Child Abuse and Neglect: The Dental Professionals’ Role in Safeguarding Children
Göran Dahllöf, Therese Kvist, Anne Rønneberg, and Birgitte Uldum
Children are abused and neglected all over the world, every day. It is essential to recognize children who live under harmful conditions in order to protect and support them from negative health development. All professionals in dental care in the Nordic countries are legally mandated to unconditionally and immediately report any suspicion of child abuse and neglect to the social services. The dental team is in a unique and good position to recognize children at risk as they often meet children and their families on a regular basis throughout the childhood, and as signs of child abuse and neglect and domestic violence can manifest in and around the head and neck area or in certain behaviors. Having up‐to‐date knowledge of how to recognize and manage child abuse and neglect is an important part of dentistry.
Definition of child abuse and neglect
Child maltreatment is often used as a universal term for all types of abuse and neglect. There are four types of abuse included in the term “child maltreatment”: physical abuse, emotional abuse (intimate partner violence included), sexual abuse, and neglect [1]. In Table 26.1 the definitions for each type of abuse are explained. Dental professionals are obliged to report all types of abuse and for that reason this chapter uses the term child maltreatment with type of abuse further specified when needed.
Table 26.1 Definitions of child maltreatment and its components.
| Type of abuse | Definition |
| Child maltreatment | Any act of commission or omission by a parent or other caregiver that results in harm, potential for harm, or threat of harm to a child. Harm does not need to be intended |
| Child physical abuse | Intentional use of physical force or implements against a child that results in, or has the potential to result in, physical injury |
| Child sexual abuse | Any completed or attempted sexual act, sexual contact, or non‐contact sexual interaction with a child by a caregiver |
| Child psychological abuse | Intentional behavior that conveys to a child that he/she is worthless, flawed, unloved, unwanted, endangered, or valued only in meeting another’s needs |
| Child neglect | Failure to meet a child’s basic physical, emotional, medical/dental, or educational needs; failure to provide adequate nutrition, hygiene, or shelter; or failure to ensure a child’s safety |
| Intimate partner violence | Any incident of threatening behavior, violence, or abuse (psychological, physical, sexual, financial, or emotional) between adults who are, or have been, intimate partners or family members, irrespective of sex or sexuality |
Source: Gilbert et al. 2009 [1]. Reproduced with permission of Elsevier.
Prevalence of child maltreatment
Estimating the prevalence of child maltreatment is difficult as it depends on the research method and the definitions used. Some countries use child protection registers whereas in others there are official statistics from police reports, and self‐reports from abusing parents and from abused children. Irrespective of research method, self‐reports result in a higher prevalence figure than official reports, indicating that many cases remain unrevealed [1]. Underreporting from dental professionals to the social services is also common [2].
In industrialized countries the prevalence of corporal punishment varies from 5 to 35%. Sexual abuse of girls ranges between 15 and 30% and of boys it is 5 to 15%. Intimate partner violence varies between 8 and 25% [1]. According to a 2014 report by the World Health Organization, 23% of adults report to have been physically abused as children, 36% report previous experience of emotional abuse, and 16% report child neglect [3]. Two Swedish national population‐based studies found that 13–15% of adolescents reported self‐experienced physical abuse and of these 3–6% reported they had been abused on repeated occasions. Further, 7–10% reported intimate partner violence in their homes [4,5]. Globally, 30% of women report exposure to intimate partner violence [6]. Being exposed to several types of abuse, so called poly‐victimization, is common [4,7].
Risk factors for exposure to maltreatment
Identifying children at risk of maltreatment is difficult. Several factors in combination such as family, child, and the social context often interact and may compound the risk [1,8]. One major risk factor is intimate partner violence. Children who live in families where there is violence between adults are often exposed to physical abuse themselves. In addition, they witness the abuse of another family member, which is psychological abuse in itself [1,4,5,9,10]. Therefore it is important for the general dental professional to recognize adults exposed to intimate partner violence when dealing with child maltreatment and not focus solely on abuse directed towards the child.
Young children and children with functional disabilities or chronic health conditions are vulnerable groups with an increased risk of being physically abused as these groups cannot protect themselves, they may have difficulties expressing what they are exposed to, and furthermore their behavior may confer extreme stress on the parents. Other factors that can increase the risk for maltreatment are low socioeconomic conditions, parents’ own history of being abused as child, parents with substance abuse, and families with parental psychiatric and mental disorders [1,4,9,11,12].
Social services: child protection and support
Child protection and providing support to maltreated children is managed by the social services, the authority that investigates and manages vulnerable social relations for both children and adults. The legal obligation to report suspicions of child maltreatment is regulated and formulated in the social services act in each of the Nordic countries. Reporting a suspicion of child maltreatment to the social services is always with the child’s best interest in focus.
After the report is received at the social services, the report is evaluated for possible investigation. An investigation includes gathering of information on the child’s situation: family, health, and social relations. This process aims to determine whether maltreatment is present and whether the child and family require any supportive or protective intervention. The reporter can be contacted for more information and the reporter can ask for feedback regarding the report and its progress. In a Scandinavian context, the aim of the social services is family oriented and favors collaboration but in other parts of the world such as USA and the United Kingdom, the focus is to protect‐child protection.
Overall, the social services organize interagency cooperation between police, schools and health organizations, and they decide or suggest appropriate interventions according to the social services act. The social services also work with “children’s houses,” which are places for interagency cooperation. Children’s houses offer a setting that make it easier for children exposed to physical and sexual abuse to be met by social services, police, prosecutor, child psychiatry, and pediatric medicine in the same place. Thereby, the child does not have to travel between settings for a medical examination or a hearing. All Nordic countries have children’s houses, but organization and content may vary from country to country. At some children’s houses a dental professional is available upon request.
Recognition of child maltreatment
Child maltreatment can be recognized or suspected when finding physical signs or symptoms, by observing behaviors, either of the child or in the interaction between the child and the adult, or by direct disclosure from a child, a parent or a third party. Child abuse can also be suspected when treating an adult (without having met the child) where a suspicion is raised regarding intimate partner violence. As always, a thorough social, medical and dental history should be taken in the clinical encounter with adults and children.
Physical abuse
Inflicted injuries can be found on the whole body although not always recognizable to the dental professional due its location. Different objects such as hands, belts, and many other things can afflict physical injury. As the facial region is often injured during physical violence, dental professionals have a particularly good opportunity to observe and uncover signs of abuse when the orofacial region is well illuminated during the clinical examination.
Bruising is common after abusive injuries and patterns of the bruises can help to identify a previous abuse [13]. Several colors in the bruise, several bruises and in different stages of healing may indicate injuries inflicted over time. However, estimating the age of bruises is difficult and not recommended as the scientific evidence is weak [13,14].
Inflicted burns can be found in the mouth due to bottle‐feeding infants with overheated drinks or with a hot spoon during feeding or by immersing the child into scalding water. Cigarettes can cause lesions that are small and circular on the skin.
Bite marks on skin can appear as bruises, abrasions or lacerations. They can be caused by animals or humans, perpetrators or victims, children or adults, inflicted as punishment, part of physical or sexual abuse, or self‐inflicted. Cases of children biting their own arm during abuse in order to keep quiet or not cry have been described. Almost 25% of 112 bite marks were found on face and head [15]. As bite marks persist for a varied period of time (from less than 24 hours to 2 or 3 days or longer) it is essential to document a bite mark when it is first noticed. Two half circles opposing each other, occasionally with a central area of ecchymosis between the arches, may be found. A distance of 3 cm or more between the canines may indicate that an adult was involved in the injury [16].
Separating accidental injuries from non‐accidental injuries
When a child presents with an injury in the dental setting, the dentist must evaluate whether the injury is accidental or non‐accidental. Non‐accidental bruises can be separated from accidental bruises on the basis of the age of the child and the pattern of the bruises [17–19]. Small children, unable to walk or crawl, are not likely to have inflicted bruises on themselves by accident and the same applies to children with severe mobility impairment. Bruising on and behind the ears, or on the neck and cheeks in these children should raise awareness of an inflicted injury (Figures 26.1 and 26.2). This “triangle of safety” (ears, side of face, and neck, top of shoulders) is rarely subjected to accidental injury whereas accidental trauma more often occurs in other parts of the body and face (bony prominences) (Figure 26.3a,b). A number of pointers that should raise a suspicion of physical abuse are listed in Box 26.1 [20].
Figure 26.1 Gripping a child’s cheeks during forced feeding will leave an impression of the thumb on one cheek and impressions of the four other fingers on the other cheek.
Image source: Harris et al. 2006 [19]. Reproduced with permission of Committee of Postgraduate Dental Deans and Directors (COPDEND) UK.
Figure 26.2 Slap marks on the cheek. The fingers of the hand will leave impressions. Petechial bruising at a finger width spacing. Marks form between the fingers on the slapped area.
Image source: Harris et al. 2006 [19]. Reproduced with permission of Committee of Postgraduate Dental Deans and Directors (COPDEND) UK.
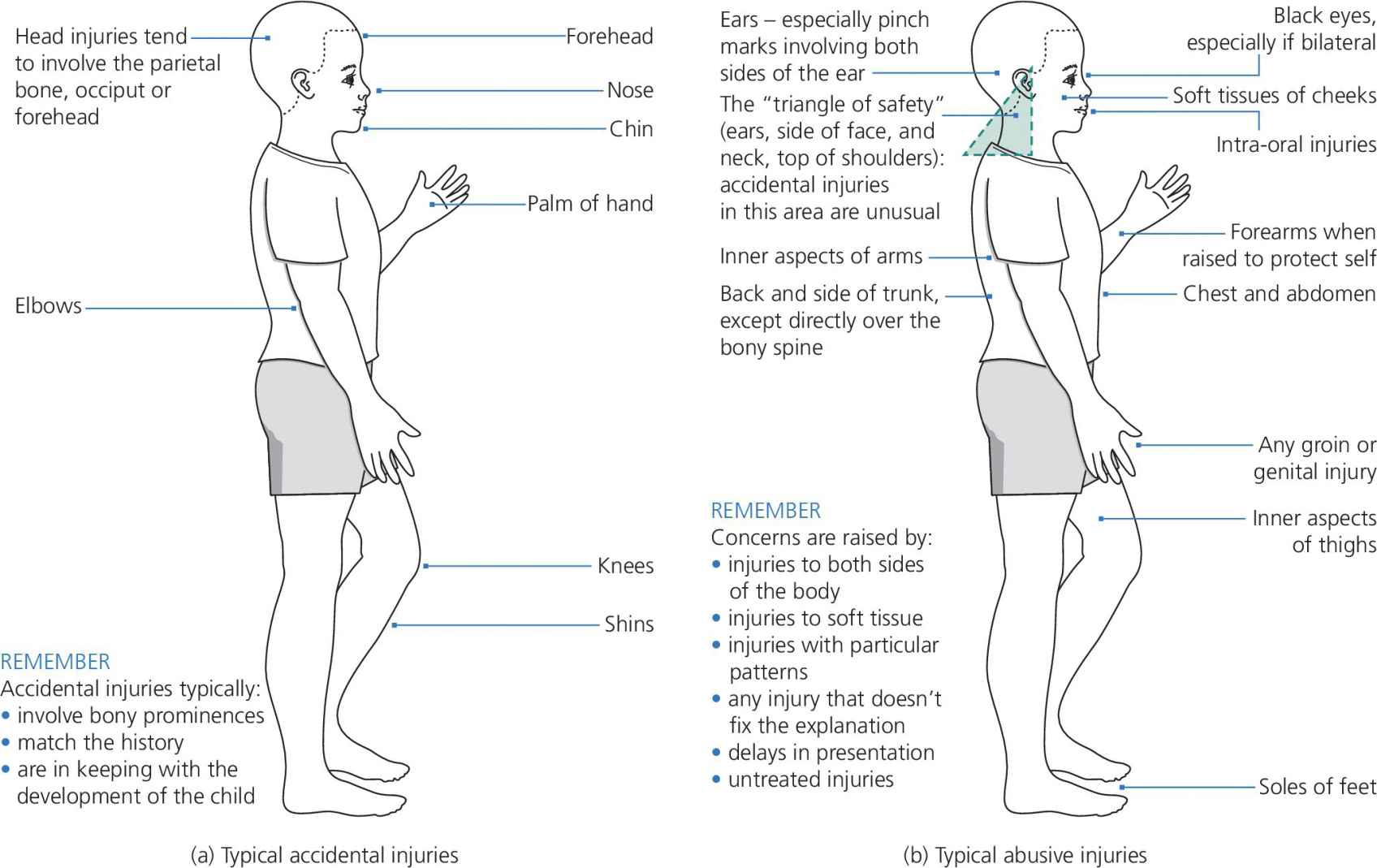
Figure 26.3 Helpful illustrations to distinguish (a) accidental injuries from (b) non‐accidental injuries.
Source: Harris et al. 2006 [19]. Reproduced with permission of Committee of Postgraduate Dental Deans and Directors (COPDEND) UK.
Psychological abuse
Signs of psychological abuse are most likely found when observing the child’s behavior and interactions with those around them. Possible signs in the child’s behavior are emotional frustration, submission, aggressiveness, and lack of concentration and social skills [19]. Older children and adolescents may react to emotional abuse (and other types of abuse) by experimenting with drugs or alcohol, by criminal behavior, by running away from home, or by inflicting injuries on themselves [21]. It can be difficult to distinguish poor parenting from emotional abuse, but behaviors that cause severe problems to children’s development are generally considered as emotional maltreatment. This includes, for example, severe nonresponsiveness, insults or threats towards the child. Emotional abuse also includes intimate partner violence [22].
Neglect
Child neglect can be recognized when parents or caregivers fails to provide basic needs such as food, clothing, medical and dental care, education, and protection from danger [1,19]. Persistent general neglect can result in failure to thrive which manifests as poor weight gain, growth retardation, delayed development, and abnormal behavior [23].
Oral and dental aspects of child maltreatment
Physical abuse
Although studies have shown that the prevalence of intraoral injuries is low, traumatic injuries such as fractures to the teeth, roots and alveolar bone, intrusion, luxation, and avulsion are found [24,25]. Other dental factors shown to be associated with physical abuse and intimate partner violence include unexplained dental traumas both acute and healed, untreated caries, dental behavioral management problems (DBMP), and poor self‐perceived oral health [26–31].
Sexual abuse
Recognition of childhood sexual abuse is difficult as it has various and broad manifestations. Signs recognized by the dental team may be associated with physical, emotional, and dental symptoms. Unexplained injury of teeth or the palate, particularly petechiae at the junction of the hard and soft palate, may be signs of forced oral sex [32]. The child or the adolescent may also react with dental fear as shown in several studies among adult women with previous experience of sexual abuse [33–35]. Poor self‐perceived oral health is also associated with forced sex [31].
Dental neglect
Dental neglect is defined by the American Academy of Pediatric Dentistry as “a willful failure of parent or guardian to seek and obtain comprehensive dental treatment necessary to ensure a level of oral health essential for adequate function and freedom from pain and infection” [36].
As caries has a multifactorial etiology, extensive dental caries is not by default synonymous with dental neglect. Certain features of dental neglect can, however, be identified: failure or delay in seeking treatment for dental caries or trauma, failure to complete a recommended treatment, and allowing the child’s oral health to deteriorate [37]. Signs and symptoms suggestive of dental neglect are presented in Box 26.2. It is important to stress that no signs or symptoms are pathognomonic of child abuse and neglect. Possible differential diagnoses should always be considered (Box 26.3).

VIDEdental - Online dental courses


