Functional occlusion goals in orthodontics
More than 100 years have elapsed since modern orthodontics gathered momentum under the leadership of Edward H Angle.1 Has his theory that good function and facial aesthetics would automatically follow if the patient bites into Class I ever been validated?2 Angle’s concept is still widely accepted as truth without ever having been questioned. Is it true that function improves automatically if the teeth are aligned within the dental arches with the molars in Angle Class I?3 Is there a body of evidence in the literature demonstrating that orthodontic treatment based on the Angle philosophy will always result in functional improvement?4,5 The teeth will certainly be straighter and aesthetically more pleasing with treatment, but we must pay closer attention to functional aspects of occlusion and question ourselves if function has really been enhanced and maintained as a result of treatment. While there have been remarkable advancements in orthodontic appliances and materials since the days of Edward H. Angle, basic principles of orthodontic diagnosis and treatment have remained relatively unchanged. Should mere straightening of all teeth in the mouth automatically lead to the establishment and maintenance of good function? Why are so many patients seeking retreatment? Something seems to be missing here. In the author’s view, it is the awareness of treatment goals in terms of functional occlusion that is lacking in the orthodontist’s mind.6 We have no clearly defined goals with clear-cut criteria as to what needs to be done for each patient we treat. If orthodontic procedures are meant to be therapeutic rather than simply cosmetic, the posttreatment health of the patient’s stomatognathic system should be improved with lasting effect.7,8 Can we really expect long-term stability of the postorthodontic result with traditional methods of diagnosis and treatment? Unfortunately, the answer to this question is negative. Treatment focusing only on the alignment of teeth and improvement of form often fails to attain functional improvement, let alone consistently achieve long-term stability, though one may get lucky every once in a great while. Orthodontists throughout the world are still making diagnoses and treating patients in a manner similar to our predecessors in Angle’s days whose orthodontic goal was simply to align teeth. The time has come for us as professionals to seriously reflect upon orthodontic goals for good functional occlusion. If we fail to do so, orthodontics would be left behind without further progress except for the development of new appliances and materials. This chapter describes the concept that will help us improve the function and form of the dentition through goal-directed treatment.
Goals of Orthodontics for Occlusion
The orthodontic treatment goal in terms of function is to create the occlusion that allows the upper and lower teeth to come into maximum intercuspation, while condyles are positioned such that there is minimal strain on the muscles of mastication. At the same time, the position of the teeth should be in harmony with the face, lips, tongue and periodontium (Fig 12.1).
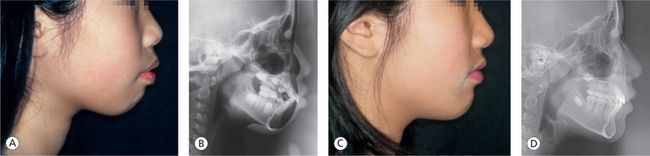
Figure 12.1 (A and B) Before orthodontic treatment. (C and D) After orthodontic treatment. Posttreatment facial profile is in harmony with tooth alignment, and perioral muscles are naturally relaxed. Condylar position was stabilized before initiating tooth movement. Careful tooth movement and counterclockwise mandibular growth allowed the chin to come forward without an increase in lower facial height, providing good function and facial harmony, which resulted in relaxed muscles and stable tooth position.
In a normally developing temporomandibular joint (TMJ), the basic structures comprising the joint – namely the disc, condyle and eminence – are intimately related to one another. By age of about 10 years, the eminence will have sufficient height to disclude the posterior teeth in mandibular movements.9 The child has a mixed dentition at this age, and it will take a few more years before the permanent dentition is complete from second molar to second molar. In the meantime, the first permanent molars and deciduous molars provide posterior support. Anterior guidance10 has not yet been established. Lateral movement is guided mostly by the permanent incisors or deciduous canines or by the deciduous molars and first permanent molars in some situations.
As a starting point for orthodontic tooth movement, we should first aim at achieving proper positioning of the condyles in the fossae where there is minimum masticatory muscle activity, followed by the provision of posterior support and proper alignment of the anterior teeth that guide protrusive and lateral movements. When this relationship between the occlusion and the joints is established, the efficiency of the masticatory muscles can be maximized without an increase in muscle tension.11 The clinical significance of orthodontics thus lies in the establishment of a harmonious relationship between the joints and the occlusion that does not require excessive muscle tension. Once the harmony has been achieved, orthodontic treatment results will remain stable (Fig 12.2).
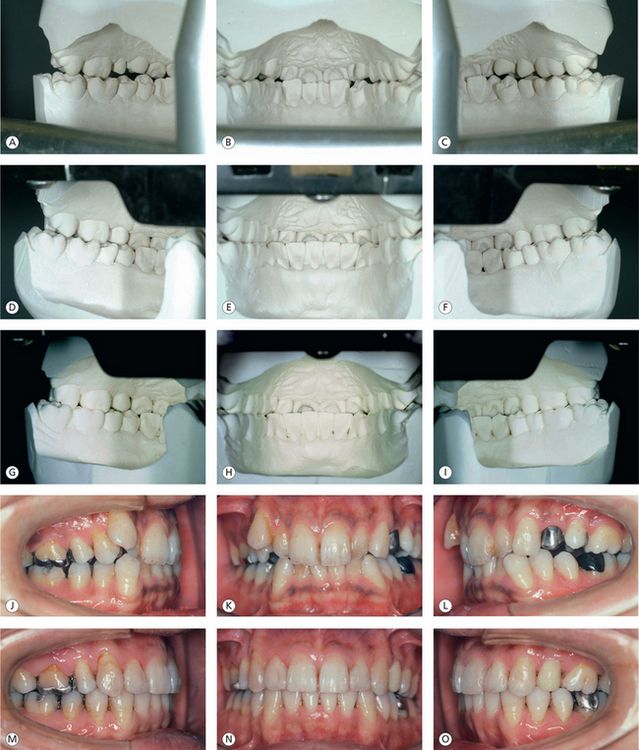
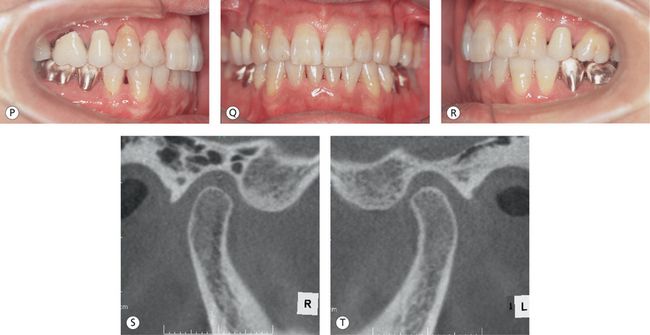
Figure 12.2 15 years out of treatment. Establishment of functional occlusion through maximum intercuspation of posterior teeth, adequate anterior coupling and canine guidance seems to have contributed greatly to the posttreatment stability. (A–C) Lingual views of initial mounted models. (D–F) Lingual views of posttreatment mounted models. (G–I) Occlusion remains stable, 15 years out of treatment. (J–L) Pretreatment labial and buccal views. (M–O) Posttreatment labial and buccal views. (P–R) Labial and buccal views, 15 years after treatment. (S and T) The cone-beam computed tomography (CBCT) images of the right and left joints, 15 years after treatment, show well-rounded functional articular surfaces, normal position of the condyles relative to the fossae and eminentia and well-preserved bone structures.
No dentist seems to argue against the importance of optimum condylar position as the basis of functional occlusion,12–14 yet this fundamental principle of dentistry is not clearly defined and often disregarded in our current clinical practise. Use of traditional orthodontic records for diagnosis does not allow us to determine if the patient’s existing mandibular position is appropriate or not. These records contain no objective data to show discrepancies in the joints. Hand-held models, for example, provide no information on mandibular position and provide no indication about where condyles are positioned in the fossae. The same is true for lateral cephalograms, which is a two-dimensional representation of three-dimensional anatomical structures such as the joints derived from mere addition of the left and right and divided by two. Then, how can we capture data on mandibular position? Knowing the answer to this question would help to enhance the quality of our clinical practise.
Mandibular Position as a Functional Goal of Orthodontic Treatment
A stable and repeatable mandibular position is important as a functional goal of orthodontic treatment. Without this functional goal, teeth may appear nice and straight in the mouth, but the tooth alignment thus obtained would not last long and may even do harm to the gnathic system. The following five requirements must be fulfilled to achieve this stable and repeatable mandibular position:

Figure 12.3 The disc is in normal position with the posterior band at 12 O’clock and the intermediate zone interposed intimately between the eminence and condyle.
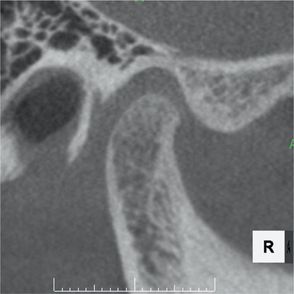
Figure 12.4 The articular eminence has a smooth S-shaped curve. The condyle also has a rounded surface and is in normal position within the fossa.
A stable and repeatable mandibular position requires the disc to be optimally placed on the condyle in close contact with the eminence without capsular or ligamentous laxity or excess synovial fluid. When these requirements are met, the condyles are seated against the discs at the most superior-anterior position against the eminentia, leading to a stable position of the condyles in the fossae.
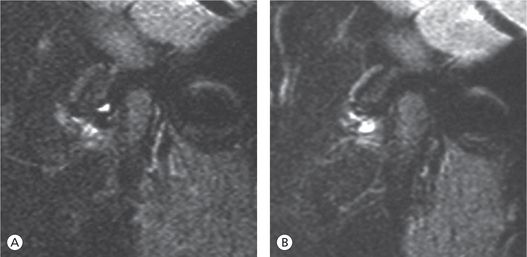
Condylar position then becomes repeatable with the condyles always returning to the same position. This is illustrated with the MRI images of the movement of the condyle–disc assembly in Figure 12.6. At the start of opening, the condyle is situated against the intermediate zone of the disc at the most superior position in the fossa in close contact with the eminence. Upon opening, the condyle begins to rotate and translate as it goes down the slope of the eminence without losing the close contact with the eminence via the intermediate zone of the disc. In closing, the condyle follows the identical reciprocal path to return to the starting position. The movement is thus repeatable.
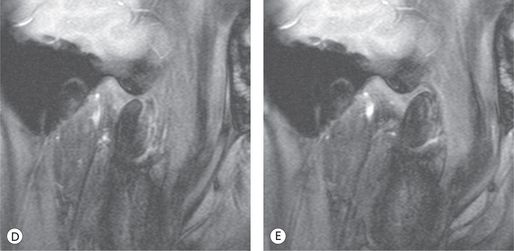
Figure 12.6 (A–E) Every cut from this MRI movie of condylar movement from centric occlusion (CO; habitual occlusal position) to maximum opening demonstrates the stable spatial relationship between the condyle and the eminence throughout the movement.
When the teeth close into maximum intercuspation with the condyle and disc seated at the most superior position in the fossa, that is, when there is harmony between the occlusion and the joints – the associated muscles are so relaxed that bite registration becomes very easy. However, this is rarely the case when we examine our orthodontic patients, both adults and children, at their initial visits. It is important to realize that a majority of our patients have varying degrees of disc displacement. These patients naturally have strained masticatory and perioral muscles, necessitating very careful registration of mandibular position at the time of initial examination.
Joints First
If we are to establish the harmony between occlusion and joints, which should we look at first when examining our patients, the occlusion or the joints? The answer is ‘the joints first’. The status of the joints should be closely examined before intraoral examination of occlusal relationship. Traditionally, orthodontists have attached importance to the way the upper and lower teeth fit together in the mouth and assumed that the joints would adapt to the occlusion. Are the joints always so pliable? With the advent of advanced imaging modalities such as CBCT and MRI, we are now able to visualize the joint structures more precisely. Accumulating data suggest that the joints may not be so adaptable. Three postorthodontic cases are shown to illustrate this point.
The first case is a male patient treated at the author’s office and is out of treatment for 7 years (Fig 12.7). He was 13 years old at his initial visit. His masticatory muscles were very tight, making bite registration difficult. He was also experiencing frequent headaches. He was therefore placed on a stabilization splint (hereinafter referred to Splint) in order to stabilize his mandibular position, prior to orthodontic treatment. The direction and amount of tooth movements were determined based on the results of the rediagnosis made in the stabilized mandibular position. The second case is a patient treated elsewhere, 2 years prior to coming to the author’s office with parents for consultation because of unstable orthodontic results (Fig 12.8). The previous orthodontic treatment did some good in that the teeth were well aligned. However, the imaging of the joints revealed hidden discrepancies.
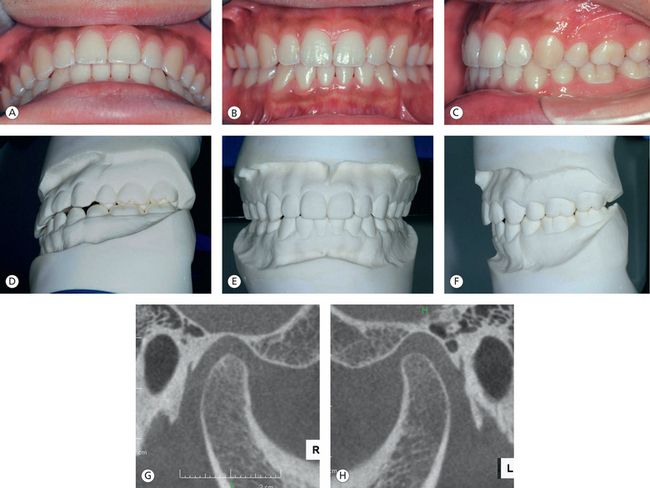
Figure 12.7 (A–H) Both joints and occlusion remain stable, 7 years after completion of orthodontic treatment. The trabecular bone of the articular structures exhibits a functional pattern outlined with uninterrupted cortication.

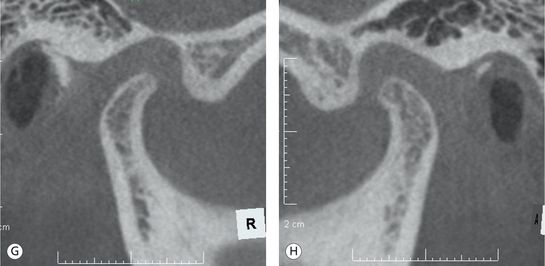
Figure 12.8 (A–H) Although teeth are still aligned, 2 years after the first orthodontic treatment, unstable bite and poor joint health are evident compared to the case presented in Figure 12.7.
Case 2 had a problem with the position of the condyles in the fossae. The condyles were significantly displaced inferiorly with the loss of intimate relationship between the condyle, disc and eminence. The shape of the condyles had also been greatly altered along with a decrease in size, precluding normal condylar movement. In Case 1, the condyle–disc–eminence relationship has been maintained with optimum condylar morphology and position in the fossae, allowing for normal function.
At the tooth level, Case 1 has adequate coupling of the anterior teeth and good canine guidance for lateral movement. The buccal cusps of the mandibular posterior teeth are either on the marginal ridges or in the central fossae of the upper posterior teeth. In contrast, Case 2 lacks in both anterior guidance for protrusive movement and canine guidance for lateral movement due to inadequate overbite. Case 2 also lacks stable posterior support.
What was the orthodontist’s treatment goal for Case 2? Without harmony between the occlusion and the joints, we cannot expect long-term stability of the postorthodontic treatment result. The patient will most likely be subjected to muscle strain, tooth mobility and occlusal wear.
Case 3 is also a postorthodontic patient, 3 years out of treatment (Figs 12.9–12.12). The patient, being a dentist herself, was aware of functional problems with a complaint of muscle fatigue from chewing. Her bite changed within a single day with full-time splint wear. How can we explain the changes? Solely based on what we see in the mouth, we cannot explain this phenomenon. Even if we could relate the intraoral changes to changes in condylar position, there is no way of knowing in which direction and to what extent the condyles moved in the three planes of space. This case, like Case 2, had well aligned teeth and could bring the teeth into intercuspation. Both cases would be considered well-treated cases in traditional orthodontics. In reality, however, they had major discrepancies hidden in the joints, were suffering from masticatory fatigue and had adverse effects on the muscles, teeth and periodontium. Their gnathic systems were not functioning in an ideal manner. Figure 12.10 shows a periapical radiograph of the second molar on the lower left side with widened periodontal ligament (PDL) space, indicating occlusal trauma. The tooth also had pathological mobility and gingival recession. The intraoral photograph taken after full-time splint wear reveals a premature contact between the upper and lower second molars on the left side. However, prematurity could not be found in the mouth at her initial visit. Figure 12.11 shows the patient’s initial models mounted in centric relation (CR). Her initial CR bite was taken with wax and the models were mounted on an articulator using the CR bite. It was possible to capture the premature contact at the left second molars on the initial CR-mounted models, while the prematurity was completely hidden in the patient’s mouth. This phenomenon is caused by the neuromuscular protective mechanism. The hidden contact cannot be found during initial examination unless the models are mounted using a CR bite carefully taken while avoiding any tooth contact between the upper and lower teeth.

Figure 12.9 (A–F) The bite changed after 24 h of splint wear. Since it is inconceivable that the teeth moved with only 1 day of splint use, the bite change can be attributed to changes at the joint level.
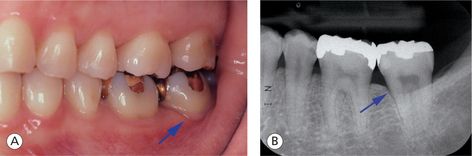
Figure 12.10 (A and B) Periapical radiograph of the patient’s lower left second molar. The PDL space is widened (arrow), i ndicating increased tooth mobility. Localized gingival recession (arrow) around the same tooth and tooth wear on canine cusp are also evident intraorally.
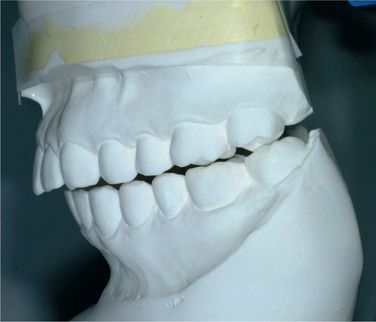
Figure 12.11 The left lateral view of CR-mounted models taken at initial visit reveals a premature contact on the lower left second molar. When performed properly, CR mounting may uncover what cannot be seen intraorally.
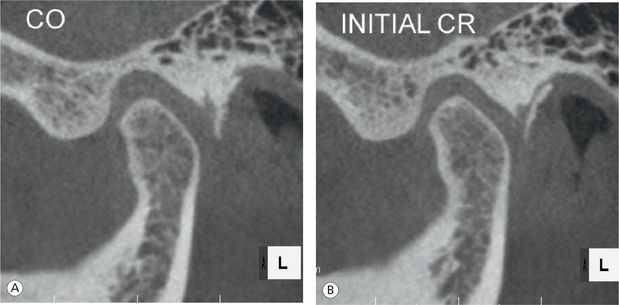
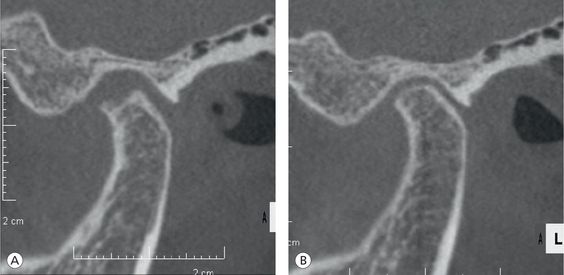
Figure 12.12 (A and B) The condyle is positioned noticeably more forward and upward in CR bite (B) relative to CO bite (A), indicating that CR bite allows anterosuperior seating of the condyle.
The recent advent of CBCT allows direct visualization of the CO-CR discrepancies in the joints for this case (Fig 12.12). These images were taken upon patient consent with her initial CR bite in place, showing that the use of a carefully taken initial CR bite enables us to visualize and even quantify superior-anterior seating of the condyles in the fossae. We can also see CO-CR discrepancies in the joints by comparing CBCT images taken in the two different positions. CBCT images thus demonstrate through the visualization of the joint structures that the use of a properly taken CR bite allows the condyles to seat superiorly and anteriorly in the fossae.
More than 99% of orthodontists seem to make diagnoses and assess postorthodontic results solely based on what they see in the mouth as in Cases 2 and 3. We should not believe what we see in the mouth before confirming the condylar position. The author uses the records shown in Figures 12.11 and 12.12 to make a diagnosis, since his orthodontic goal is to attain harmony of the occlusion with the dictates of the joints, which is different from the traditional orthodontic goal of aligning teeth. To pursue this goal, it is essential to first examine the joints, hence ‘the joints first’.
Anatomy of the Temporomandibular Joints
Structure of the disc
The disc, which mainly consists of dense collagen fibres without any innervation or vascularization, is divided into the anterior band, intermediate zone and posterior band. The intermediate zone, in particular, is a good shock absorber with collagen fibres oriented predominantly in anteroposterior (PA) direction. The disc of a newborn is biplanar in shape with all three sections equal in thickness but soon becomes biconcave, in approximately 2 months, as the joint start to function. According to Hansson,15 the normal functioning disc’s posterior band, intermediate zone and anterior band are 3, 1 and 2 mm in thickness, respectively.
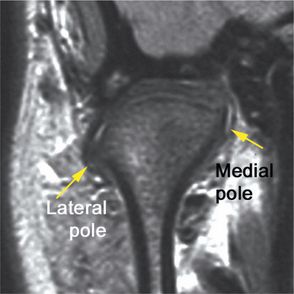
Normal position of the disc
The posterior band of the disc is at the 12 O’clock position relative to condylar head (Fig 12.13). The intermediate zone is in intimate contact with the articulating surface of the condyle and the posterior slope of the articular eminence. The anterior band is slightly inferior and anterior to the rotational centre of the condyle and slightly superior to the apex of the eminence.
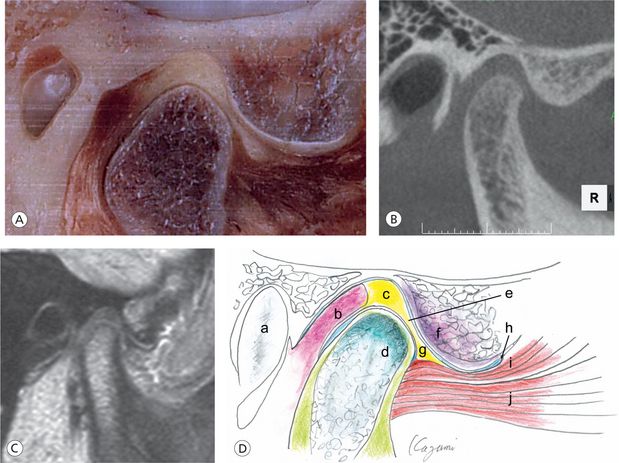
Figure 12.13 (A) The cryosection (Image courtesy: Dr A. Isberg, Sweden), (B and C) CBCT and MRI image of a same patient. (D) Illustration depicts normal joints: a, auditory canal; b, posterior disc attachment; c, posterior band; d, condylar head of mandible; e, intermediate zone; f, articular eminence; g, anterior band; h, anterior limit of capsular insertion; i, superior head of lateral pterygoid muscle; and j, inferior head of lateral ptery-goid muscle.
Roles of the disc
The disc has two main roles. The first role of the disc is to stabilize the condyle in the fossa with the assistance of associated ligaments and muscles. The posterior band of the disc, being at the 12 O’clock position in a normal joint, serves as a good indicator for the most superior position of the condyle during mouth closure. This disc–condyle relationship makes the terminal hinge axis (THA) stable and repeatable. The second role of the disc is to distribute the load applied to the articulating surfaces of the condyle and eminence during mandibular function by interposing between the two structures. The presence of just enough synovial fluid outlining the joint surfaces also serves as a lubricant to allow smooth movement of the condyle. The disc contributes to the maintenance of anatomical configuration of the condyle and eminence by preventing excessive loading to these structures. The position and function of the disc thus have major impact on mandibular structural development in growing children by providing the optimum force on the cartilage at the growing aspect of the bone.
Reversibility
Positive remodelling of the condyle and eminence is routinely observed on CBCT images as mandibular position becomes stabilized even in cases of disc displacement without reduction. These positive morphological changes may be accompanied with improvements in disc position in some patients with early to moderate disc displacement. The amount of synovial fluid is normalized at the same time (Fig 12.14).
Condyle
The condyle is covered with dense connective tissue similar to periosteum. Underneath this covering is an undifferentiated mesenchymal cell layer. Under this layer, there is a cartilaginous layer with chondrocytes.16 The cartilage here is called secondary cartilage, which is different in nature from the cartilage in the growth centre of a long bone in that its proliferation depends on the surrounding environment rather than the growth hormones.17 Its proliferative capacity is retained through adulthood, allowing the condyle to adapt to environmental changes. The bone is formed through ossification of this cartilage. The undifferentiated mesenchymal cell layer remains until an advanced age, although its thickness decreases after the end of growth.18 It contributes to chondrocyte proliferation if such a need arises (Fig 12.15).
Factors causing condylar deformity
Reversibility
The intact fibrous covering of the condyle permits positive remodelling of the condyle even in adults. The shape of the condyle can be improved when aetiological factors of condylar deformity are removed20 (Fig 12.16).
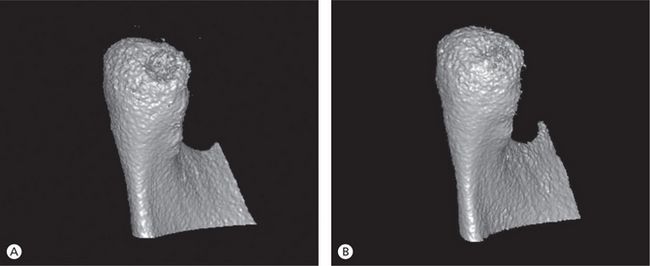
Figure 12.16 (A and B) Comparison of the condyle of a 31-year-old woman before and after orthodontic treatment demonstrates positive remodelling or restoration of the major bone defect that was present initially on the posterior surface. Orthodontic mechanics was designed to minimize stress to the joints, so that posttreatment CO-CR discrepancy could be kept to a minimum.
Eminence
The eminence basically has the same structure as the condyle. When the condyle undergoes negative remodelling or resorption in response to a factor causing joint instability, the eminence is also subjected to more or less similar changes. Conversely, when mandibular position is stabilized, positive remodelling is observed in the eminence and in the condyle.
Normal configuration of the eminence
The articular eminence is a convex area of the articulated surface of the temporal bone with a gentle and smooth S-shaped curve and a thin cortical outline. The more superior the condyle is positioned in the fossa, the steeper the slope of the eminence becomes. This facilitates the disclusion of the posterior teeth in mandibular movements.
The anterior limit of the joint is determined by the insertion of th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses