Chapter 12
Periodontal regeneration
Introduction
“Lesson one” for any student of periodontology usually describes periodontitis as occurring when gingivitis spreads to the deeper periodontal tissues, causing irreversible loss of marginal alveolar bone and periodontal ligament and also apical migration of the junctional epithelium. Thus, periodontitis is considered to cause irreversible tissue loss, and it is not surprising that for many years one of the major challenges in periodontal research has been to devise and implement methods to regenerate the tissues that are lost due to the disease process.
A number of different techniques are now in use for promoting periodontal regeneration (also sometimes referred to as “new attachment therapies”). In this chapter, these techniques are outlined, their clinical indications are described, the outcomes that can be achieved by these methods and the factors that may influence outcomes are discussed, and a brief review of possible future developments is considered. It should be stated at the outset that success with periodontal regenerative therapies is dependent on the skill and the experience of the operator, and consequently these procedures are normally considered as within the realm of the trained periodontal specialist. The general dentist, however, should be aware of the methods used and their possible applications, but it is not the intention of the discussion here to give a comprehensive description of the detailed techniques used during regenerative procedures.
Overview of regenerative therapies
Periodontal regeneration can be defined as the regeneration of periodontal tissues to replace those lost due to disease, resulting in the formation of new bone, cementum, and functionally orientated periodontal ligament. Because these criteria can only be confirmed definitively by histological examination, in clinical use their outcome is assessed by increased gain in clinical attachment level and increased bone height, either by radiographic evaluation or sometimes, particularly in studies, by direct “bone sounding” using a probe under local anaesthesia. All of the techniques have (to a greater or lesser extent) been evaluated for histological evidence of actual regeneration, mainly in animal models of periodontal regeneration.
There are three main types of regenerative therapy:
• Barrier membranes (guided tissue regeneration)
• Biologically active materials that stimulate the periodontal tissues to regenerate
Guided tissue regeneration
Guided tissue regeneration (GTR) is the use of barrier membranes to exclude the superficial gingival tissues from a healing periodontal surgical wound and thus promote wound repopulation by cells of the periodontal ligament which are able to regenerate the periodontium. The basic technique involves the placement of a thin membrane overlying the periodontal defect under the gingival flap during periodontal surgery. The membrane is secured in place, usually with an internal suture, and the flap is repositioned and sutured over the membrane (< ?xml:namespace prefix = "mbp" />
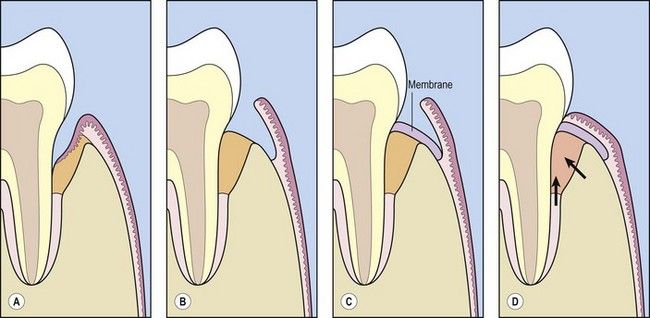
Fig 12.1 Diagram of the principles of guided tissue regeneration. (A) Pocket formation and infrabony defect. (B) Flap raised surgically, and granulation tissue from infrabony defect removed. (C) Membrane placed over defect. (D) Flap replaced and sutured. Membrane forms a barrier to exclude gingival tissues from surgically debrided defect and promotes wound repopulation by cells migrating from the periodontal ligament and bone (arrows).
Graft materials
A wide range of graft materials have been described for placement in periodontal defects to promote periodontal regeneration. The types of graft are summarized in
Table 12.1 Types of graft material for periodontal regeneration
| Type | Description | Additional comments |
|---|---|---|
| Autografts | Autogenous bone harvested from a donor site from the same patient and placed in the periodontal defect | Bone harvesting from donor site (e.g., mental region of mandible, tuberosity of maxilla, iliac crest) is associated with considerable increased patient morbidity |
| Allografts | Graf/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses



