig. 13.8 (1) A 44-year-old woman treated in 1995 complained of a progressively increasing diastema between the lower incisors with recession and attachment loss at the interproximal surfaces. The diastema made plaque removal more difficult. (2) After being motivated, and after the scaling and root planing, the patient became more attentive regarding hygiene maintenance. At the end of the orthodontic treatment, the occlusion and the aesthetics were restored. Bonded retainers from canine to canine were fitted in both arches. At the end of the treatment a redistribution of the interdental periodontal tissue was noted, although, due to the thin marginal tissue, root coverage and normal papillary height were not achieved.
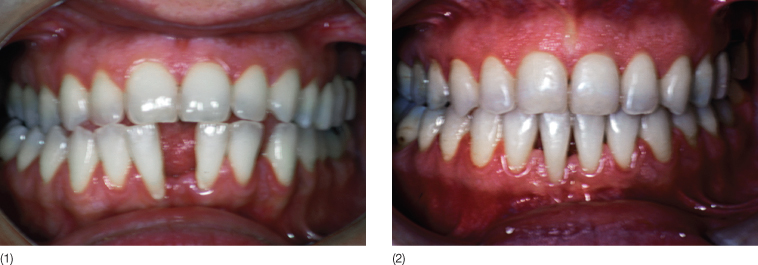
Fig. 13.9 (1,2) A 33-year-old woman (1988) complained of an increasing diastema between the lower incisors with speech problems and spraying of saliva through the wide open space. The lower first molars had been extracted a long time ago with mesial migration of second molars. There was total absence of attached gingiva, thin gingival margins and gingival recession with loss of interdental papilla height. (3,4) After patient motivation, scaling and root planing, a free gingival graft was placed to increase the thickness of connective tissue before orthodontic treatment to be “squeezed” during the orthodontic closure of the diastema. In this patient, periodontal surgery alone would be insufficient to obtain root coverage and papilla height. (5,6) Orthodontic treatment was performed only in the lower arch, as elimination of the traumatic occlusion between the lower and upper incisors was sufficient to allow spontaneous closure of the upper diastema. (7) At near completion of the orthodontic treatment, complete root coverage was obtained and the papilla filled the interdental space up to the cementoenamel junction, but total recovery of the papilla was not possible due to the triangular shape of the lower incisors. (8) Improvement of the periodontal situation was maintained with a lingual retainer.

In patients treated with guided tissue regeneration (GTR), simultaneous or almost simultaneous orthodontic treatment may lead to an accentuation of the results (Fig. 13.10).
Fig. 13.10 (1) A 42-year-old man presenting in 1995 with an retained upper canine. (2–4) When the flap was raised, no alveolar bone was seen on the buccal aspect of the root of the canine. Guided tissue regeneration periodontal therapy was performed, using a resorbable collagen membrane (Paroguide®) and a layer of Biostite® between the root and the membrane. (5) A bracket with a gold chain was bonded to the crown and the flap sutured. (6) At the reopening it is possible to see the new periodontal tissue. (7) An apically positioned flap was carried out to improove the attached gingiva. (8) The treatment is almost finished. (9–10) Clinical and radiographic situation 10 years later (2005).
Periodontal Therapy
Preventive Therapy
This includes oral hygiene education and prophylaxis for inflammation control. Orthodontic treatment in adult patients should only be initiated in the presence of a healthy periodontium. Based on the premise that the most important aetiological agent of periodontitis is plaque, one must consider that the orthodontic appliance increases the risk of plaque accumulation and the difficulty of performing daily oral hygiene at home. Changes in the quality of the microflora in periodontal sites around orthodontic bands have been described in literature (Diamanti-Kipioti et al. 1987; Huser et al. 1990; Turkkahraman et al. 2005). Therefore, in order to avoid complications during orthodontic treatment, it is important to:
- Give detailed oral hygiene instructions. Toothbrushing can be made more effective through the use of an electric toothbrush with a circular head (Sicilia et al. 2002; Heanue et al. 2003), supplemented with rinsing with chlorhexidine to control gingivitis (Sicilia et al. 2002; Heanue et al. 2003; Sekino et al. 2003). At this time it is opportune to proceed with general oral health behaviour education including motivation and a recommendation to stop or reduce cigarette smoking, avoid or reduce parafunctions and/or residual ‘bad hygiene habits’
- To have quarterly recall visits (Boyd and Baumrind 1992) for professional oral hygiene sessions to control plaque and supra and subgingival calculus
- To arrange recall visits with the periodontist to register probing depth, the plaque index and bleeding score, tooth mobility and gingival recession.
Non-Surgical Mechanical Therapy
Non-surgical mechanical therapy, scaling and root planing, is performed using manual, sonic or ultrasonic instruments to remove plaque, calculus, necrotic cement and bacteria until the root surface is clean, smooth and hard. This serves to obtain and maintain a healthy periodontal state with reduced bleeding and probing depth. After this primary therapy, the patient is re-evaluated and the need for possible surgical therapy is assessed (Heitz-Mayfield et al. 2002) (Fig. 13.11).
