15
Patients with Temporomandibular Joint (TMJ) Problems
Orthodontics and dysfunction
Controversy in the literature regarding TMD and occlusion
Treatment and TMD
Treatment of clicking joints
Orthodontic treatment of patients with TMD
Organization of the treatment
Conclusion
References
Orthodontics and Dysfunction
The relationship between orthodontic and functional problems has been the focus of many studies. A PubMed search with the keywords ‘malocclusion’ and ‘TMD’ (temporomandibular dysfunction) resulted in 1664 references and 1253 references were registered under the keywords orthodontics and TMD, but a search for randomized controlled trials reduced the number of published papers to 65. This reflected the fact that most papers were case reports and several questions remain unanswered. Does malocclusion lead to craniomandibular disorder? Does orthodontic treatment play a role in the treatment of craniomandibular disorders? In other words, can TMD be considered an indication for orthodontic treatment?
The relationship between craniomandibular disorders and malocclusion is rated highly by some authors while others claim that the presence of a malocclusion has no impact on the risk of TMD (Luther 2007a,b). One explanation for this discrepancy is the difference between morphological occlusion and functional occlusion. The patient in Figure 15.1 with a Class I occlusion complained of muscle pain and tension headache. When the patient was given a flat occlusal splint, her occlusion changed from neutral occlusion to distal occlusion. She clearly had a dual bite and an electromyographic examination demonstrated significantly higher muscle activity in the contact position than in the position in which the patient was occluding when she was asked to bite together. Radiographs, taken in the two different occlusion positions, verified that the mandibular condyles were displaced forwards and downwards when the patient was occluding in Class I intercuspation and were centred when she attempted the retruded contact position. The fact that patients are generally registered in maximum intercuspation, which does not necessarily represent a mandibular position that is in harmony with the functional occlusion may be a confounding factor when assessing the correlation between occlusion and TMD (Tallgren et al. 1979).
Fig. 15.1 (1) Study casts in two different occlusion positions. The cast on the right side displays the spontaneous occlusion observed when the patient is asked to bite together, and that to the left displays the posterior contact position that occurs after a period of wearing a flat splint. (2,3) Clinical views of the same situations.

The above mentioned example illustrates but one of the methodological problems which may contribute to the conflicting notions regarding malocclusion and oral function. As the functional deviation may be related to the deterioration of the dentition, adult patients with TMD should be asked to explain their version of the development of the problem. This also applies to all aspects of oral function such as parafunctions and bruxism.
Whereas the general relationship between occlusion and TMD is controversial, there is general agreement that misarticulation is more frequent in patients with certain types of malocclusion, such as excessive overjet, lateral crossbite and anterior open bite (Johnson and Sandy 1999; Pahkala and Qvarnstrom 2002). Misarticulation can be evaluated subjectively by the orthodontist, by a speech therapist (Laine 1992) or objectively by an electro-acoustic sound analysis (Mehnert 1987). In cases in which misarticulation is diagnosed, speech training rarely helps the patient unless the morphology does allow for normal function. Mastication can be evaluated either subjectively by asking the patient to explain the problem or objectively by asking the patient to chew on a standard object (Huggare and Skindhoj 1997). Lip activity during swallowing and the presence or absence of tooth contact during swallowing can be evaluated clinically. Cinefluorography studies have been used to describe the tongue movement and its adaptation to morphology (Hiiemae and Palmer 2003; Kawamura et al. 2003).
Analysis of jaw movement and palpation of muscles should precede the analysis of the occlusion, as detailed knowledge of the occlusion may bias the registration of the signs and symptoms of TMD. The muscles included in the examination are usually the temporal, masseter, digastric and the pterygoid muscles. Jaw movement can be evaluated clinically or registered by means of jaw tracking equipment (Simonet and Clayton 1981; Piehslinger et al. 1991). It should be recorded whether the opening movement is symmetrical and smooth, asymmetrical or irregular, and the presence of any sounds and clicking should be noted. If clicking is present it should be noted whether it occurs at the same spot during opening and closing. Clicking during opening may reflect an anterior disc displacement. The click occurs when the condyle is repositioned on to the disc and the click during closing occurs when the condyle slips off the disc again (disc displacement with reduction). The click therefore does not occur at the same spot during opening and closing. In a patient in whom the click is at the same spot during opening and closure of the mouth, it is most likely a symptom of a disc that is ankylosed to the articular eminence of the joint fossa. (Bumann and Lotzmann 2002).
The range of lateral movements and protrusion should likewise be noted. A limitation especially in protrusion may be a sign of a permanently forward displaced disc. In the case of a midline discrepancy, this may either be reduced or increased by opening (Fig. 15.2). In the patient with a skeletal asymmetry the asymmetry will increase during opening, the mandible will deviate towards the short side or to the side with the least translation. If the midline is centred during maximum opening, this is a sign of a forced bite and closure can proceed in two different ways: either starting with symmetrical closure until the initial tooth contact position is reached, after which deviation towards maximal intercuspation takes place; or closure that proceeds towards a midline discrepancy in a smooth manner. In the first case, the sensory input from the primary contact is still present and the midline discrepancy can most likely be corrected by removal of the primary contact. In the latter case, the neuromuscular pattern has adapted to the malocclusion and the parasympathetic input from the occlusion should be removed before the structural position of the mandible can be established. This can be done with a flat occlusal splint. The importance of determining the condylar position in the orthodontic diagnosis has been underlined by several authors (Gianelly 1989; Roth 1995; Johnson and Sandy 1999; Cordray 2002).
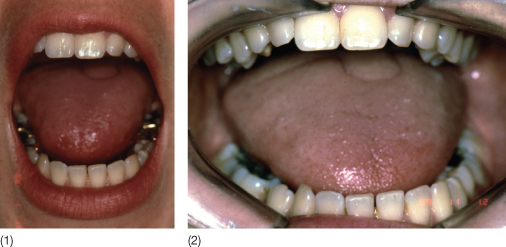
Fig. 15.2 (1) Normal opening movement with midlines coinciding. (2) Limited opening movement with more deviation towards the left side.
Controversy in the Literature Regarding TMD and Occlusion
The controversies regarding the relationship between occlusion and TMD may be related to the design of the studies as well as the reproducibility and validity of the parameters. In addition, the specificity and the sensitivity of the applied methods may have an impact. The methods used to establish the presence of a TMD have involved questionnaires, clinical analyses and instrumental analyses. The result of questionnaires and the clinical analyses are both subject to fluctuation over time, since the cause of TMD is generally being accepted as multifactorial (Dworkin and LeResche (1992) (see Chapter 16).
The reproducibility of jaw tracking, however, has proved to be very high when computerized methods are used. Kimmel et al. (1986) performed axiographic and sirognathographic analysis in young adults with normal occlusion who had never had TMJ symptoms and had clinically normal opening capacity. In 7 of the 30 test subjects, the axiographic registrations indicated internal derangement in one or both joints and six were confirmed by the sirognathographic registration. Repeated examinations gave identical results, indicating good reproducibility but low specificity as there was a large number of positive findings in healthy persons. The sensitivity was, on the other hand, good, as clinical findings were always confirmed by the jaw tracking method.
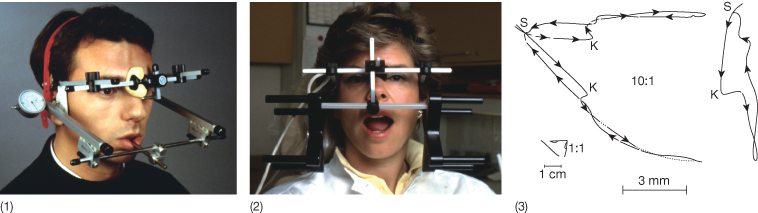
Instrumental methods can thus be used to follow the development of the pathology in a joint but not as a diagnostic tool. The validity of the condylar movement could also be questioned, as the sensor moving was not localized to the condyle and it is doubtful whether a patient is able to perform natural movement of the mandible with the tray in the mouth (Fig. 15.3). In the case of sirognathography, a small magnet was glued to the lower incisors and the displacement of the magnet during mandibular movement was picked up in a magnetic field generated by an appliance placed adjacent to the cheeks of the patient (Fig. 15.3). Without doubt, the advantage of both methods is that the results can be presented in a digital form or graphically in all three planes of space, whereby changes occurring over a period of treatment or development of a disease can be followed (Fig. 15.3). When jaw tracking was used to study the influence of occlusion on condylar movement patterns, it was refuted that there was a correlation between occlusion and joint pathology, as clinically healthy patients were diagnosed as having internal derangement.
Fig. 15.3 Jaw tracking devices. (1) Classic axiograph. (2) In sirognathography, the movement of a small magnet glued to the lower incisors is followed in three planes of space. (3) Enlarged image obtained by the jaw tracking device revealing that the clicking is related to a medial displacement of the condyle.
The parameters reflecting occlusion may also influence the result of studies relating occlusion to TMD. Normally, the morphological occlusion is expressed using Angle classification or selected features such as overjet >6 mm, overbite >5 mm, etc. Gianniri et al. (1991) performed a study with the purpose of analysing the relationship between occlusion and TMD. Based on systematic screening, 30 16-year-old individuals with significant subjective symptoms and clinical signs of TMD were matched with individuals of the same age, gender and with identical occlusion and no symptoms and signs according to the form filled in by the community dentistry team. In addition to the parameters reflecting TMD and occlusion, the distribution, number and intensity of occlusal contacts were noted by means of a photo-occlusal method. The study demonstrated that although the occlusion was registered as identical, both the distribution and intensity of the occlusal contacts differed between the two groups. In the population without symptoms, the occlusal contacts were distributed symmetrically whereas they were asymmetrically distributed in the group with symptoms. In addition, the intensity of the occlusal contacts when evaluated by photo-occlusion differed. The intensity of individual occlusal contact was significantly higher in the group with symptoms than in the healthy group. This indicates that the method by which the occlusion is registered influences the results of the studies evaluating the relationship between occlusion and TMD.
Treatment and TMD
Treatment of TMD can focus on the patient as a whole (see Chapter 16), on the joint or on the occlusion. Regarding treatments focusing directly on the joint, intra-articular surgery or lavage has been performed as well as intra-articular injections of various substances (Dolwick 2007). Bertolami et al. 1993 divided 120 patients with TMD into two groups, one of which had injections of 1% sodium hyaluronate in physiological saline and the other only physiological saline. The result was clearly in favour of the sodium hyaluronate group, both when evaluated by the Helkimo index and with a visual analogue scale used for the level of pain and noise during movement. Glucocorticoid injections have been recommended (Kopp et al. 1985, 1987) in spite of the detrimental effect discussed already by Chandler and Wright in 1958 (Chandler and Wright 1958). The long-term results of glucocorticosteroid injections were evaluated as positive in 16 out of 19 patients examined. However, the results of the 8-year follow-up may not necessarily solely represent the effect of the cortisone injection (Wenneberg et al. 1991).
Whether orthodontics plays a role in treatment of patients with TMD depends on the probability that changing the occlusion will have an impact on the symptoms. This can be evaluated by the use of a splint. These splints may be soft or hard, balanced flat, repositioning or stabilizing splints. Comparisons of the results of treatment with splints clearly reflect the multifactorial character of TMD. Several studies (Table 15.1) have demonstrated that the type of appliance or splint used was not important. All splints were associated with a positive response with regard to the level of pain whereas clicking was less influenced. Most studies have reported short-term results but the few long-term follow-up studies that have been reported have demonstrated that the effect is not permanent in most cases, although the best long-term results seemed to be related to the repositioning splints. A significant effect in the short term was also seen in the control groups and had an obvious influence on the conclusions of such studies. A meta-analysis focusing on the treatment of disc dislocation with reduction confirmed that a repositioning splint was significantly more effective than a flat splint in reduction of both pain and clicking (Santacatterina et al. 1998). However, it could be argued that sample size in all the included studies was limited.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


