Root Morphology
• To understand the functions of the roots of teeth
• To understand how the shape of the root affects the support of the tooth
• To understand how root shape affects the periodontal tissue health and hygiene
• To understand how orthodontic tooth movement is possible
• To understand the anatomical differences between root canals
FUNCTIONS OF ROOTS
Sensory Functions
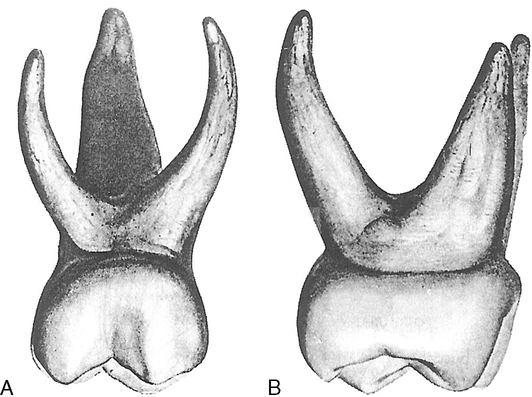
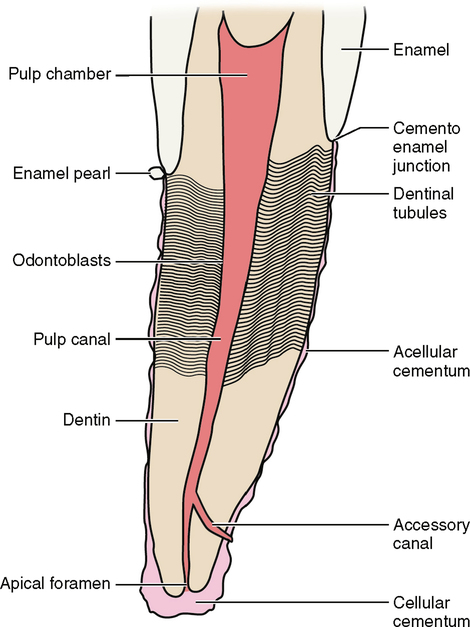
The dentin that surrounds the pulp tissue of the root is itself covered by an imperfect layer of cementum. This patchwork of cementum has bare areas where dentin is exposed. If the tooth root is exposed because of periodontal disease, recession, trauma or any form of pathology, these exposed spots of dentin can stimulate the pulpal nerves through their tubules (Fig. 11-1).
Reparative and Nourishment Functions
Inside the tooth the odontoblasts allow secondary and reparative dentin to be formed in response to trauma (see Chapter 20). This process is not restricted to the root but to the entire pulp chamber.
The apical third of the root at or near its apex can continue to form cementum on the outside of the root. If this process is extreme, it is called hypercementosis, and it forms a cementoma at the apex of the root (see the section on Dental Anomalies in Chapter 7 and Root Formation in Chapter 21). A cementoma is usually associated with bone destruction and or trauma. This cementum is different from the cementum that lines the rest of the root. First, it can continue to grow and add on to itself. Second, in this process of adding on to itself, cells that form cementum are trapped in the cementum. This cementum is called cellular cementum (see Fig. 11-1).
Tooth Movement
On the opposite side of the tooth, the PDL is tensed to accommodate the tooth’s movement. This tension is exerted on the bone. Osteoblastic bone-forming cells respond to the tension by forming new bone (Fig. 11-3).
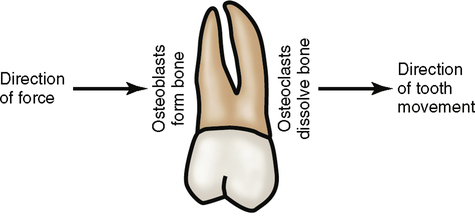
Even without external forces, a tooth still moves. If all of the occlusal forces are removed from a tooth and it has no occlusal antagonist, the tooth continues to erupt. A tooth moves mesially if it does not have another tooth mesial to it; this is called mesial drift (see Chapter 6). The shape of the roots and the residual tension within the PDL may play some part in causing these above phenomena.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses