Diagnosis and Management of Dental Caries
Annika Julihn, Margaret Grindefjord, and Ivar Espelid
The concept of caries diagnosis
The proper management of dental caries in clinical practice requires an accurate diagnosis. Before deciding on a treatment plan, which may include a range of clinical techniques, the characteristics of the manifestations of the caries disease of the individual child must be assessed. This includes the child as a whole, as well as individual teeth and surfaces. In this chapter the concept of caries diagnosis and its diagnostic tools are described. The chapter also describes the concepts of nonoperative and operative treatment and the properties of restorative materials and techniques for their use. Age‐specific considerations related to caries diagnosis and treatments are described under separate headings.
Dental caries is the localized destruction of susceptible dental hard tissues by acidic byproducts from bacterial fermentation of dietary carbohydrates [1,2]. The disease process is initiated within the bacterial biofilm (dental plaque) that covers the tooth surface. The process is dynamic and numerous episodes of loss and gain of mineral (demineralization and remineralization) take place on the enamel surface. If demineralization prevails over remineralization the result will be permanent and irreversible loss of mineral, cavity formation, and continuous destruction of hard tissues [3]. The signs and symptoms of the disease range from the smallest subsurface loss of minerals to severe destruction of the tooth (Figure 12.1). In clinical practice, the signs and symptoms of the carious demineralization describe the disease once it is detectable by visual–tactile examination possibly combined with other diagnostic methods such as radiography. In this chapter the term caries is used to describe both the caries disease and the caries symptoms (lesion). See Box 12.1.
Figure 12.1 How is caries defined? Caries disease is assessed by its signs and symptoms that depend on the severity of the disease. The figure shows the time‐dependent development of a lesion from a subclinical level to increasing destruction of dental hard tissues.
Detection and assessment of the caries lesion (caries diagnosis)
Assessment of the presence or absence of a caries lesion is dependent on the cut‐off chosen. Traditionally, the presence of a cavity involving the dentin defines a carious (decayed) tooth that needs a filling. Along with changes in caries prevalence, incidence, distribution, severity, and rate of lesion progression, the treatment philosophy has also changed. Thus, there is a growing international trend in clinical practice to move, wherever possible, away from operative intervention towards the nonoperative treatment of caries [4]. This has necessitated the need for a more detailed description and assessment of the caries lesion and also methods for monitoring the behavior of a lesion (regression, progression, or no change) [5].
Assessing and grading lesion severity
A valid and reliable system for assessing and grading the severity of the caries lesion has many advantages:
- Progression of the disease can be more accurately monitored and the effect of measures to control the disease may be evaluated.
- Clinicians can calibrate themselves and inter‐observer and intra‐observer reliability can be assessed.
- It can facilitate the communication between the clinician, the patient, and the parent.
- It can facilitate the communication between clinicians, researchers, and public dental health workers.
The ICDAS (International Caries Detection and Assessment System) has been introduced for this purpose and great efforts have been made and still continue to make the criteria valid and reliable [6]. The ICDAS detection codes range from 1 to 6 depending on the severity of the caries lesion. The basis is essentially the same for all types of surface, but varies somewhat depending on surface characteristics (pit and fissures versus free smooth surfaces) and whether or not there are adjacent teeth present (mesial and distal surfaces). The codes and criteria are given in Box 12.2.
Detection and grading the severity of approximal lesions of surfaces contacting neighboring teeth are done from bitewing examination. How radiographic findings should be integrated with the clinical ICDAS criteria is still to be decided. ICDAS‐based codes for free smooth surfaces and occlusal surfaces are presented in Figure 12.2(a). An alternative to the ICDAS criteria, which also includes radiographic scores for approximal surfaces, is given in Figure 12.2(b).
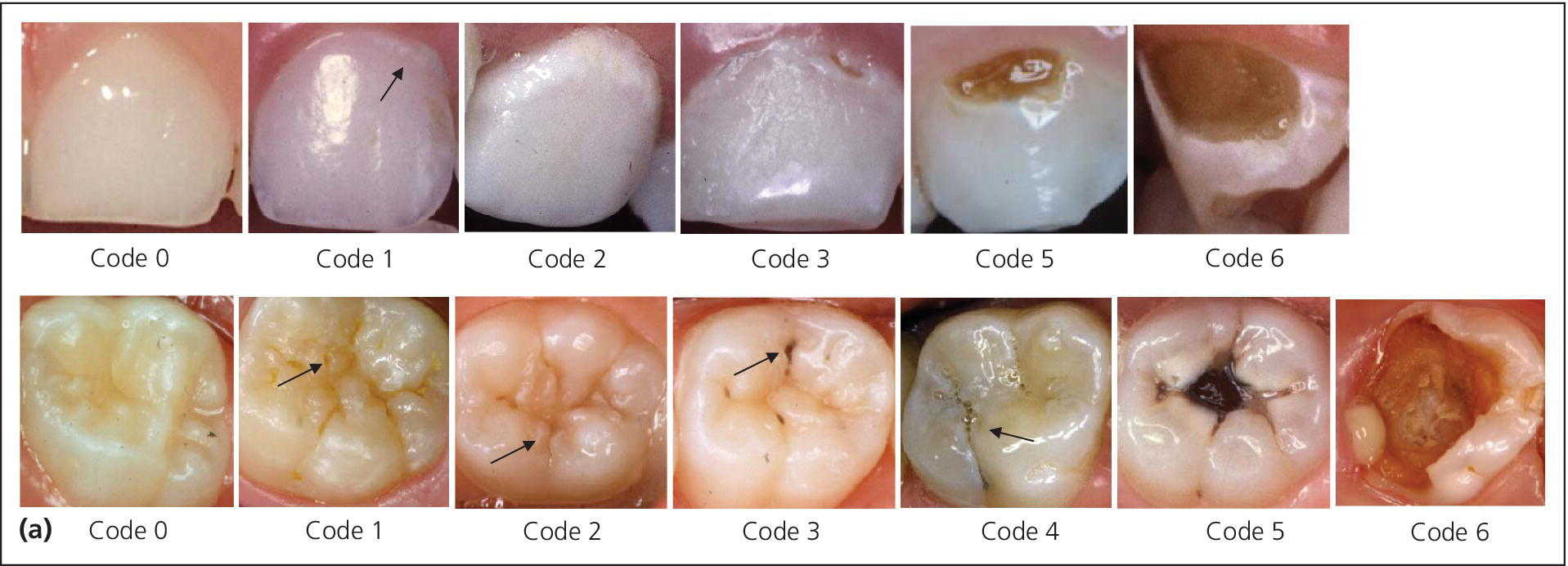
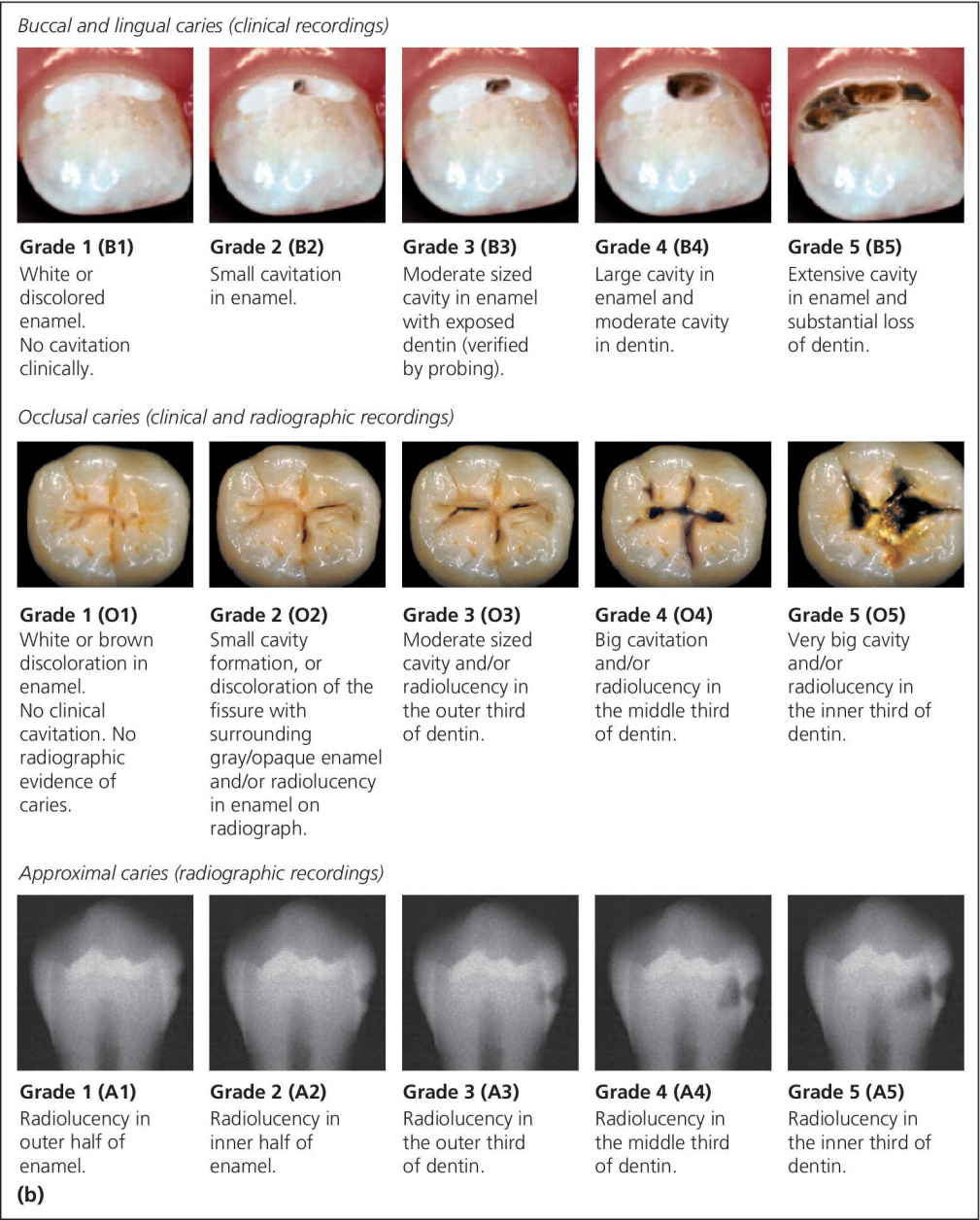
Figure 12.2 (a) ICDAS‐based criteria for severity grading of caries on free smooth and occlusal tooth surfaces. (b) Alternative index using a five‐graded scale for severity grading of caries on free smooth, occlusal, and approximal tooth surfaces.
Assessing and grading lesion activity
Assessment of lesion activity is as important as lesion detection. Criteria for active and inactive caries lesions slightly modified after Nyvad et al. [7] and Ekstrand et al. [8] are presented in Box 12.3. Figure 12.3 illustrates active and arrested lesions.
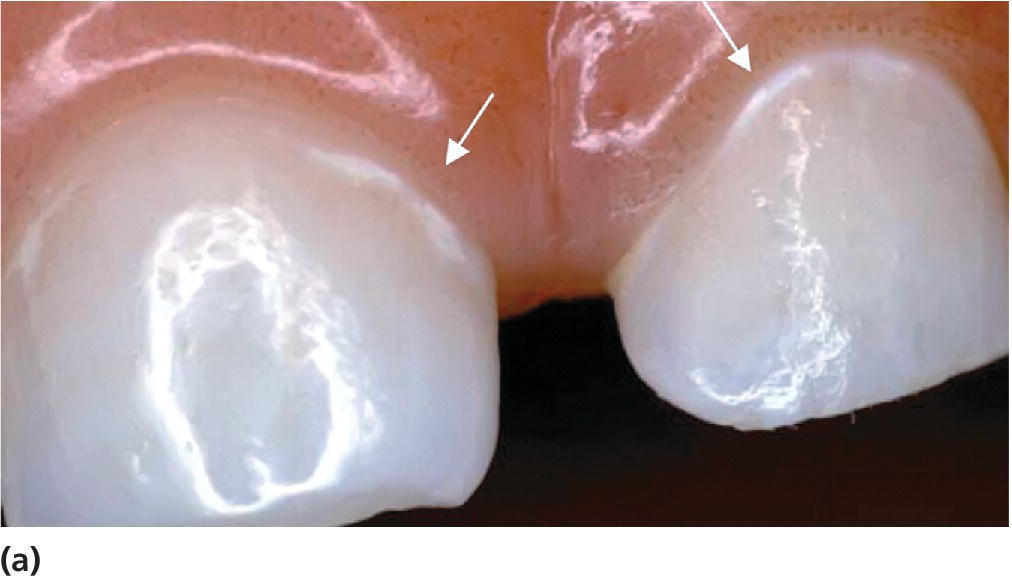
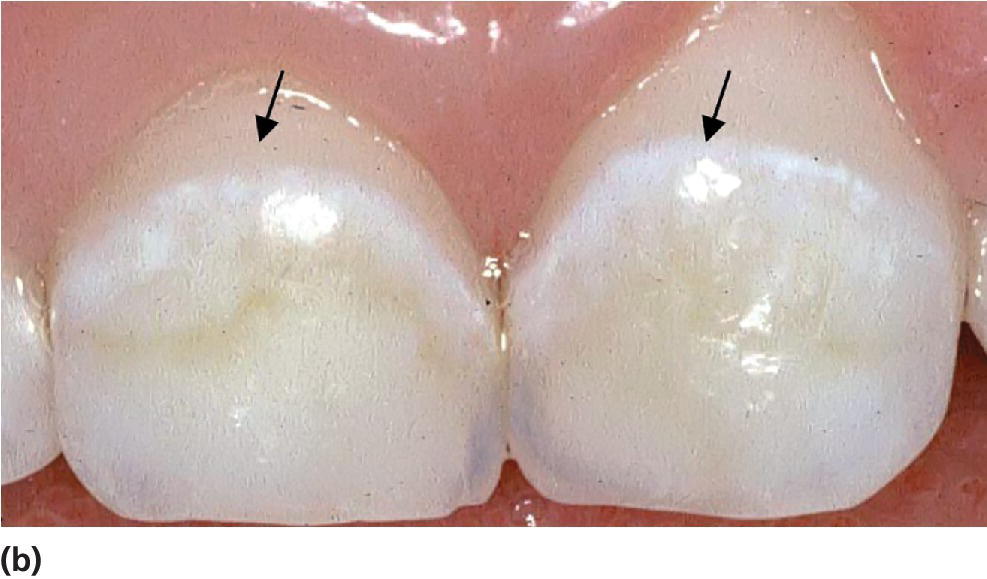


Figure 12.3 Active and inactive/arrested caries lesions. Upper row shows initial (noncavitated lesions) and the lower row shows cavitated lesions. (a) Active noncavitated lesions close to the gingival line on the buccal surfaces of primary upper incisors in a 2‐year‐old. There is loss of luster and the lesions are rough on probing. (b) Arrested noncavitated lesions on the buccal surfaces of primary upper incisors in a 4‐year‐old. The lesions are situated at a distance from the gingival line, and are shiny and hard on probing. (c) Active cavitated lesion in a primary lower second molar in a 5‐year‐old. The dentin is soft on probing and the cavity borders are blunt and irregular. (d) Inactive/arrested cavitated lesion in a primary lower first molar in a 7‐year‐old. The dentin is brownish‐black, hard on probing, and the cavity borders are sharp and regular.
Diagnostic tools
Visual–tactile and radiographic examination
The two traditional, and still most commonly used, diagnostic tools are visual–tactile examination and bitewing radiography. How accurate are these methods? That is, how well do they correspond to the true presence and extension of a lesion? A systematic review [9] concluded that visual–tactile examination is a simple, cheap, and reliable method for diagnosing obvious lesions on all tooth surfaces not contacting neighboring tooth surfaces. Also, visual–tactile examination is reliable for detecting early enamel lesions on buccal and lingual surfaces. It is, however, less accurate for detecting enamel and early dentin lesions on occlusal surfaces. For this purpose visual examination of occlusal surfaces should be combined with bitewing radiography. The same applies to enamel and dentin lesions on approximal surfaces in contact with adjacent teeth.
The teeth should be cleaned, dried, and examined in good lighting. A whitish carious spot is detected more easily when the tooth is dry, since the difference in refractive index between carious and sound enamel is higher when the water in the porous carious enamel is removed by drying.
Occlusal surfaces (pit and fissures)
Particularly in pits and fissures, the probe should be used carefully in order to avoid iatrogenic damage (Figure 12.4). The probe is an important tactile aid and may be necessary to remove plaque. However, solely visual assessment of early (noncavitated) fissure caries lesions is not improved by probing [10]. In this context it is important to recognize that even if the probe “catches,” this does not necessarily mean that there is a soft lesion.
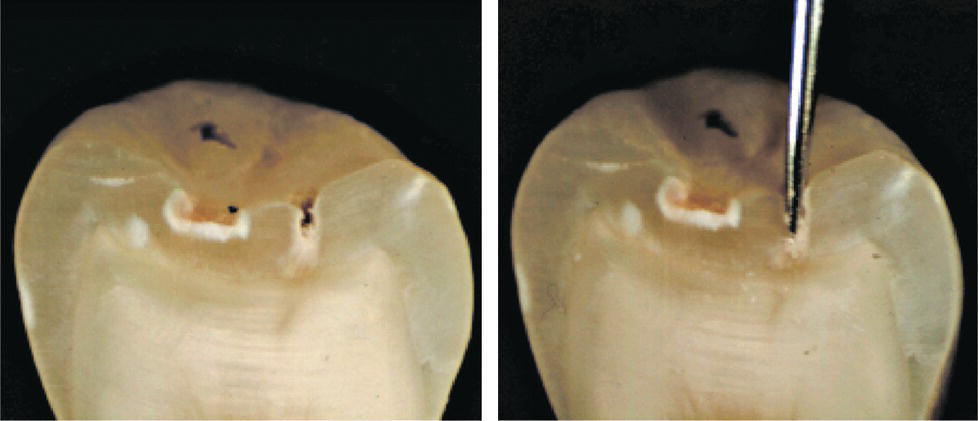
Figure 12.4 Sectioned premolar with an enamel caries lesion in the fissure before probing (left). Intense probing (right) destroys the surface zone of the lesion.
Early caries lesions may develop during tooth eruption when the occlusal surface of the molar constitutes a plaque stagnation area [11]. The reason is that the occlusal surface is located below the occlusal plane and is easily missed by the toothbrush. These early lesions are characterized by whitish opaque areas at the entrance of the fissures, and are easy to overlook if the surface is not clean and dry and the lighting is not optimal. For the same reasons, small cavitated lesions in these areas may easily be missed.
The discolored fissure often poses diagnostic challenges. A discolored fissure does not necessarily indicate an active caries process. To discriminate between active and inactive or arrested lesions, the following characteristics may help:
- Active lesions are most frequently seen in erupting and newly erupted teeth in children with other signs of caries activity in the dentition. The discoloration is usually opaque, whitish, or light brownish. Softened enamel at the entrance of the fissure from gentle tactile probing is indicative of an active lesion. When the discoloration also involves obvious loss of continuity of the enamel surface (clinical cavity), bitewing examination frequently reveals a radiolucency in the dentin (Figure 12.5). Many borderline cases can be difficult to diagnose. For these cases, bitewing radiography is a valuable tool for assessing possible dentin involvement (Figure 12.6a,b).
- Inactive lesions are usually seen in “older” teeth in adolescents with no signs of caries activity. The discoloration is dark brown or black and the surface is hard on careful probing (Figure 12.6c). There is usually no substantial dentin involvement.
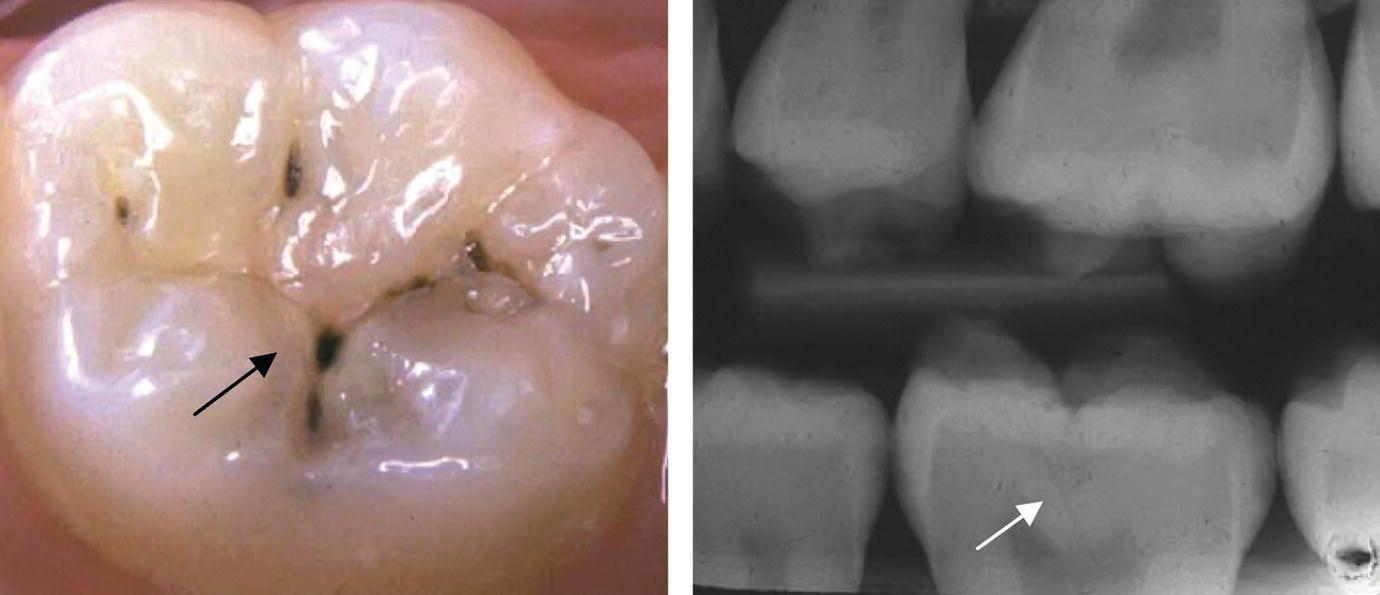
Figure 12.5 A small but obvious occlusal cavity in the central fossa of a permanent first molar (arrow). The borders around the cavity are whitish and rough in texture suggesting an active caries process. There is a shadow from underlying dentin caries. The radiograph reveals a substantial radiolucency in the dentin (arrow).
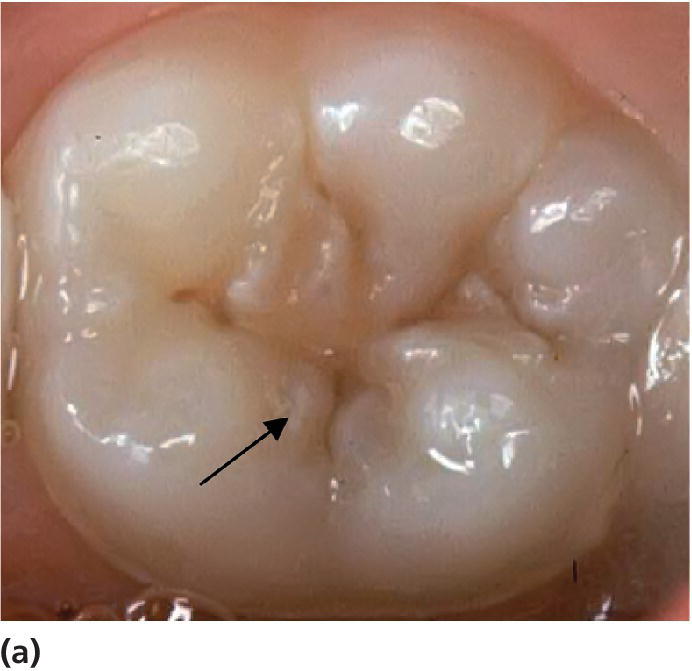
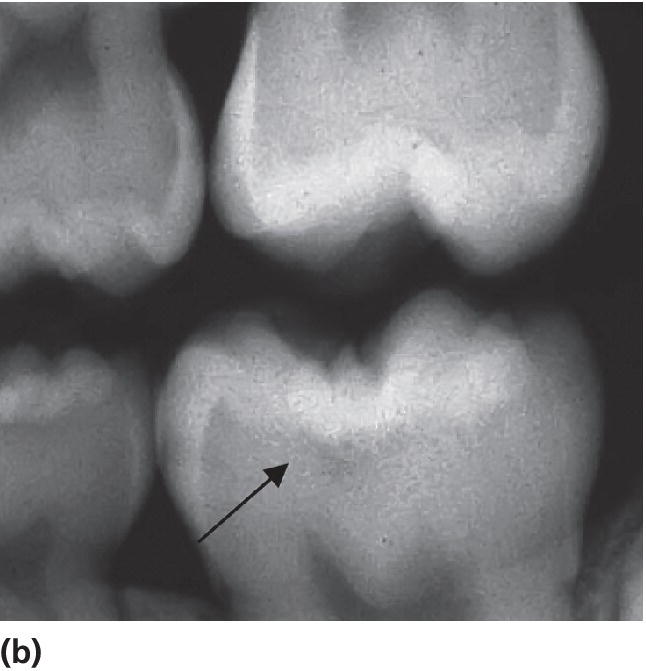
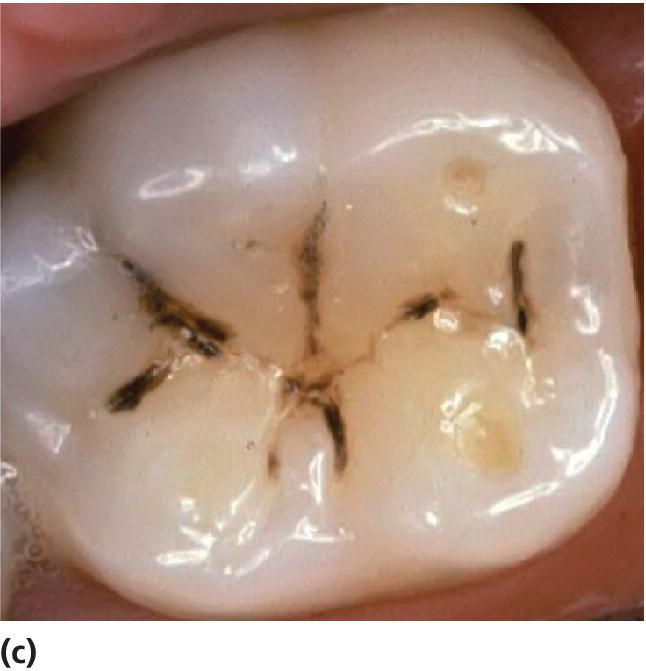
Figure 12.6 (a) Light brown discolored fissures in a permanent first molar of an 8‐year‐old. The enamel around the central fossa is whitish and there is softened enamel at the entrance of the fissure indicating an active lesion (arrow). (b) The radiograph reveals radiolucency in the dentin (arrow). (c) Dark brown/black discolored fissures in a permanent first molar of a 19‐year‐old with a low caries activity. The fissures are hard on probing indicating an arrested (inactive) lesion.
Free smooth surfaces
The buccal and lingual aspects of teeth are easily examined, and it is easier to disclose small changes in surface color and texture of early caries lesions on these surfaces compared to “inaccessible” areas on approximal surfaces or in pits and fissures. The active lesion on free smooth surfaces is usually located near the gingival margin. It is whitish and rough in texture (Figure 12.3a). In contrast, a typical inactive lesion is often seen in primary incisors at a distance from the gingival margin when the tooth is fully erupted, is hard on probing, and the lesion may be shiny (Figure 12.3b).
Approximal surfaces
Radiographic examination is the most commonly used method for detecting and assessing caries lesions on approximal surfaces with adjacent contacting surfaces. The early, noncavitated lesion on these surfaces is, however, not possible to detect in the radiographic image [9] and usually not from direct visual–tactile examination either. It is important to bear in mind that the proportion of false‐positive diagnoses from bitewing radiography is relatively high in low caries prevalence populations. Details on the validity of radiographic caries diagnosis are described in Chapter 8.
For an approximal caries lesion contacting a neighboring tooth, the border between nonoperative and restorative treatment is the presence of an obvious clinical cavity on the tooth surface. This diagnostic decision is therefore crucial. However, on this matter the radiograph does not give straightforward information. An example of this is shown in Figure 12.7, where only one of two lesions with similar radiographic appearance had a clinical cavity. Studies comparing the radiographic and clinical appearance of approximal lesions in children and young adults report great variation. The percentage of clinical cavities of surfaces with radiolucencies in the outer half of the dentin varies between 41 and 100%, the median (mean) values being 78% [12–18]. The most likely reasons for this variation are different methods used to record the presence of a cavity, different depths of the lesions investigated, and different populations with different caries activity in the various studies. It is obvious, however, that the deeper the lesion, the more likely is cavitation.
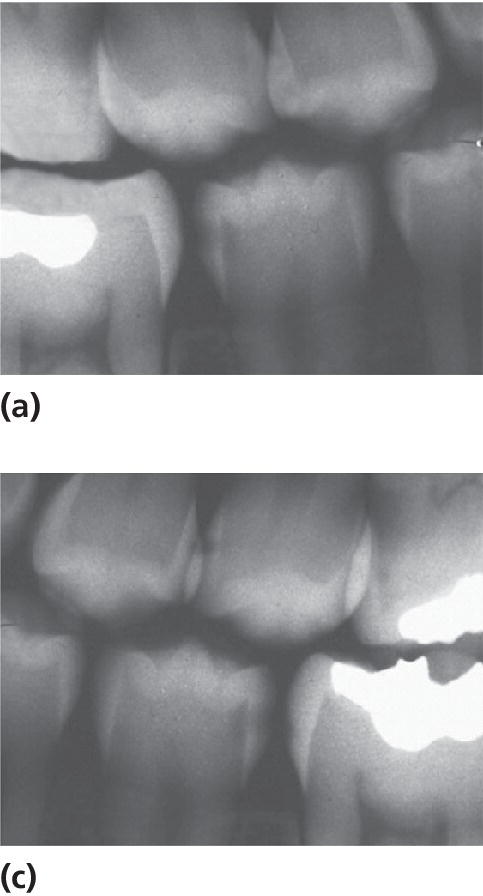
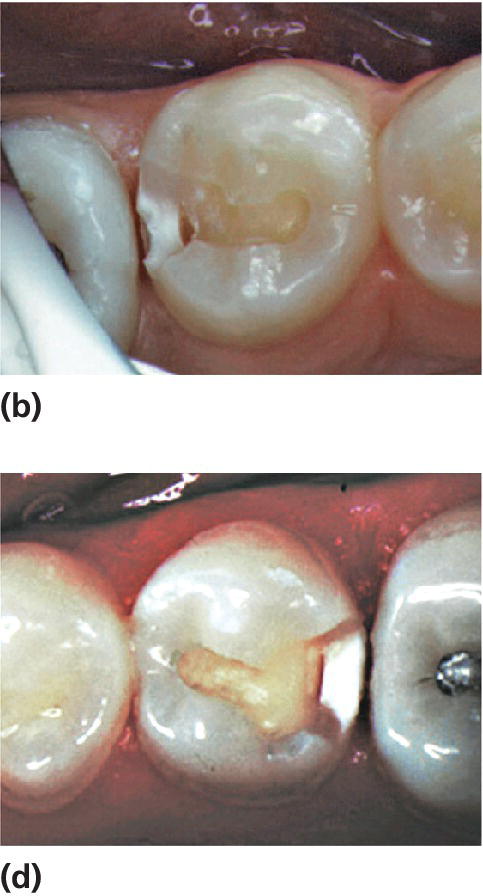
Figure 12.7 Caries lesions on distal surfaces of two mandibular second premolars: both radiographs (a and c) showed radiolucency in outer dentin, but during cavity preparation, a clinical cavity was observed only in one of them (b).
Some clues are useful to assess the probability of the presence of a cavity. Cavitation was more frequently found in A2 and A3 lesions (Figure 12.2b) in individuals with high caries activity than in those with lower caries activity [14]. Cavitated lesions were found more frequently in surfaces with gingival bleeding [19,20]. Tooth separation will allow gentle probing to assess the presence of a cavity. The use of an impression of the approximal surface can be helpful for diagnosing borderline cases [14,17,20]. Admittedly, we lack a simple and valid method for assessing the presence of a cavity on the approximal surface contacting a neighboring surface.
It is likely that the extensive use of fluorides has led to a change in the clinical appearance of pit and fissure caries as well as of approximal caries. The finding of a relatively intact enamel surface hiding a dentin lesion is not uncommon (Figure 12.8). Continuous fluoride supply seems to delay the progression of the caries process in enamel as well as the breakdown of the enamel surface over the dentinal lesion. This phenomenon is sometimes called occult caries [21].
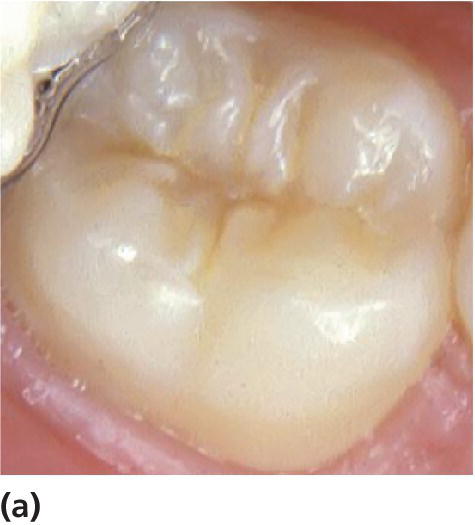
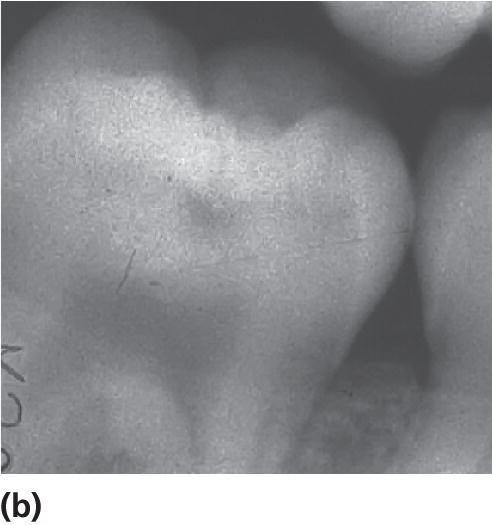
Figure 12.8 Hidden caries under a seemingly sound occlusal surface of a permanent lower second molar in a 14‐year‐old. (a) Visual–tactile examination of the surface did not reveal any clear signs of caries. (b) The bitewing radiograph shows, however, an obvious radiolucency in the dentin. The presence of soft carious dentin was confirmed at drilling.
Alternative/supplementary diagnostic tools
There are a variety of alternative/supplementary caries‐diagnostic tools available to the pediatric dentist:
- fiber optic transillumination (FOTI)
- digital fiber optic transillumination (DiFOTI)
- laser fluorescence (DIAGNOdent)
- near‐infrared (NIR) transillumination technique (DIAGNOcam)
- quantitative light‐induced fluorescence (QLF)
- electronic caries measurement (ECM).
The first five are optical methods and the last one is based on electrical impedance. FOTI (DiFOTI) is used as an alternative to bitewing radiography. Holt and Azevedo [22] compared the diagnostic gain from FOTI and radiography and concluded that in terms of accuracy and reliability, the use of FOTI offered no advantage over radiography. In situations when radiography cannot be used, for example children not accepting having radiographs taken, FOTI can serve as an alternative. DIAGNOcam represents a further development of FOTI, but the methods need validation before it can be recommended as a supplement to radiography. In a clinical study, the laser‐based DIAGNOdent detected both enamel and dentin lesions with high sensitivity but at the price of high proportion of false‐positive diagnoses (low specificity) [23]. This suggests a considerable risk of overtreatment when relying on this method. QLF can detect small changes in mineral loss with high accuracy but the method is so far little used in clinical practice. ECM was tested in two studies on extracted teeth [24,25]. High specificity was found in both but sensitivity varied from low to high in the two studies.
In conclusion, each of these alternatives and supplementary diagnostic tools has shown advantages and drawbacks. A systematic review concluded that there is not sufficient evidence to decide on the accuracy of these diagnostic tools [26].
The concept of caries treatment
There has been a strong tradition in dentistry to associate caries treatment with restorative techniques, and to use the term prevention for methods aiming at preventing this kind of treatment. The major drawback with this way of thinking is that it makes dentistry restorative focused. This affects how we make treatment decisions, how we judge the value of restorative treatment, and how resources are allocated. However, since the signs and symptoms of dental caries are the result of a disease process, our treatment should aim at arresting the disease process before repair of destroyed tissue is needed [27]. In other words, the primary treatment objective should be to manage the disease by nonoperative measures, while repair of destroyed tissue should come second. It follows that it is very important that resources be allocated accordingly.
Nonoperative treatment aims at reversing, arresting, or postponing progression of the caries lesion and should be the choice of treatment whenever possible. Surgical correction of a medical chronic disease is not effective. Therefore, operative treatment should be used only when progression of the caries lesion cannot be prevented, that is, when the lesion is cavitated and adequate plaque control cannot be obtained. From one perspective, nonoperative treatment of noncavitated lesions and operative (restorative) treatment of more advanced lesions both have the same main objective, that is, to prevent the disease from further progression leading to further tissue destruction, infection of teeth and other tissues which may create pain, suffering, and reduced function. The major difference between nonoperative and operative treatment is the long‐term benefit of an unrestored tooth.
Nonoperative treatment
The nonoperative treatment techniques are the same as those used to prevent caries, that is, oral health behavior counseling, fissure sealing, and use of fluoride. Nonoperative treatment is used mainly for noncavitated lesions, but there are exceptions such as the management of cavitated lesions in small uncooperative children (see the section “0–3 years”).
The most commonly used techniques are:
- General intervention (patient‐oriented): The basic and most important measure is to motivate and teach the patient how to remove dental plaque covering the caries lesion, to keep the lesion clean on a daily basis with the use of fluoride toothpaste. Diet counseling may also be included. In special cases, when the patient and/or the parent are unable to clean the teeth, professional plaque removal may be indicated [28] (Figure 12.9).
- Local intervention (lesion‐oriented): Fissure sealing is used to treat noncavitated caries lesions in pits and fissures. This treatment concept is based on the assumption that a properly placed sealant prevents micro‐leakage from the oral environment. Thereby, supply of nutrients to bacteria in the caries lesion is restrained and the caries process arrested. There is support from the literature that the caries process does not progress as long as the seal is intact, and this applies to both enamel and dentin caries [29–33]. Evidence for the effectiveness of sealing noncavitated caries lesions in pits and fissures in clinical practice is, however, incomplete [34,35]. Notably, this does not prove that the technique is not effective; lack of evidence of effect may rather be due to scarcity of well‐designed and well‐performed clinical studies in contemporary populations. In a systematic review from Cochrane the application of resin‐based sealants is a recommended procedure to prevent and control caries in permanent first molars [36]. Furthermore, recently, a systematic review concluded that occlusal fissure sealing with a resin‐based sealant may arrest the progression of noncavitated occlusal dentinal caries [29]. However, further clinical trials with longer follow‐up times must be performed to strengthen the scientific evidence.
- Fluoride varnish application is a medicinal mode of treating noncavitated caries lesions. When topical application of Duraphat® was used in teenagers every third month during a 3‐year period, the progression rate of approximal lesions in premolars and molars was reduced significantly [37]. This procedure requires resources in terms of professional personnel, time, and equipment but this should be weighed against the benefits. Thus, if successful, this treatment is so much more valuable to the child than a restoration, because it preserves sound tooth tissue. As for fissure sealants, the evidence for the effectiveness of fluoride varnish for treating noncavitated caries lesions is incomplete, implying that there is a need for more studies in this field [34,35].
- Glass ionomer cements (GIC) may be used as a temporary sealant in fissures and other lesions, based on their cariostatic and fluoride‐releasing properties. This is described later in this chapter.
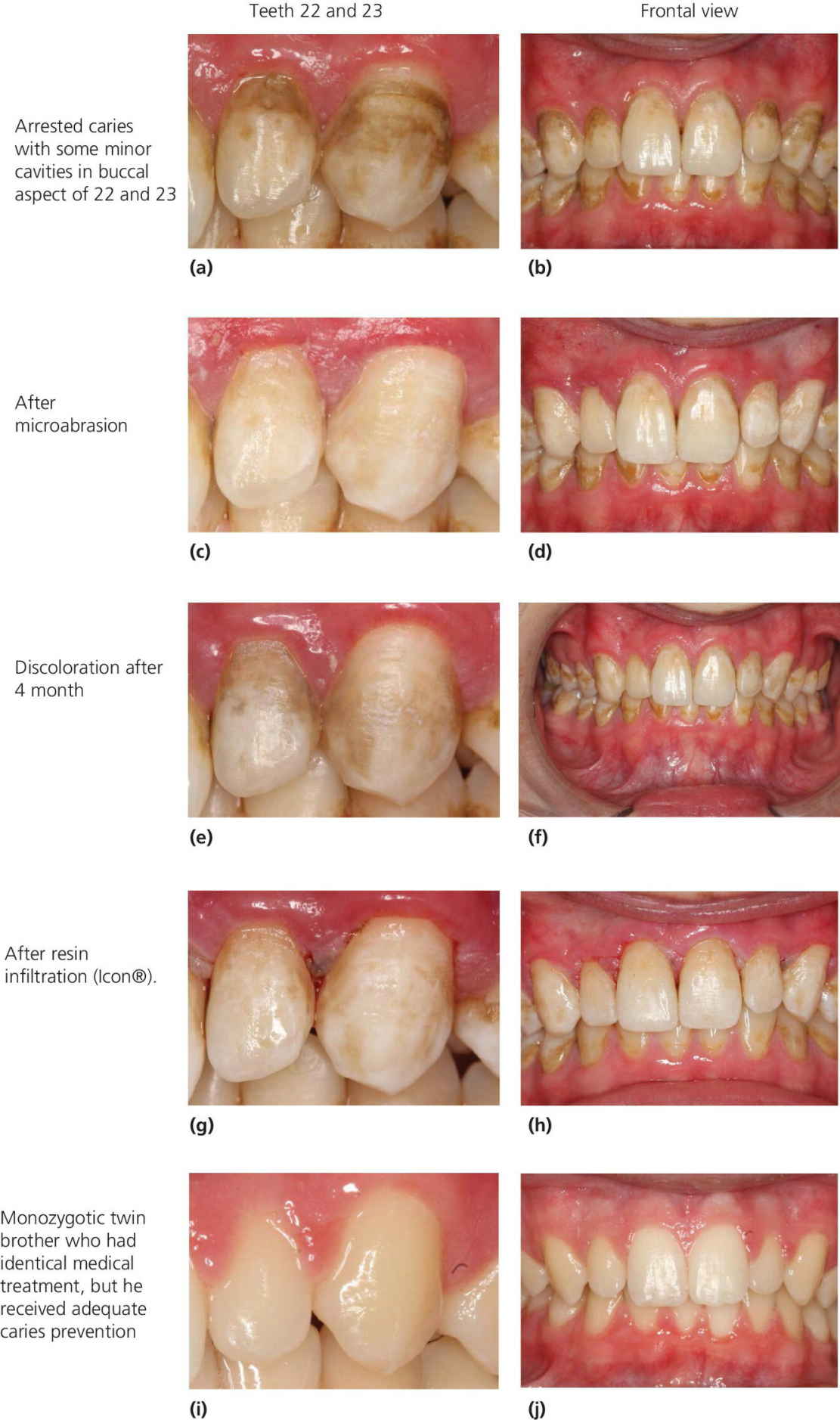
Figure 12.9 (a) to (j) A 14‐year‐old boy who was treated with bone marrow transplantation (BMT). Three months later he developed graft‐versus‐host disease, which prolonged his hospitalization to a total of 4 months. His condition and the treatment he received resulted in hyposalivation, and during the treatment period he experienced frequent supply of sugary drinks, inadequate dental hygiene, and little fluoride exposure.
Photos (a) and (b) show situation 16 months after BMT. Reproduced with permission of Eva Gudrun Sveinsdottir.
Operative (restorative) treatment
Irreversible loss of tooth substance and surface continuity has occurred when tooth mineral is lost to the extent that a cavity is formed. This is a critical stage since—unless plaque is effectively removed from the surface of the cavity—destruction of hard tissue will continue. Strictly speaking, the critical border between nonoperative and operative (restorative) treatment is when the patient cannot remove plaque effectively. That border often corresponds to cavity formation (codes 3–6 in Figure 12.2a). This particularly applies to occlusal surfaces and approximal surfaces contacting a neighboring tooth. On buccal and lingual surfaces, even a lesion with an obvious cavity can be arrested without placing a restoration since the surface is accessible to cleaning with the toothbrush (Figure 12.9).
Most restorative techniques include irreversible loss of sound tooth tissue and therefore permanently weaken the tooth. Furthermore, restorations do not last forever and as a filling is replaced, the cavity becomes larger and the tooth further weakened. This is true particularly for Class II restorations in primary teeth. Their longevity is further discussed later in this chapter. With Class II restorations there is also a considerably increased risk of iatrogenic preparation damage to the neighboring approximal surface resulting in an increased risk of lesion progression of the damaged surface [38,39]. It follows that there are several reasons to scrutinize whether operative treatment is in the best interest of the patient.
Before deciding to restore, the following factors should be considered:
- The potential for plaque removal. The potential for lesion arrest depends on whether or not plaque can be removed from the surface of the cavity. In principle, plaque covering a cavity on a buccal or lingual surface can be removed by the patient with a toothbrush. The critical question is therefore: will the child or the parent be able to clean the cavity effectively? Whether or not this can be done properly has to be decided for the individual patient. Particularly in small children where cooperation for restorative treatment is not optimal, the best option could be to teach the parent to remove plaque from the lesion, that is, to turn an active cavitated lesion into an inactive, arrested lesion. The patient cannot clean an obvious cavity on an approximal surface with a contacting surface effectively—even flossing will only slide over the surface—and the lesion should therefore be restored. The same applies to most cavities on occlusal surfaces. The molar in Figure 12.5 could serve as an example. The cavity in this permanent first molar cannot be cleaned effectively by the patient since the toothbrush cannot reach the cavity floor because of the undermined enamel. This cavity should therefore be restored.
- Lesion activity—active or arrested lesion. If there are signs of arrest of a cavitated lesion, restorative treatment may be unnecessary [40]. This mostly applies to buccal and lingual lesions. Assessment of caries activity is often difficult for lesions not accessible to visual examination, that is, approximal surfaces in contact with adjacent teeth. Several approximal caries lesions or fillings in an individual often indicate high caries activity with an overall increased risk of relatively fast lesion progression. However, even for the caries‐active individual, the rate of progression for a given lesion is difficult to estimate. The only means of deciding whether the lesion is active or arrested is therefore to observe it from repeated radiographic examinations. Here it is important to realize that even with radiographs of good quality, small differences in projection, darkness, and/or contrast can make it difficult to assess whether the lesion has diminished, progressed, or is unchanged. Although it is likely that noncavitated caries lesions visible radiographically can be arrested, the scientific evidence for it is incomplete [9,34].
- Influence of caries prevalence in the population on the risk of overtreatment. The interpretation of the radiographic image is always associated with risks of making false‐negative and false‐positive diagnoses (see Chapter 8). The risk of overtreatment mainly concerns approximal lesions. The reason is that the proportion of false‐positive radiographic diagnoses is relatively high in low‐caries prevalence populations. In other words, the predictive value of a positive diagnosis is low. This can be compensated for by adopting the philosophy of “when in doubt, wait” for borderline cases.
Indications for operative (restorative) treatment of primary teeth
There are several indisputable reasons for maintaining a healthy primary dentition (Box 12.4). However, the benefit and effectiveness of restoring primary teeth are sometimes questioned by practicing dentists as well as by parents of preschool children. The risk of toothache, if not restoring carious primary teeth, was investigated in two studies from England. In one [41], total caries experience in primary molars was the main predictor of pain, while increased levels of restorative care did not lead to either reduced levels of reported pain or to fewer extractions. The authors concluded that if restorative care is not an important factor in predicting dental pain but total decay experience is, then prevention of the disease rather than its repair should form the focus of care for young children. The other study [42] found that 82% of caries lesions extending into the dentin, but left unrestored, exfoliated without symptoms, while 18% had caused pain and were extracted or otherwise treated. The carious teeth most likely to cause symptoms were found in molars that developed cavities with pulpal involvement by the age of 3 years, 34% of which caused pain. Both studies were retrospective and they have several methodological flaws. Bitewing examination was not used and the severity of the lesions at the time of restoration is not stated. In the study by Milsom et al. [41] the involved general practitioners were not selected randomly and—perhaps the most serious flaw—the children were not randomly assigned to restoring or not restoring the carious teeth. It is remarkable that restored teeth suffered the same fate as unrestored teeth. This could, however, occur if the lesions were in advanced stages with pulp involvement at the time of restorative treatment. The quality of restorative care may therefore be questioned. Furthermore, the only outcome measure was pain whereas other important parameters were not considered (see Box 12.4). Admittedly, however, there is a need for prospective randomized clinical trials designed to evaluate at what ages and which primary teeth benefit from restorative treatment [43].
Treatment planning
Treatment planning for the individual child includes the strategy that one applies after having examined the child and recorded its history. Any treatment action must be adjusted to the child’s age, maturity, and ability to cope. This is dealt with in Chapter 6. The treatment is divided into four stages (Box 12.5).
Stage 1: acute treatment
This stage particularly applies to the highly caries‐active child. The treatment aims at relieving the child from acute pain and discomfort, or preventing any immediate threat of such suffering. The most commonly used therapies are extraction, pulp treatment, or excavation of deep caries lesions with subsequent application of temporary fillings (Figure 12.10). Acute treatment in children with coping problems should be carried out under conscious sedation or general anesthesia (see Chapter 9).
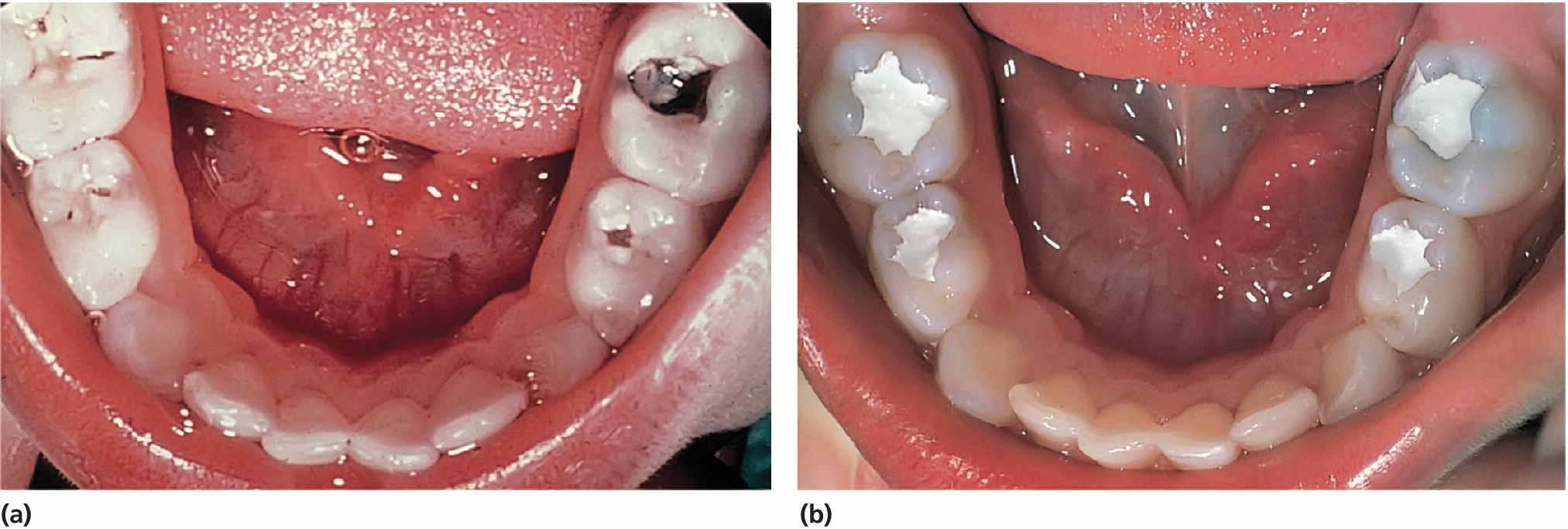
Figure 12.10 (a) A 3‐year‐old boy with high caries activity due to frequent intake of high sucrose‐containing meals. (b) After gross excavation of the caries lesions and application of a temporary zinc oxide–eugenol cement the child is ready for nonoperative treatment.
Stage 2: management of the caries disease; general and local interventions
This stage is based on a general consideration of the caries situation, starting with an estimation of the caries activity. Typical signs of active caries are white spot lesions with rough texture, blunt borders, and location close to the gingival line. The higher the number of active lesions, the higher is the activity [44]. In children under regular control and where caries has been recorded over time by the use of a severity grading system, the degree of progression of lesions is also helpful for assessing caries activity. Based on the findings, general and local interventions as described previously in this chapter (section “Nonoperative treatment”) should be applied. In individuals with active caries, stage 2 is the most important phase since it involves treatment of the disease itself. In the most difficult cases, it may take months or even years before the disease is brought under sufficient control so that placement of the “final” restorations can be made. The long‐term goal should be to reduce the need for restorations and thereby ensure the individual’s oral and dental health for a lifetime (Figure 12.11).
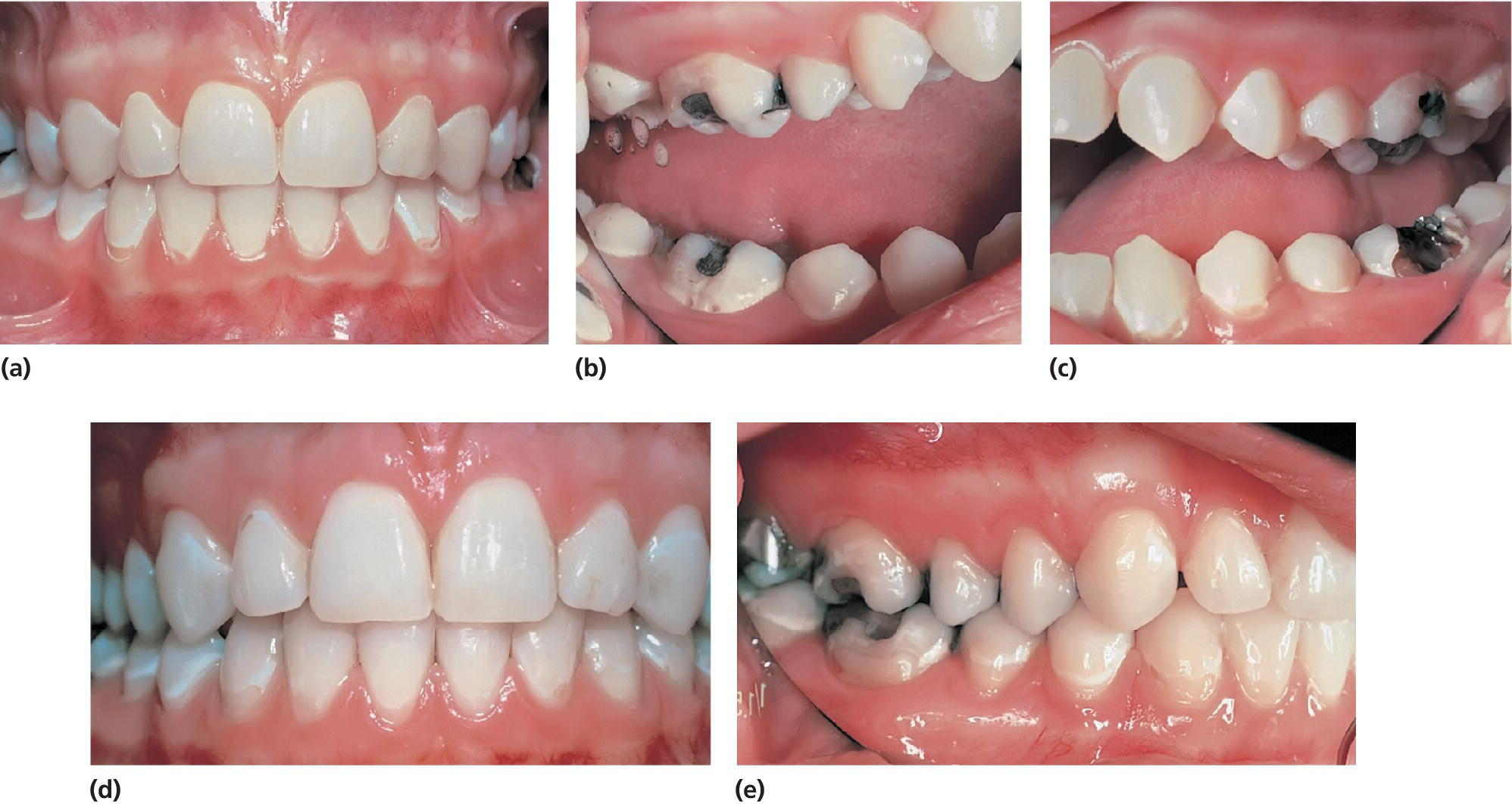
Figure 12.11 (a–c) A 13‐year‐old girl with active caries and low motivation, treated by the use of general and local caries‐arresting interventions. (d) Five years later: adequate caries control. (e) Another 3 years later: still adequate caries control. Observe the glossy surfaces of the previously active initial caries lesions.
Stage 3: restorative (operative) treatment
The operative treatment of caries lesions is usually based on traditional techniques that involve the complete removal of soft, demineralized dentin and aims at preventing the caries process from further progression as well as restoring the tooth to its original size and form (and color). However, the principle of total caries removal is questioned and it has been suggested that the total removal of infected dentin is not necessary for the success of caries treatment [40,45]. More conservative approaches such as minimal intervention techniques for the management of caries have been adopted and are becoming more widely accepted in efforts to address and reduce the adverse consequences of restorative treatment. In addition, there is no evidence that the total removal of carious tissue had better performance than minimally invasive procedures in arresting caries lesions.
In a recently updated Cochrane systematic review [46], stepwise, partial, and no‐caries removal was compared with complete caries removal for managing caries in both primary and permanent teeth. The conclusion of the review was that for symptomless and vital teeth, these minimally invasive techniques had clinical advantages over complete caries removals in the management of dentinal caries.
- The stepwise excavation is an established technique and option for the treatment of deep caries lesions. It involves initial excavation, in which the necrotic and disorganized tissue is removed, leaving soft tissue over the pulp wall. The cavity is then temporarily sealed, allowing the pulp to react and produce tertiary dentin [47]. The cavity is subsequently reopened, and the remaining demineralized dentin is removed. In comparison with complete caries removal, stepwise excavation leads to fewer pulp exposures and provides better outcomes with regard to preserving pulp sensitivity [48].
- Partial caries removal implies that the carious dentin is completely removed from the dentino–enamel junction and lateral walls, while the necrotic carious dentin from the cavity floor was only removed superficially. The hypothesis is that a restoration with an adequate peripheral seal, placed over a cavitated dentin lesion, can arrest the progress of caries lesions. The sealing of the cavity contributes to the formation of tertiary dentin and sclerosis of dentinal tubules, thus preventing pulp exposure [40]. However, clinical trials with long‐term follow‐up periods have demonstrated that the cavity sealing is an extremely important factor for the success of this technique, regardless of the material used for protection and induction of the remaining carious dentin [49,50]. Compared to complete caries removal, the technique of partial removal demonstrates similar results in terms of carious lesion progression and longevity of the restorations [46]. It has also been reported in recent systematic reviews that partial caries removal appears to be advantageous because it reduces the risk of pulp exposure and postoperative pulpal symptoms [46,51]. However, further studies with longer follow‐up times must be performed to increase the scientific evidence.
Indications for operative treatment are given in the specific sections for the different age groups later in this chapter.
Stage 4: estimation of risk and establishment of follow‐up program
At the end of the treatment period, an individual risk assessment and a subsequent agreement of recall interval are made. The decreased prevalence of caries among children and adolescents in Scandinavian countries has initiated a discussion of the previously accepted and extensively used 1‐year interval (or even shorter) is too short with regard to the most cost‐efficient use of resources. There are two drawbacks with short recall intervals and frequent check‐ups:
- resources that could be allocated to at‐risk patients are used for screening healthy individuals, and
- increased risk for overtreatment.
Regarding the first of these drawbacks, we maintain that all dentists, irrespective of type of practice and payment system, should strive for an optimal use of resources allocated to dental services. The second argument is dependent on the dentists’ skills and attitudes to dental treatment. Dentists who allocate most of their time and interest to restorative care may constitute a risk group for delivery of overtreatment. In contrast, dentists who focus on preventive and nonoperative techniques for treating caries, and who are sufficiently skilled in caries diagnosis and risk assessment, probably run a lower risk of overtreating. Risk assessment is further discussed in Chapters 8 and 11.
Restorative procedures
Restorative materials: basic principles and handling
Due to controversies about possible side‐effects of mercury, amalgam is no longer allowed in pediatric dentistry in Nordic countries. Therefore, the materials of first choice are GICs, compomers, and composites. These tooth‐colored materials represent a variety of possibilities for improved restorative care in the primary as well as the young permanent teeth due to their ability to adhere to the tooth tissues. In accordance with the principles of minimal invasive dentistry, these materials are appropriate for small cavities with restricted loss of tooth substance. The GICs may also have anti‐cariogenic properties from fluoride release [52], while compomers and composites have good esthetic properties.
New restorative materials are frequently launched following the decreased use of amalgam in dentistry, and it may be difficult for dentists to keep up‐to‐date in the field when the manufacturers’ representatives are boasting the advantages of their products. The classification of the materials may also seem confusing, for example the distinction between resin‐modified GICs (RMGIC) and compomers. McLean et al. [53] suggest a nomenclature for the classification of adhesive materials, and two reviews describe the properties and possibilities of these materials [54,55]. The general characteristics of GICs, compomers (polyacid‐modified resin composite), and composites are summarized in Table 12.1. Uncured resins and degradation products are released from resin‐based restorations like composites, compomers, and RMGIC. Although these materials have been on the market for decades we know little about the potential biological effects of resin‐based filling materials [56]. Adverse effects possibly caused by resin‐based dental materials should also be taken into consideration when there is a choice between using conventional GIC (polyalkenoate cements) and resin‐based materials in primary teeth.
Table 12.1 General characteristics of GICs, compomers, and composites
| Material | Strength and wear | Adhesion | Handling | Fluoride release |
| GICs; conventional and resin‐modified | Low fracture strength. Low wear resistance | Moderate to enamel and dentin | Sensitive to mixture procedure, capsules are recommended. Relatively slow setting reaction and low early strength | High, possibly caries preventive. Reloads fluoride |
| Compomers | High fracture strength. High wear resistance | High to enamel (acid etch) and dentin | Easy handling. High early strength. Moisture sensitive | Low, probably not caries preventive |
| Composites | Very high fracture strength. Very high wear resistance | High to enamel (acid etch), and dentin | Bonding procedure may be complicated. High early strength. Moisture sensitive | No |
The conventional GICs adhere to both enamel and dentin and they release fluoride. This occurs mostly during the maturation phase in the first week after application. Still, the low tensile strength and brittleness exclude their use in stress‐bearing areas in permanent teeth, other than as a temporary filling material. To improve the physical and esthetic properties, and to allow a fast set, RMGICs have been developed. The setting mechanism is a combination of light‐induced curing and the acid/base reaction. However, they are not considered appropriate for stress‐bearing Class II restorations in permanent teeth. High‐viscosity GICs may be used in small Class II restorations.
The idea behind the polyacid‐modified composites (compomers) is to combine the advantage of fluoride release with improved physical properties. The release of fluoride from compomers is, however, comparatively small and of questionable clinical importance. The advantage of the dual setting mechanism has also been questioned.
The properties of composites have improved continuously during the past decade, and today a number of composites can be used for posterior stress‐bearing restorations. The material requires pretreatment of enamel and dentin in order to adhere to these tooth structures. More details about restorative techniques, material properties, and longevity of restorations are given below.
Rubber dam
Acid etching of the enamel and the use of a dentin adhesive are procedures that are extremely sensitive to moisture contamination, and isolation with a rubber dam is therefore preferable. The rubber dam is used for two purposes in restorative dentistry:
- to isolate the operation field from the rest of the oral cavity, and
- for moisture control.
In Scandinavian countries, a rubber dam in restorative dentistry is used mostly for placing composites and other moisture‐sensitive filling materials. However, it is acknowledged that the use of a rubber dam facilitates all restorative work in children and increases the quality of the restoration. Thus, the use of a rubber dam during the whole sequence of preparation, filling, and polishing procedures prevents movements of the tongue, cheek, lips, and saliva ejector interfering with the procedures. It also gives a much better control of the operation field. It must be emphasized though that the use of clamps and dental floss to attach the dam to teeth may be associated with pain, and this must be prevented by the use of local analgesia (injection or topical). Another concern related to use of a rubber dam is the increased prevalence of allergic reactions to latex, which should encourage the use of latex‐free rubber dams.
The procedures for applying a rubber dam in two common situations are described in Box 12.6 and illustrated in Figures 12.12 and 12.13. In the first example, the main purpose is to isolate the operation field in the posterior quadrant during the procedures of drilling and filling primary molar teeth (Figure 12.12). The second example is the upper front region where the main objective is to keep the operation field dry (Figure 12.13).
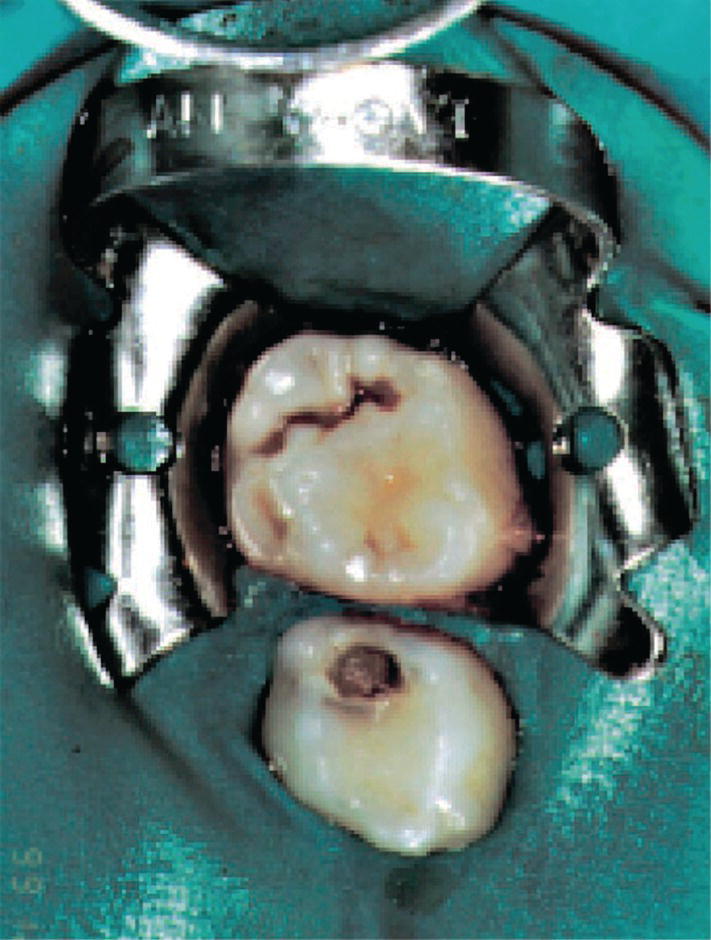
Figure 12.12 Rubber dam for isolating the operation field before restorative therapy of primary molars.

Figure 12.13 Rubber dam for isolating and drying the operation field before restorative therapy of maxillary incisors.

VIDEdental - Online dental courses


