Chapter 12
Problem-Solving Challenges in Root Canal Obturation
Problem-solving challenges and dilemmas in obturation of the enlarged, shaped, cleaned, and disinfected root canal system addressed in this chapter are:
“Gutta-percha … for convenience, utility, and harmlessness withal, it is invaluable.”< ?xml:namespace prefix = "mbp" />
“Perhaps there is no technical operation in dentistry or surgery where so much depends on the conscientious adherence to high ideals as that of pulp-canal filling.”
The evolution of root filling materials and techniques has a long and challenging history, but not much has changed in this regard. Gutta-percha, the use of which is credited to Dr. Asa Hill in 1847, is still being used to obturate prepared root canals.
Dr. Neil Postman, a noted author and professor of media and communications at New York University, once posed a very useful question in an interview on PBS: “When confronted with a new technology, whether it’s a cellular phone or high-definition television or cyberspace or Internet, the question, the one question, should be What is the problem to which this technology is the solution?” Later in the interview, he concludes with the observation, “It is very easy to be swept up in the enthusiasm for technology, and of course all the technophiles around, all the people who adore technology, are promoting it everywhere you turn.”
Turning these concepts to root canal obturation, pastes were developed to speed the tedious process of obturation and more effectively move filling material into canal irregularities.
Yet as we enter the second decade of the 21st century, gutta-percha still dominates. The gutta-percha cones that have been available for decades and gutta-percha on core carriers that have been used extensively over the past 20-plus years are still the filling material of choice globally—used, of course, with some type or root canal sealer or cement and compacted into the prepared root canal space.
When all the more recent developments in root canal obturation materials and techniques are considered, there appear to be recurring themes that beg Dr. Postman’s question: What is the problem to which this technology is the solution? The list includes developing ways to manage the intricacies of the root canal system, ensuring complete obturation, sealing the canal system, providing a radiographic appearance of the filled root that signifies to the clinician they have achieved their goal (and, of course, provided that needed signature of expertise), and strengthening the root canal to prevent potential fracture during function (see
Root Canal Sealers: Their Role and Use
A root canal sealer or cement is essential with any gutta-percha technique, just as an etching agent and bonding material are required when using resin-filling techniques.
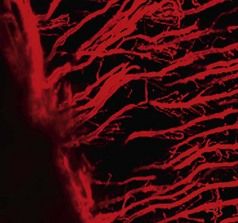
FIGURE 12-2 Sealer penetration into the dentinal tubules (Rhodamine B dye).
(Courtesy Ronald Ordinola-Zapata, São Paulo, Brazil.)
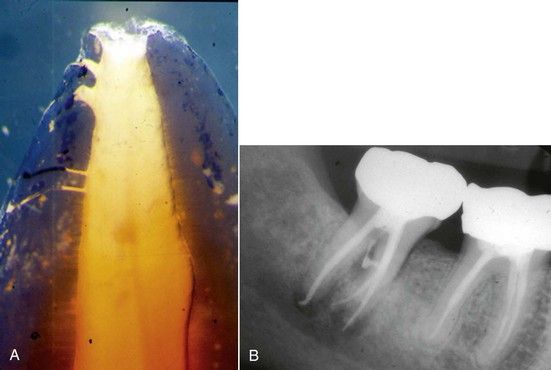
FIGURE 12-3 A, Sealer penetrating into dentinal tubules and accessory communications in a tooth that has been demineralized and cleared for visualization. B, Mandibular molar showing the movement of root canal sealer into accessory communication into the furcation.
Ideally, all sealers should be antimicrobial and biocompatible; some sealers or portions of substances within them may be absorbed when exposed to tissues and fluids.
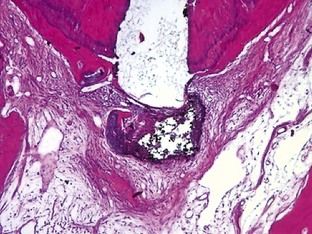
FIGURE 12-4 Photomicrograph showing chronic inflammation surrounding the extrusion of root canal sealer beyond the root canal (H&E ×10).
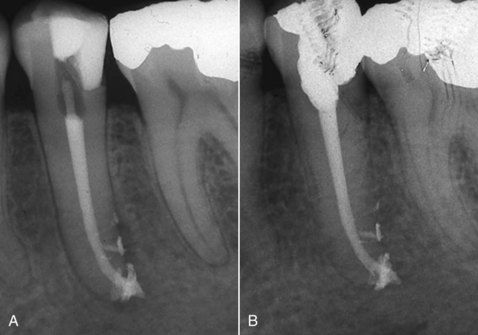
FIGURE 12-5 A, Obturated mandibular premolar that exhibits multiple accessory communications and extrusion of sealer. B, Six-month reexamination shows what most clinicians would consider as healing; however, healing cannot occur with the presence of the irritating sealer that contributes to long-term chronic inflammation.
Sealers are generally grouped based on their primary component or chemical make up (e.g., zinc oxide eugenol, polyketone, epoxy, calcium hydroxide, silicone, glass ionomer, or resin based). Ideally, none of these sealers should be extruded beyond the end of the root canal, because chronic inflammation may persist (see
Gutta-Percha Obturation Techniques
Popular methods of canal obturation are lateral compaction, vertical compaction, thermoplasticized gutta-percha injection techniques, and thermoplasticized core-filler techniques.
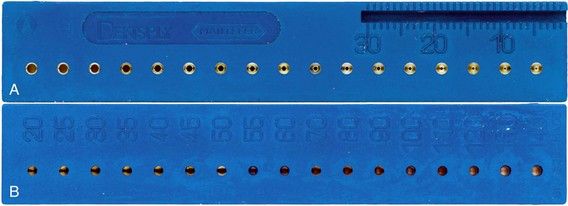
FIGURE 12-6 A and B, Measuring gauge is shown for both length and apical sizing.
(Courtesy Dentsply Maillefer,
Lateral Compaction
A spreader that reaches the working length or within 0.5 mm is chosen and fitted in the canal (
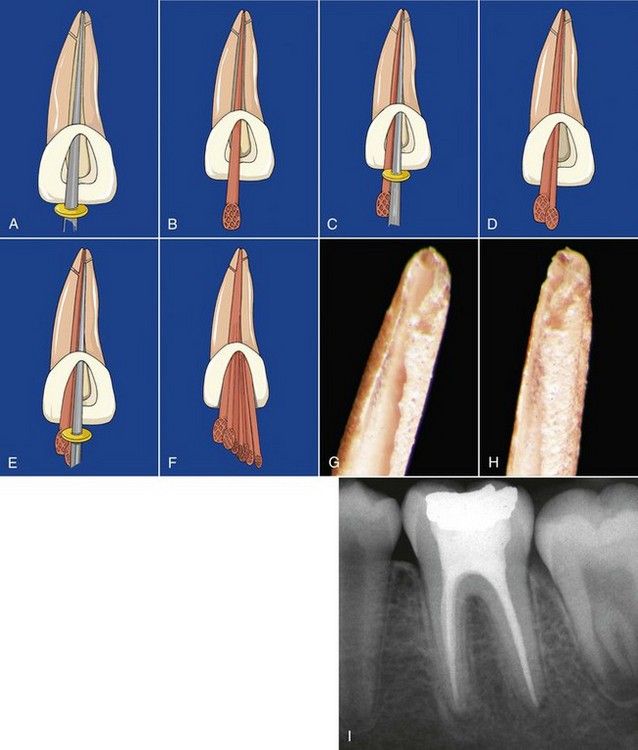
FIGURE 12-7 A, Fit of the spreader is visualized to the working length in a prepared canal. B, Fitting of the master cone to the working length. C, The spreader is placed alongside the master cone to length to compact the apical portion of the cone and seal the canal. D and E, Adding additional cones are followed by compaction apically and laterally. F, Finished compaction. G and H, Adapting the master cone to the root canal walls and apical preparation when the spreader is placed to the working length during lateral compaction. Failure results in a single uncompacted master cone in a sea of cement—an invitation to failure! I, Mandibular molar shows well-adapted and laterally compacted gutta-percha fillings.

