11
Preventive dentistry
- Prevention
- Fluoride
- Life-long prevention
- Prevention for people with special needs
- Prevention and implantology
- Oral cancer, alcohol abuse, illegal drug abuse
- Smoking cessation
- The primary healthcare team
Introduction
Prevention of disease must be the foundation of all healthcare provision. To avoid invasive treatment, whether it is cardiac surgery or the provision of dental restorations, must be the goal of all healthcare practitioners. Oral health is essential to overall health and well-being and profoundly influences the quality of life, including speaking, eating, and self esteem and has the possibility to disrupt our ability to learn and work.
Oral diseases, particularly dental caries and periodontal disease, are common in the United Kingdom, affecting both children and adults. Most oral health problems are preventable. Oral health is not solely dependent on individual behaviours. Much can be done to reduce oral diseases by using a variety of approaches that include community-based initiatives, self-care, and professional care. There is also much that governments and other authorities can do to ensure that oral health continues to improve. Findings from the Adult Dental Health Survey (2011) show that edentulousness has decreased significantly over the past 30 years and the role of different members of the dental team in the prevention of oral diseases has no doubt played a huge part in the improvements to the health of the population. Surveys such as this one, undertaken every 10 years, are important as this enables the government to develop policies to provide targets and strategies for the promotion of oral health. The Department of Health produced Delivering Better Oral Health: An evidence-based toolkit for prevention in 2009 and this document was developed by a number of well-known experts who have provided contemporary evidence-based oral health prevention and promotion guidelines. The document identifies key areas and comments on how the main problem areas could be addressed by providing clear and simple messages for setting targets for improving the oral health of the individual.
Definitions of prevention
Prevention can be defined as preventing either the onset or the progress of a disease or to restore function lost due to disease. Prevention can be divided up according to the stages of disease prevention, and can be categorised into primary, secondary and tertiary prevention (Table 11.1). However, not all disease prevention strategies fall into a single category of primary, secondary or tertiary prevention; e.g. dietary advice could fall into either primary prevention to prevent dental caries from occurring in the first place, or secondary prevention to prevent dental caries that has already occurred in one or more teeth from progressing further.
Table 11.1 Primary, secondary and tertiary prevention applied to oral and general health interventions.
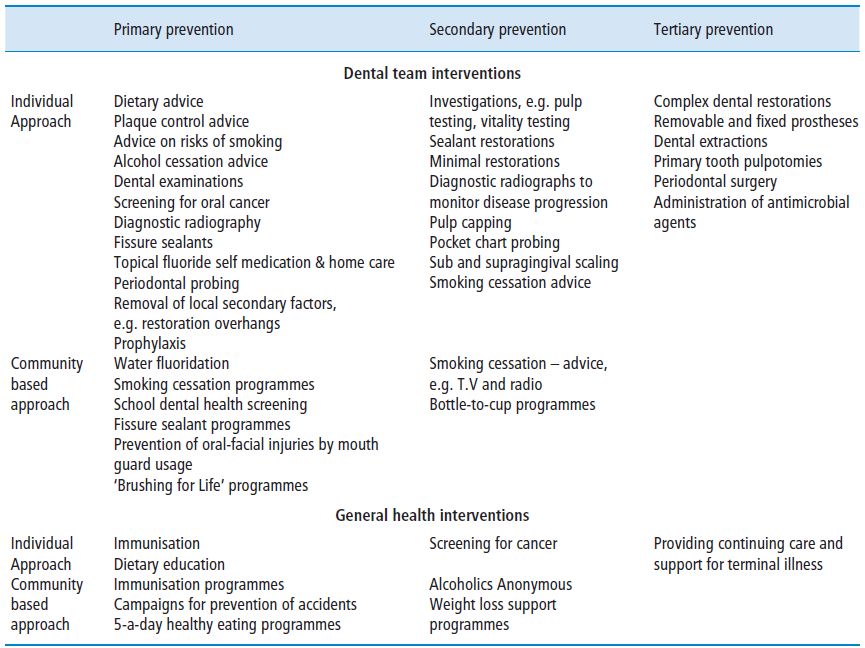
Primary prevention
Primary prevention protects individuals against disease, such as immunisation, and prevention of the initiation of the disease, as in dietary advice and plaque control within dentistry. Primary prevention is aimed at keeping an individual and a population healthy and to minimise the risk of disease or injury.
It is this stage that seeks to implement programmes, procedures, or measures to prevent a disease, before it actually occurs. Programmes designed to prevent people from starting to use tobacco (primary prevention) or to help them quit if they have already started (secondary prevention) can help prevent oral cancer and periodontal diseases, and also be an effective general health promotion strategy. Additionally, plaque control and diet are effective primary prevention methods for both the prevention of dental caries and periodontal disease. Other primary prevention methods include the provision of fissure sealants, water fluoridation and routine dental examinations and diagnostic radiographs.
Secondary prevention
Secondary prevention aims to limit the progression and effect of a disease at the earliest possible opportunity after onset. It refers to the cessation of the disease process and preventing its progressive activity to more advanced stages, as well as preventing the recurrence of the disease, with further primary prevention interventions and advice. Therefore, to stop disease progression and recurrence, once a condition has been recognised, actions are needed to control and eliminate the further spread of that condition.
Removing carious tooth tissue and restoring structure and function at an early stage of the caries process can prevent tooth loss or the need for more extensive treatment. This intervention may be in the form of preventive resin restorations or the placement of more extensive restorations. Secondary prevention measures to diagnose and treat periodontal diseases include periodontal probing and diagnostic radiographs, professional removal of hard and soft deposits, and the local application of antimicrobial agents. Oral examinations of the soft tissues, in addition to obtaining a comprehensive social history to assess past and present tobacco and alcohol use, are also effective measures for detecting oral cancer at its early, most treatable stages.
Tertiary prevention
Tertiary prevention is concerned with limiting the extent of disability once a disease has caused some functional limitation. At this stage, the disease process will have extended to the point where the patient’s health status has changed and will not return to the prediseased state. Tertiary disease prevention refers to the rehabilitation of an individual, and with respect to oral disease, the re-establishment and maintenance of the integrity of the oral cavity.
In the dental caries process, tertiary prevention is aimed not only at restoring carious teeth but also must include further primary and secondary prevention in order to prevent further carious attack. This means that in addition to the placement of a restoration, the causes of caries must also be addressed as part of a clinically effective caries management programme. When considering periodontal disease, periodontitis can be treated by a variety of interventions, surgical procedures or by administering antimicrobial agents either locally or systemically but again the aetiology must be identified.
Prevention of periodontal disease
Mechanical plaque control
Effective plaque control is necessary to maintain oral health, as dental plaque is the main aetiological factor in both periodontal disease and dental caries. There are so many oral care products available on the market, that it is easy for consumers to feel overwhelmed by the choice on offer and not select the most appropriate product for their own needs. It is important for dental professionals to consider the manual dexterity, motivation and financial abilities of the individual, and to also consider the available research supporting an evidence base prior to recommending any dental product.
Regular toothbrushing with fluoride toothpaste is arguably the most widely employed method of home dental care. However, in the multicultural society in which we live, not all people use a toothbrush and toothpaste and caution should be exercised as some people may use more natural products such as a ‘chewstick’ or Miswak (tree twigs from the Salvadora persica plant). These products may be effective, although the evidence base is limited, but do not offer the additional benefit of the application of topical fluoride to the tooth surface so may be less effective at preventing caries.
Toothbrushing
The first mass-produced toothbrush was made by William Addis in England in around 1780. The toothbrush as we know it today was not invented until 1938; before then toothbrushes were made with bamboo handles and boar bristles. Nylon bristles made from nylon yarn were first introduced in 1938.
The aims of toothbrushing are to obtain a high standard of oral hygiene by the mechanical removal of plaque from accessible sites and to allow the application of fluoride and other agents to the tooth surface. The western diet, being relatively soft, does little to stimulate the maintenance of healthy keratinised gingivae. The frictional effect of toothbrushing on the attached gingivae, when managed correctly, provides an effective substitute for a more fibrous diet. In periodontal disease, removal of plaque assists in the reduction of the inflammatory process of the periodontal tissues. Twice daily brushing, particularly last thing at night when saliva is decreasing, therefore reducing the washing and buffer effect, is recommended as it plays a key role in the prevention and control of dental caries, periodontal disease and dental erosion.
Over the years, dental professionals have seen many designs of toothbrush on the market. Variations in design include the length, shape, diameter and angulation of the filaments, and heads that contain tongue brushing adjuncts. Oral care companies continue to produce innovative designs in an effort to increase sales and try and achieve the most effective toothbrush both for both plaque control and periodontal health. In reviewing these requirements, the following aspects should be considered:
The ‘ideal’ toothbrush should have
- A head size that is small enough to meet the needs of the individual for whom it is recommended; a toothbrush that is too large to be manoeuvred around the mouth may cause gagging and will not remove plaque more effectively; similarly, a toothbrush that has too small a head will also be ineffective as the individual may tire of brushing because of the excessive time requirement. It is the responsibility of the dental professional to recommend the brush to best fit the needs of the individual taking into account the mouth size, ability to gain access, muscular configuration, and dexterity.
- Toothbrush bristles should be soft or medium in texture and have round ended filaments with a compact arrangement of filaments as this causes less damage to the gingival tissues and reduces toothbrush abrasion at the cervical margins of the teeth. Bristles should also be of nylon texture and made from synthetic rather than natural materials, as natural bristles may be porous and therefore more likely to harbour bacteria and their texture is less predictable.
- The handle should have the correct length and thickness appropriate to the age and dexterity of the individual. It must be easy to use and provide for a firm and comfortable grip. Toothbrush handles can easily be modified if difficulty is experienced with a regular brush handle (Figure 11.1).
Figure 11.1 Examples of modified toothbrushes.

It is important to modify the patient’s existing toothbrushing technique and encourage a systematic approach, so that all surfaces are cleaned; ensuring that the gingival margin area is cleaned by using the modified bass or mini scrubb technique is recommended if the existing technique is inadequate. Parents should be encouraged and shown how to brush children’s erupting teeth, as the occlusal surfaces of erupting first and second molars are below the level of the arch during eruption and are prone to dental caries.
Patients need to be reminded to change their toothbrushes regularly at approximately 3 month intervals or when the bristles have become ‘splayed’ as the toothbrush will then cease to be effective in the removal of plaque.
An adjunct to toothbrushing is interdental cleaning as these are areas that are most covered with dental plaque, as regular toothbrushing appears to be less successful at removing plaque from these sites. There is a body of evidence to suggest that interdental brushes are more effective at plaque removal than dental floss, but the choice of interdental aid should be based on the size of the interdental space and the ability, motivation and compliance of the individual.
Powered toothbrushes
There are a variety of powered toothbrushes available on the market, with these being battery operated or electric rechargeable. They often have a small round head and the head movement is usually oscillating, rotating or counter-rotational. There have been a number of recent studies on the benefits of powered toothbrushes over manual ones and the evidence is equivocal but it has been found that generally manual toothbrushes are as good as electric toothbrushes, if used correctly. However, a systematic review by the Cochrane Collaboration concluded that powered toothbrushes with a rotation oscillation action reduce plaque and gingivitis more effectively than manual toothbrushing (Robinson et al., 2005).
Instances where powered toothbrushes may be more appropriate than manual brushes include children who struggle to brush their teeth, either because of lack of dexterity or lack of motivation, which may be improved particularly if the brush has a timer. Other people who may benefit from powered brushes are the elderly and people with arthritis or other disabilities, who may find it difficult to manage effectively with a manual toothbrush. Additionally, people who have become institutionalised may rely on carers to brush their teeth and the carers may find a powered brush easier to manipulate. However, it must be noted that some powered brushes may be heavy for individuals to use, particularly for those people with hand related problems. Of course brushing of the teeth and supporting structures will only be really effective where the patient is well motivated and has received professional instruction on the appropriate use of the brush, whether manual or powered.
Dentifrices
The functions of a dentifrice are to:
- Assist in removing plaque and stain and polishing the teeth.
- Prevent and reduce dental caries by applying topical fluoride to teeth.
- Prevent gingivitis by the inclusion of antimicrobials.
- Achieve other effects such as desensitisation and whitening.
- Give the patient a feeling of well-being with a pleasant tasting mouth and fresh breath.
The principal constituents of toothpastes are outlined in Table 11.2.
Table 11.2 The constituents of toothpaste.
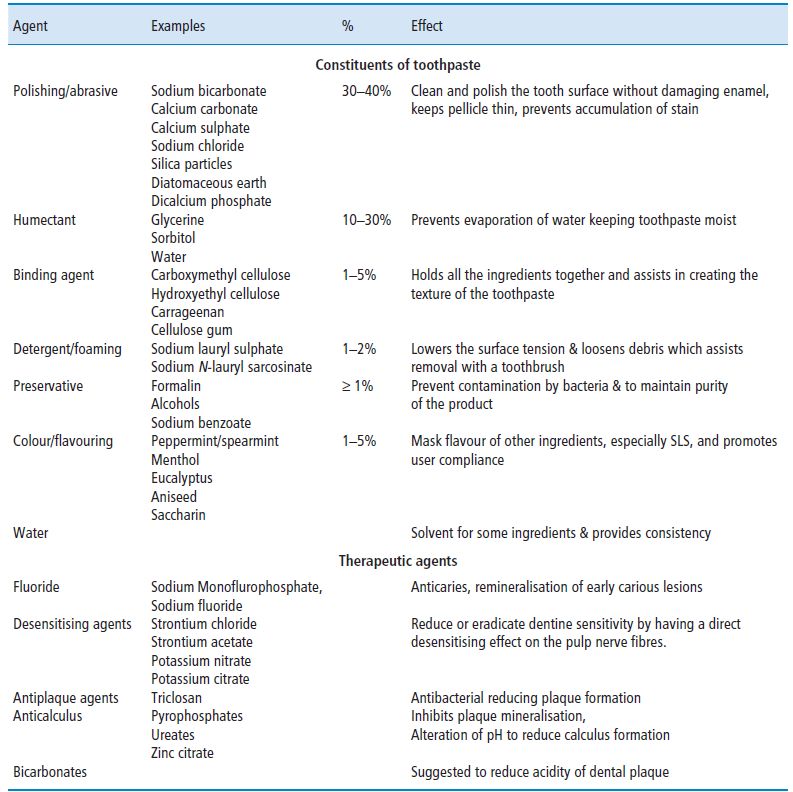
Sodium monofluorophosphate and sodium fluoride are probably the most common fluoride formulations used by toothpaste manufacturers in concentrations from 525–1450 ppm F. Toothpastes containing fluoride were introduced during the 1970s, and the addition of fluoride to toothpaste has contributed greatly to the reduction in caries in UK with reductions of 20–40% over a 2–3 year period of use (Fejerskov and Kidd, 2003). Fluoride toothpastes currently represent more than 90% of the sales of toothpaste products in many EU Member States, such as Germany, France, Italy, Denmark and the UK.
When recommending fluoride toothpaste, dental professionals should consider an individual’s caries risk; this should take into account previous caries experience, dietary habits, socio-economic status and whether fluoride is in the local water supply. Spitting out excess toothpaste, rather than rinsing immediately after brushing, will enable individuals to get an elevated effect of fluoride intra-orally and the full benefits of both the topical and systemic application.
- A family fluoride toothpaste (1350–1500 ppm fluoride) is indicated for maximum caries control for all members of the family over the age of 3, except for those children who cannot be prevented from eating toothpaste.
- Children under the age of 3 should use a toothpaste containing no less than 1000 ppm fluoride using a smear of toothpaste on their toothbrush.
- Parental involvement and supervision is needed to ensure that a small amount of toothpaste is used for children up to the age of 7 years and that the child spits out excess toothpaste.
- Toothpaste containing 2800 ppm or 5000 ppm fluoride is appropriate for adults who have a high risk of dental caries, especially the elderly who are more prone to root caries, those with xerostomia or patients undergoing head and neck radiation therapy.
Prevention of caries
Dental caries is an oral disease often found in young children due to the vulnerability of the tooth surface to acid attack by refined carbohydrates. It has been discussed already (Chapter 4, p. 72) that four factors are necessary for dental caries to occur: these are bacteria, a substrate, time and a tooth. Saliva also plays a role, as teeth are continually bathed in saliva and a reduction in this causes an increase in food retention and a decrease in buffer capacity; this has the potential to cause rapid carious attack.
Prevention of dental caries is by effective toothbrushing, reduction in refined carbohydrates through a healthy diet, use of fluoride and fissure sealants. These aspects are discussed in more detail in Chapters 4 and 7 and the section on Fluoride.
Identifying the ‘at-risk’ individual
Assessing caries risk is important for all patients and the process has to be repeated at regular intervals throughout life to be most effective, as an individual’s circumstances and personal habits can change. People can move from a low-risk to a high-risk group; diet, medication, and radiotherapy can play a part. Assessing risk is important to dental clinicians as this will assist them in determining whether intervention is appropriate and what the recall periods for re-assessment should be for each individual.
Assessing the recall interval
The frequency of review for both the maintenance of oral health and the prevention of disease is currently a contentious issue since there is little scientific evidence on which to base a judgement. Some authorities argue that recall intervals should be relatively short to support a preventive approach to disease management whilst others argue that longer time intervals reduce costs with minimal impact on oral health (Pitts and Pendlebury, 2001). The Scientific Basis of Oral Health Education (Levine and Stillman Lowe, 2004) states that the period between oral examinations must be flexible and based on a professional assessment of the risk from oral disease.
The National Institute for Health and Clinical Excellence (NICE, 2004) recommends that the shortest interval between oral health reviews for all patients should be 3 months. The longest interval between oral health reviews for patients younger than 18 years should be 12 months and the longest interval for patients aged 18 years and older should be 24 months. The recall interval should be reviewed again at the next oral health review, to learn from the patient’s responses to the oral care provided and the health outcomes achieved.
In children, the assessment of those individuals who are considered ‘high risk’ to dental caries ensures that fissure sealants are placed in those who would benefit most from them.
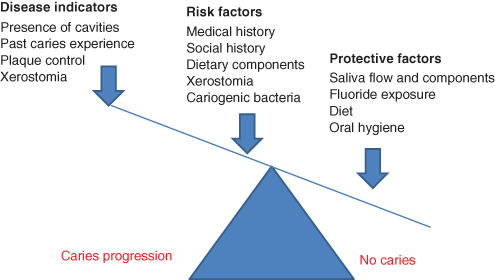
When assessing caries risk a number of factors need to be considered; risk factors will increase our patients’ susceptibility to dental caries and by identifying these allows us to educate our patients on the best ways to manage them.
Aspects that need to be considered include:
- Medical history: cardiovascular disease; bleeding disorders; immunosupression; diabetes; cariogenic medication,
- Social history: socioeconomic status; high caries rate in parents and siblings; motivation towards dental treatment; attendance patterns.
- Dietary assessment: frequent intakes of fermentable carbohydrates.
- Fluoride use: use of fluoride toothpaste; exposure to fluoridated water.
- Dental caries status: presence of new lesions; past caries experience; exposure of root surfaces.
- Plaque control: poor oral hygiene; evidence of plaque retentive factors; presence of high levels of lactobacilli and Streptococcus mutans.
- Saliva flow: xerostomia.
Figure 11.2 indicates the caries imbalance; the balance between disease indicators, risk factors and protective factors determines whether dental caries progresses, halts or reverses.
Figure 11.2 The caries imbalance (Adapted from Featherstone J.D.B (2004) The Continuum of Dental Caries-Evidence for a Dynamic Disease Process. J Dent Res 83 (Spec Iss C):C39–C42, 2004.)
Primary prevention of dental caries in high-risk children
The Scottish Intercollegiate Guidelines Network (SIGN, 2000) and the National Guideline Clearinghouse (NGC, 2009) have published evidence-based recommendations. Children identified as being at high caries risk should:
- Have individual oral health education at the chairside as this intervention has been shown to be beneficial.
- Have emphasised the need to restrict sugary food and drink to mealtimes only.
- Be encouraged to use non-sugar sweeteners, e.g. xylitol in food and drink.
- Be encouraged to use sugar-free chewing gum when this is acceptable.
- Have dietary analysis regularly reviewed and as previously described; fissure sealing should be considered.
- Be considered for a fluoride varnish, e.g. Duraphat applied professionally every 4 to 6 months.
Fluoride
History of fluoride in caries prevention
The first record of fluoride use dates back to the 1870s when potassium fluoride was advocated for use by pregnant women and children by Erharde who believed fluoride could play a part in the prevention of dental caries in a similar way to iron supplements for blood. At the time there was no scientific basis for this advice; it was only an opinion which appeared in a German publication for ‘rational physicians’.
Sir James Crichton, who addressed the British Dental Association in 1892, emphasised the link between fluoride and dental caries. His address consisted of an inspired guess regarding the importance of fluoride in the diet. He claimed that the improved diet of white bread and food made from fine flour was to blame for the decrease in fluoride content that had previously been present in the population’s diet.
However, it was only through Dr Frederick McKay’s extensive research over 30 years in the early part of the last century that any evidence was produced to support these claims. As a recently qualified dental graduate in 1901, Dr McKay took up a position in Colorado Springs, USA. He soon noticed that many of the residents had a distinctive stain on their teeth, which was known to local residents as ‘Colorado stain’. McKay noticed that only the residents who had lived all their lives in Colorado were affected by the stain. Even those inhabitants who had moved into the area when very young (2 or 3 years old) seemed to escape the minute white, yellow and brown flecks that gave their teeth a mottled appearance. On further investigation over a period of years, McKay established that occurrence of mottling was localised over a definite geographical area and was not influenced by home or environmental factors but all the areas affected all received their water supply from one source. In 1931 McKay, in collaboration with the US Public Health Service, and a chemist called Churchill, published his findings showing an increased level of fluoride in the water supply. However, Churchill emphasised the fact that no precise correlation between fluoride content and mottled enamel had been established, only that an unsuspected quantity of fluoride had been found in the endemic areas.
Chemistry of fluoride action on tooth enamel
Natural fluoride exists in two forms, inorganic and organic but it is only the inorganic form that yields the fluoride ion. Inorganic fluoride can be either ionic or non-ionic and it is only the former that is relevant to dentistry and measured in parts per million.
The mineral of tooth tissues exists as a carbonated apatite, which contains calcium, phosphate and hydroxyl ions in the form of hydroxyapatite [Ca10(PO4)6(OH)2]. Carbonated portions weaken the structure and render the tissue susceptible to attack. Food remnants and debris mix with saliva and adhere to tooth surfaces as dental plaque. Bacteria present in the oral cavity, particularly those considered cariogenic such as Streptococcus mutans and Lactobacillus species, metabolise dental plaque and produce acid that lowers the pH of the mouth. When the pH is below the critical level of 5.5 for hydroxyapatite, demineralisation occurs with an outward flow of calcium and phosphorus ions from the enamel surface into plaque and saliva. When the pH returns to 7.0, remineralisation occurs with an inward flow of ions into the enamel surface. If ionic fluoride is present during remineralisation it is incorporated in the enamel to form calcium fluorapatite [Ca10(PO4)6(F)2] according to the following equation:
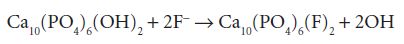
Calcium fluorapatite is more stable and resistant to further attacks than calcium hydroxyapatite.
Fluoride toxicity
Excessive ingestion of fluoride can result in fluorosis (mottling), which presents as opaque or white areas, lines or flecks in the enamel surface and can be cosmetically disfiguring when they occur on anterior teeth. Fluorosis can occur at different times and varies in severity. Figure 11.3 shows very mild dental fluorosis (graded TF1) and Figure 11.4 shows more severe fluorosis (graded TF3) classified by the York review as being ‘of aesthetic concern’. The most important time is when ingestion of excessive fluoride occurs during enamel formation of the aesthetically important permanent upper anterior teeth at between 15–30 months of age, although this period can be extended from birth to 6 years. More severe and cosmetically unacceptable cases of fluorosis are uncommon in the UK but these can result from the use of fluoride supplements in areas where the water is artificially fluoridated or where fluoride occurs naturally at the optimum level of 1 ppm. It has been estimated that about 20% of all enamel defects in the UK are attributable to fluorosis but mainly of the mildest form (TF1). Most of the staining in mottled enamel is confined to the outer 50–100 μm so if treatment is considered necessary this is usually by composite restorations or in severe cases (Figure 11.5) by crowning or veneers. More severe toxicity can result in systemic disease such as osteoporosis and skeletal deformity (Table 11.3).
Figure 11.3 Very mild enamel mottling (fluorosis) – grade TF1.

Figure 11.4 More severe mottling ‘of aesthetic concern’ – grade TF3.

Figure 11.5 Very severe mottling – Grade TF4.
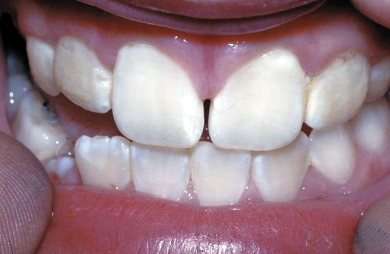
Table 11.3 Potential toxicity of fluoride.
Adapted from NHMRC, 1991.
| Exposure to fluoride (mg/1 drinking water) |
Age | Effect |
| >2 | Child | Dental fluorosis |
| >8 | All ages | Skeletal fluorosis |
| >50 (12 hours) | All ages | Gastroenteritis |
| Pathological doses for exposures other than drinking water |
Age | Effect |
| 5–20 mg/m3 air (occupational) | Adults | Crippling fluorosis |
| 2500–10 000mg oral | Adults | Lethal dose |
| >16 mg/kg oral body weight | Child | Lethal dose |
The most extreme outcome of fluoride toxicity is death. The lethal dose is approximately 15 mg/kg body weight, although as little as 5 mg/kg may kill some children. The exact method that fluoride produces a toxic effect is not known. Symptoms of sublethal poisoning are salivation, nausea, and vomiting. A lethal dose of fluoride will result in death from cardiac or respiratory failure within 24 hours of the overdose. If the overdose is a result of ingestion, symptoms usually appear within 1 hour and therefore if this follows topical application, symptoms may not be seen until after the patient has left the surgery. However, to put this risk into perspective, a 5-year old child weighing 20 kg would need to ingest 0.9 ml (1/5 teaspoon) of sodium fluoride varnish (2.26% F) to have the effects of a sublethal acute poisoning dose, and 4 ml (4/5 teaspoon) for a potentially lethal dose (Kidd, 2005).
Drinking a large volume of milk will neutralise a small dose of fluoride but if the dose exceeds 5 mg/kg ingested or is unknown, medical attention must be sought immediately because of the rapid absorption of fluoride by the body.
It is suggested by some that the impurities in the water fluoridation process can lead to toxicity. Some of the possible impurities include heavy metals such as lead, aluminium and iron. However, the Water Fluoridation Act 1985 gives maximum limits for impurities. Despite this, toxicity from aluminium appears to pose the greatest of concerns to a significant proportion of the population. Aluminium and fluoride are mutually antagonistic in competing for absorption in the gut, therefore the more fluoride in the diet, the less aluminium is absorbed. Aluminium has been implicated as having an aetiological role in Alzheimer’s disease. It follows that if absorption of aluminium is reduced by ingestion of fluoride, this condition may be less common in communities with fluoridated water (Foster, 1993).
Methods of delivery of fluoride
The water supply
Fluoride can occur naturally in the water supply, for example, the water supply of Hartlepool has a natural fluoride content of 1.2 ppm. All water contains fluoride at some concentration because of the natural minerals present (e.g. fluorspar – calcium fluoride – Ca F2). When this dissolves in water it releases fluoride ions:
Throughout the 1930s researchers discovered that people living in areas where drinking water contained naturally high levels of fluoride suffered less dental caries than in other areas. More extensive research demonstrated that, in a temperate climate, a water fluoride level of 1 part per million (1 ppm) was optimal for a significant reduction in dental caries. This led researchers to believe that the benefits of this naturally occurring fluoride could be replicated in areas where the level of natural fluoride was low, by artificially increasing the level to 1 ppm (Lennon, 2004). The concentration of fluoride in water is measured by a fluoride ion specific electrode, which measures free fluoride ions not fluoride bound to metals such as calcium, magnesium, etc.
In 1944, Dr Trendley Dean and his colleagues carried out a trial to test this hypothesis in a community in Grand Rapids, USA, followed by a number of other studies. Dean published his results in 1942 and established that mottling of the teeth was extremely rare at fluoride levels of 1 ppm or below, while the greater part of the caries preventive effect was to be seen at 1 ppm. These results were mirrored at about the same time by a number of other studies in Canada, East Germany, the Netherlands, New Zealand and the UK.
In 1953 the UK Medical Research Council recommended that the Government should send an expert committee to visit the North American trial sites used by Dr Trendley Dean and his colleagues. As a result of the committee’s report, in the mid-1950s the Government established fluoridation schemes in Anglesey, Watford, Kilmarnock and Andover, with detailed reports being published after 5 and 11 years. These reports confirmed the findings of the earlier studies and shortly after their publication the local authorities in Birmingham and Solihull started schemes in 1964 followed by Newcastle a few years later. By the early 1980s approximately 10% of the UK’s population were benefiting from water fluoridation; currently approximately 6 million people in the UK and around 400 million worldwide receive water with the fluoride level adjusted to the optimum level.
In the UK the fluoride compound most commonly added to the water supply is liquid hexafluorosilicic acid (H2SiF6). When this is added to water it releases fluoride ions according to the formula:
Despite the success of fluoridation in the early implementation sites of Birmingham and Newcastle, further efforts to expand water fluoridation to other areas in the UK have been impaired by legislation and a small but vocal antifluoridation movement. The result is that dental caries remains an intransigent public health problem in socially deprived, non-fluoridated areas across the UK. It is estimated that by extending water fluoridation from the current 10% to 25–30% of the UK’s population, targeted at communities with high levels of disease, there would be a substantial reduction in dental caries experience and a reduction in the large inequalities that exists in dental health.
In 1994 a World Health Organization (WHO, 1994) Expert Committee drew the following conclusions regarding water fluoridation:
- Community water fluoridation is safe and cost-effective and should be introduced and maintained wherever socially acceptable and feasible.
- The optimum fluoride concentration will normally be within the range 0.5–1.0 mg/l.
- The technical operation of water-fluoridation systems should be monitored and recorded regularly.
- Surveys of dental caries and dental fluorosis should be conducted periodically.
A systematic review was commissioned by the Chief Medical Officer of the Department of Health to ‘carry out an up to date expert scientific review of fluoride and health’ in 2000, known as the York Review. This was the largest assessment of evidence on the positive and negative effects of population wide drinking water fluoridation strategies. After reviewing 214 separate studies the review found no conclusive negative effects on health from water fluoridation.
In 2004 the British Dental Association collaborated with a number of other organisations including the British Fluoridation Society to produce a definitive document on water fluoridation called ‘One in a Million, The facts about water fluoridation’ (Lennon, 2004). This document aims to inform Strategic Health Authorities and Primary Care Trusts as they consider whether or not to take fluoridation forward in their localities as a result of new legislation (The Water Industry Act) in 2003.
Toothpaste
Fluoride toothpaste has been in general use since the early 1970s and is recognised as being the single most important development in the reduction of dental caries in the last 30 years.
A review of clinical trials going back more than 50 years firmly establishes that, in children, brushing with toothpaste containing fluoride results in 24% less cavity fo/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