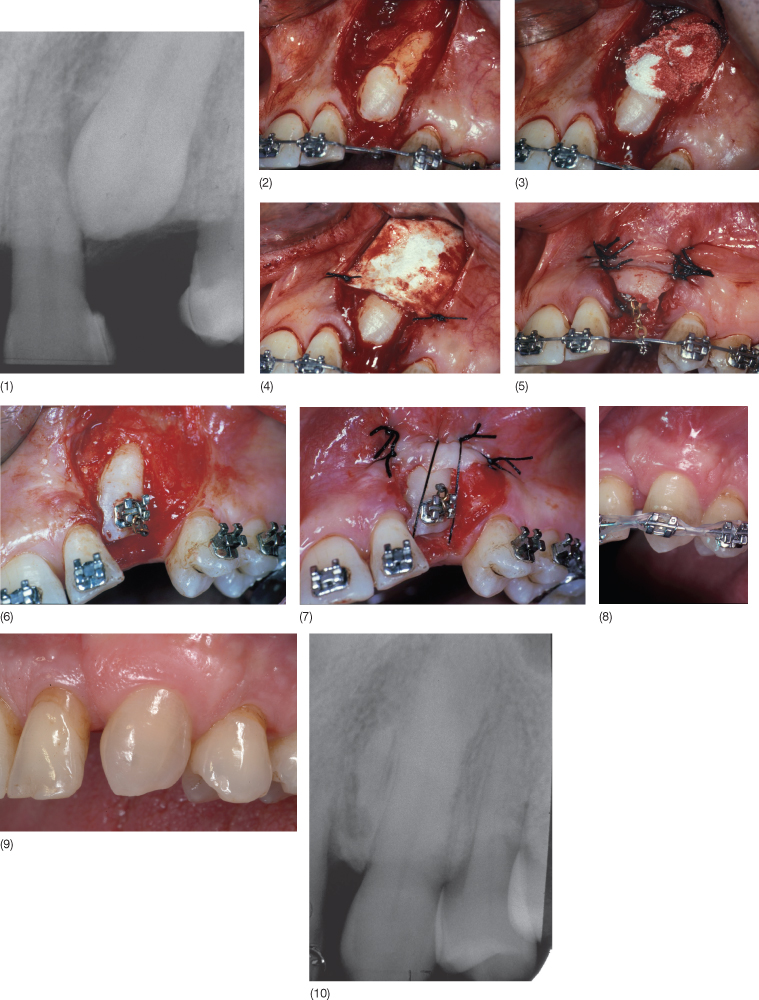
Fig. 13.11 (1–4) In 1986 a 25-year-old woman showed a Class II division 2 malocclusion with deep bite, a deep curve of Spee, a gingival impingement, a periodontal compromised situation and spontaneous migrations. In addition she had also temporomandibular joint (TMJ) symptoms due to the loss of vertical dimension. (5) The initial full mouth radiographic examination shows loss of supporting tissues. (6,7) After patient motivation, scaling and root planing, oral hygiene and periodontal condition improved. The treatment plan consisted of orthodontic treatment, including intrusion of the upper incisors. (8) At the end of the combined orthodontic and non-surgical periodontal therapy. (9) Radiographs at the end of treatment. Supportive periodontal therapy was strictly followed. (10,11) The smile before and after interdisciplinary treatment.

Local and Systemic Antimicrobial Therapy
Antimicrobic therapy, administered systemically or applied locally as a support for mechanical therapy, may be prescribed by the periodontist based on the specific diagnosis formulated (Herrera et al. 2002; Haffajee et al. 2003; Hallmon and Rees 2003, Hanes and Purvis 2003).
Surgical Therapy
Surgical Elimination or Reduction of Deep Pockets
If the periodontal status is controlled, orthodontic tooth movement in adults can be performed even in the case of advanced loss of marginal periodontium (Artun and Urbye 1988; Zachrisson 1997). Before initiating orthodontic treatment, it is necessary to perform periodontal surgical therapy on teeth that, at the completion of preventive therapy and root planing, have deep residual pockets (>4–5 mm) with persistent clinical signs of disease.
The specific goal is to eliminate pockets and to obtain a shallow sulcus in order to facilitate plaque control. According to Armitage (1996), when the pocket depth is 5 mm or more there is a high risk of relapse. The surgical procedures for pocket reduction require access flaps as the modified Widman flap, while the techniques for pocket elimination include gingivectomy and the apically positioned flap, with or without osseous resective surgery. When performing a gingivectomy, a gingivoplasty is also performed (Goldman 1951), aiming to eliminate suprabony pockets to facilitate access for root planing and to establish a gingival architecture that is favourable for maintenance.
Access flaps consist of lifting of a flap that preserves marginal gingival tissues and gives access to root planing instruments and removal of the granulation tissue. In this way, healthy tissue is adapted to the root surface and sutured. The modified Widman Flap (Ramfjord and Nissle 1974) consists of a vestibular and palatal incision of approximately 1 mm from the gingival margin, which is highly scalloped in such a way that the maximum amount possible of interdental gingiva is included interproximally in the flap. This ensures adequate coverage of interproximal bone while suturing. Having eliminated the collar of gingival tissue from around the alveolar bone, the surgeon proceeds with root planing and curettage of the bone defects. Finally, the flaps are positioned on the alveolar bone and sutured (Fig. 13.12). The apically positioned flap (Friedman 1962) is a mucoperiosteal internal bevelled flap, positioned at the level of the bone crest. This permits pocket elimination and keratinized tissue preservation and allows proceed/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