FIGURE 12-8 Obturation of a mandibular molar with long, curved canals.
(Courtesy Dr. David P. Rossiter III.)

FIGURE 12-9 Mandibular molar is obturated using the lateral compaction technique; note lateral canal in the distal root.
(Courtesy Dr. David Stamos.)
If the shape of the canal is developed with a hand instrument, the taper usually closely corresponds to a cone that is .02 or slightly larger. Cleaning and shaping is often accomplished using the step-back technique or variation thereof. A .02 master cone is chosen for obturation that provides sufficient taper or space lateral to the master cone for root canal sealer and placement of the spreader to within 1 mm or less of the working length.
If the shape is developed with a rotary instrument at larger taper sizes (.04, .06), the chosen master cone corresponds to the last instrument placed to the working length. The size of the cone may have a specific taper, or it may be a nonstandardized cone (e.g., fine-medium, medium) cut to fit the taper and length of the prepared canal. These cones can be cut to fit into the apically prepared space more accurately using a metallic standardized gauge (see
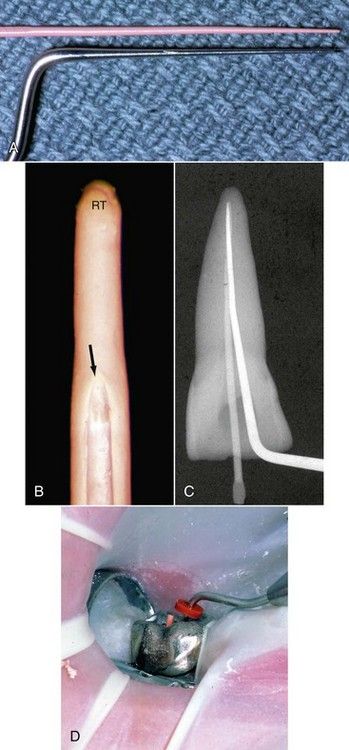
FIGURE 12-10 A, Accessory gutta-percha and resin-bonded accessory cones are chosen based on the size of the compacting instrument. The cones should be slightly smaller. B, Spreader inserted into a root canal only reached to the position of the arrow, far short of the ideal length (RT). Note there is no compaction of the gutta-percha apical to the arrow. C, Spreader reaches to the desired length at the extent of the master cone. D, Spreader reaching the reference point for the working length adjacent to the master cone in a molar tooth.

CLINICAL PROBLEM
Problem
At the point of cone selection, it appears that there is insufficient room for the spreader to extend to the proper depth as described in the preceding section.
Solutions
The interrelationship between the shape of the canal and the technique for obturation cannot be overemphasized. Furthermore, the understanding of the balance between preparation and obturation varies from person to person. It involves such subjective aspects as experience, the “feel” of the canal shape, the “feel” of the cone fit and the “fit” of the spreader. There are a number of objective remedies if there are problems with the fitting of master cone or the fitting of the spreader. For most clinicians, the majority of the problems seem to occur in the mid-root areas. Usually, there is insufficient enlargement of the canal space, but there may be other contributing factors.
To address this issue, there are a number of effective remedies:
Some of these concepts will be revisited in greater detail later in this chapter in the discussion of obturation problem areas in general.

Vertical Compaction
A nonstandardized master gutta-percha cone (master cone taper .02, .04, .06, .08) is chosen to ensure that it has a slightly smaller taper than the prepared root canal space (
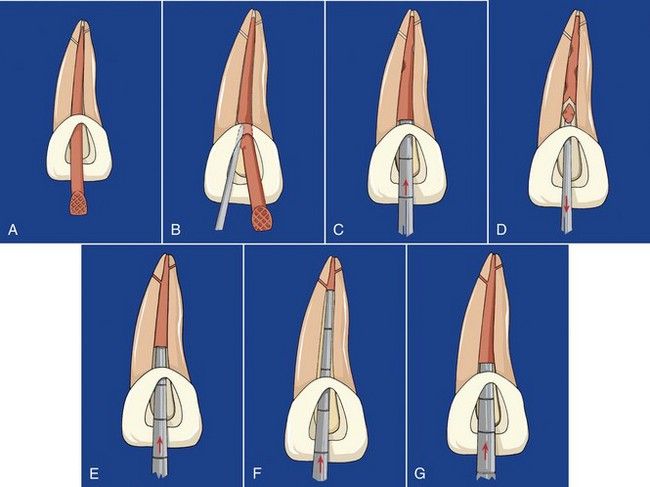
FIGURE 12-12 A, The master cone is fitted for vertical compaction. B, Heated instrument is used to sever the coronal portion of the canal and add heat to the cone. C, Initial compaction. D, Segments are removed with a heated instrument, followed by compaction. E, Once the apical extent of compaction is reached (F), heated segments are placed in the canal and compacted (G).

FIGURE 12-13 A to D, Examples of well-shaped and well-obturated canals that were achieved by using NiTi rotary instruments to ensure proper enlarging and shaping. Note the tapers and shapes of the canals. Excessive removal of root dentin was not necessary to achieve these goals.
With ALL techniques of canal preparation and choice of vertical compaction for obturation:
Thermoplasticized Injection Techniques
Gutta-percha may be softened and delivered to the prepared canal using a variety of instruments designed for injection that permits compaction (Calamus Flow, Calamus Dual 3D obturation system [Dentsply Tulsa Dental Specialties, Tulsa, OK, USA]; BeeFill 2in1 [VDW, Munich, Germany]; Elements Obturation Unit [SybronEndo, Orange, CA, USA]; E&Q Master [Meta Dental Co., Elmhurst, NY, USA]).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses




