11
Oral Disease
- the causes and risk factors involved in dental caries
- the process of cavity formation, and its progress ultimately to an alveolar abscess
- non-carious tooth surface loss
- the causes and risk factors involved in periodontal disease
- the onset of gingivitis and its progress to periodontitis
- the non-surgical treatment of periodontal disease
- other periodontal conditions
- the risk factors associated with oral cancer
The two main oral diseases of concern to the dental team are dental caries and chronic periodontal disease, and the prevalence of both throughout the human race provides the vast majority of the day-to-day work of dental team members. Other periodontal conditions that may be seen from time to time are also mentioned.
Dental caries and chronic periodontal disease are discussed in detail within this chapter, while full details of oral health assessment and diagnosis techniques, and oral disease prevention are covered elsewhere.
Although oral cancer was discussed in Chapter 7, it is included again here as a worryingly increasing disease condition that may be seen from time to time in the dental workplace, and the importance of the dental team in its early diagnosis and prevention cannot be overestimated.
Dental caries
Dental caries (tooth decay) is a bacterial disease of the mineralised tissues of the tooth, where the strong crystal structure found in both enamel and dentine is demineralised (dissolved) by the action of acids. This allows the softer organic component of the tooth structure to be broken down to form cavities.
The acids involved are created as a waste product by oral bacteria, as they digest the foods we eat for their own nutrition. Although the acids are relatively weak organic ones, such as lactic acid or citric acid, they are strong enough to attack enamel and dentine. Not all the bacteria found in the oral cavity are associated with the production of these acids – the usual ones are:
- Streptococcus mutans (initial stages of cavity formation)
- Streptococcus sanguis
- Some lactobacilli (later stages of cavity formation).
Not all the foods that we eat can be broken down into acids either, but those foods that can easily be formed into these damaging organic acids contain carbohydrates. Foods that consist of protein or fats are not relevant to the onset of dental caries. So in summary, the relevant factors in the development of dental caries are:
- the presence of certain types of bacteria
- carbohydrate foods
- the production of weak organic acids by these bacteria
- adequate time or frequency for the acids to attack the tooth.
The bacteria need to become attached to the tooth surface to be able to digest food debris and initiate dental caries, and they do this by forming themselves into a sticky layer called bacterial plaque.
Bacterial plaque
Millions of bacteria live in our mouths, flourishing on the food that we eat. Some of this food sticks to our teeth and attracts colonies of bacteria to the tooth surfaces. This combination of bacteria and food debris on a tooth surface forms a thin, transparent, protein-containing, soft and sticky film called plaque. It tends to form and stick most readily in areas where it cannot be easily dislodged, such as at the gingival margins of the teeth, in the fissures of teeth, and around the edges of dental restorations. These are called stagnation areas.
The build-up of plaque at the gingival margins of the teeth is directly associated with the onset of gingivitis and periodontal disease.
The plaque that sticks to the tooth surfaces allows the bacteria living within it to turn sugar into weak acids, which in turn dissolve enamel to produce dental caries.
The main micro-organism which initiates the process of caries is Streptococcus mutans. Large numbers of lactobacilli are then able to thrive in the acid environment, and the presence of these two micro-organisms is put to practical use as a test for caries activity. By periodically counting the number of streptococci or lactobacilli in a patient’s saliva, the level of caries activity and the effect of preventive measures can be monitored.
Sugars
As referred to in Chapter 5, all types of food are classified into three distinct groups.
- Protein – such as meats, fish and various dairy products and pulses.
- Fat – such as animal fats and vegetable oils.
- Carbohydrate – natural sugars and starches from fruit and vegetables, and artificial sugars from processed foods.
Of these, only carbohydrates can be turned into acid by bacteria and thereby cause caries – so they are described as cariogenic foods because they are capable of causing caries. The most acid-producing carbohydrates are those which are artificially added during food preparation, and which therefore tend to be based on non-milk extrinsic sugars (NMEs).
As their name suggests, these types of sugar are not derived from milk and have been added artificially during the manufacturing process, rather than being found naturally in the food product itself. The most damaging ones of all are the refined sugars sucrose and glucose (also called dextrose).
Naturally occurring sugars that produce so little organic acid that they are considered harmless to teeth include the following.
- Intrinsic sugars – found naturally in foods, such as fructose in fruits.
- Milk extrinsic sugars – especially lactose.
Refined sugars can be instantaneously turned into acid by the bacteria concerned and available types include table sugar, sugar used in cooking, and sugar added to anything else taken by mouth, whether liquid or solid. Any food containing added sugar can cause caries and some obvious ones are:
- cake, biscuits, jam and sweets
- breakfast cereals
- pastry, desserts, canned fruit, syrups and ice cream
- soft drinks
- hot beverages sweetened with sugar.
Sugar is widely added to many savoury foods too, in order to flavour or preserve them but without making its taste apparent. Such foods can include soups, sauces, canned vegetables and breakfast cereals which are accordingly sources of hidden sugar. Medicines may also contain hidden sugar and can be a significant cause of caries in chronically sick children.
Sugar occurring naturally in milk, fruit and vegetables is not a significant cause of caries. Naturally starchy and fibrous vegetables such as potatoes, carrots, peas and beans are rich in carbohydrate but may be regarded as insignificant causes of caries as long as no sugar is added by producers or during cooking. The prime cause of dental caries is refined sugar (sucrose), processed from sugar beet and sugar cane, and commercial glucose, which together constitute such a large proportion of the manufactured and sweetened food in our diet. Unfortunately, foods containing these NMEs tend to be cheap and readily available in most First World countries, along with acidic drinks such as carbonated fizzy ′pops’.
Acid formation
As soon as the carbohydrate source is eaten, the oral bacteria take the sugar component into the plaque structure and begin to digest it themselves. Within just a minute or two, it is turned into acid by the plaque bacteria and then attacks the enamel surface beneath the plaque. Enough acid is produced to last for about 20 min and in this initial acid attack, a microscopic layer of enamel is dissolved away. This phase is called demineralisation.
At the end of the meal or snack, when the intake of sugar is over, the acid persists for a period of time ranging from 20 min to 2 h before it is neutralised by the buffering action of saliva.
Saliva is the fluid bathing the oral cavity that is secreted from the salivary glands (see Chapter 10). Amongst its many roles, it maintains the mouth at a neutral level, being neither acidic nor alkaline. The measure of acidity/alkalinity of a solution is called its pH level and the neutral level maintained by saliva is pH 7. When the weak organic acids are produced by the oral bacteria, the pH level starts to fall and once it passes the critical pH 5.5, the environment is acidic enough to attack the enamel and dentine of teeth, and produce cavities.
Once neutralisation has occurred, no further demineralisation can take place until such time as more sugar is consumed. In this phase where no more sugar is present in the plaque, some natural healing takes place; mineral constituents naturally present in saliva enter demineralised enamel and restore the part lost by the initial acid attack. This healing phase is called remineralisation.
What happens next is entirely dependent on the frequency of sugar intake. If it is confined to mealtimes only, for example, at breakfast, midday and early evening, there can only be three acid attacks a day on the teeth. The amount of time available for remineralisation will greatly exceed that of demineralisation and the initial phase of caries will be arrested. But if a series of snacks is eaten between meals throughout the day, the reverse will occur. Most processed snacks contain some added sugar and the result is a rapid succession of acid attacks, with insufficient respite between them for saliva to neutralise the acid and allow the healing process of remineralisation to become dominant. Caries can then spread rapidly through affected teeth, as described later.
The longer the sugar stays on the teeth, the longer the duration of acid production. Thus sweet fluids, such as tea or coffee with sugar, which are rapidly washed off the teeth by saliva, are not normally a major cause of caries unless many drinks are taken throughout the day, whereas the much more frequent consumption of very sweet soft drinks by children is far more serious. But, overall, the most dangerous sources of sugar are those which have a sticky consistency when chewed, as it is far more difficult for the natural saliva flow to wash them away. The adherent nature of such foods allows them to cling to the teeth for a very long time, throughout which they are supplying plaque bacteria with the raw materials for prolonged acid formation and demineralisation.
Foremost among these sticky forms of sugar which cause caries are:
- toffee and other sweets
- cakes, biscuits, white bread and jam
- puddings with syrup or treacle.
With our modern diet, added sugar is consumed nearly every time something is eaten, and the teeth are attacked by acid on each of these occasions. If snacks containing such sugar are frequently taken between meals, there will be a corresponding increase in the number of acid attacks on the teeth. The delicate balance between the forces of destruction (demineralisation) and those of repair (remineralisation) will then be completely upset in favour of tooth destruction and irreversible damage will occur.
Thus it is evident that the prime cause of caries is the frequent and unrestricted consumption of sweet snacks between meals. It is not the amount of sugar eaten but the frequency with which it is eaten that is all-important. This fundamental fact forms the basis of personal caries prevention and good dental health education.
Sites of caries
The parts of a tooth most prone to caries are those where food tends to collect and plaque bacteria can flourish. Such sites are known as stagnation areas. Occlusal fissures and the spaces between the mesial and distal surfaces of adjoining teeth (the interproximal areas, or contact points) are the most common stagnation areas. That is why caries occurs most often on occlusal and proximal surfaces. However, anywhere food debris can accumulate is a stagnation area where plaque will proliferate and caries is likely to occur. Such food traps are the necks of teeth covered by ill-fitting partial dentures, irregular teeth and unopposed teeth.
Minimal harm is caused by partial dentures which fit perfectly, but those which do not are a menace to dental health. They leave spaces between the necks of the teeth and the acrylic plate, or between any metal clasps and the teeth, which are dangerous stagnation areas.
During mastication, the movement of saliva and the food bolus over the tooth surfaces as it is chewed actually helps to clean teeth which are in good occlusion. This does not prevent plaque formation, but does reduce the amount of retained food debris which is responsible for the harmful effects of plaque. Teeth which are not in good occlusion, such as irregularly positioned and unopposed teeth, are not so exposed to this beneficial cleansing effect. Consequently food collects around these instanding or outstanding irregular teeth. It also covers the crown of any tooth which has lost its opposite number, and remains unopposed because the space has not been replaced artificially. To make the situation even worse, the sticky sweet food most likely to produce caries needs the minimum amount of mastication anyway, and therefore has a negligible cleansing effect – even on teeth in good occlusion.
Caries and cavity formation
Unrestricted consumption of carbohydrates and their sugar content produces an abundance of acid-forming bacteria in the plaque which collects in stagnation areas. The resultant series of continual acid attacks prevents remineralisation and allows acid to eat through the enamel until it reaches dentine, whereupon the caries spreads more rapidly through the more open structure of this inner tooth layer (Figure 11.1).
Microscopically, the process of cavity formation is as follows.
- Very early acid attacks will show as ‘white spot lesions’ on the enamel surface.
- Continued and frequent acid attacks will follow the prism structure of the enamel, and eat into any exposed cementum on the tooth root.
- Demineralisation occurs, followed by episodes of remineralisation if the acid attacks are not too frequent – these areas of repair often appear as brown lesions on the teeth, especially at contact points (Figure 11.2).
- With frequent or prolonged acid attacks, the mineral structure of the enamel is eventually destroyed and caries enters the tooth.
- Caries extends deep into the enamel and eventually reaches the amelodentinal junction (ADJ).
- Up to this point, the patient will feel no pain as enamel contains no nerve tissue.
- Once past the ADJ, the caries enters dentine and can spread more rapidly because of the hollow structure of this tooth layer and its lower mineral content compared to enamel.
- This undermines the overlying enamel, and normal occlusal forces are able to fracture off pieces of the tooth surface, leaving a hole in the tooth structure – this is called a cavity (Figure 11.3).
- Odontoblast cells at the ADJ react to the bacterial attack by laying down secondary dentine in an attempt to protect the underlying pulp tissue.
- The nerve fibrils lying within the dentine tubules will be stimulated as the caries progresses, and the patient will begin to feel sensitivity to temperature changes and to sweet foods.
- The pulp tissue will also become irritated and inflamed – this is called pulpitis.
- At this point, the caries can be removed by the dentist and the cavity restored with a filling (see Chapter 15), the inflamed pulp will settle and the tooth will be restored to its normal function – the inflammation is better described then as reversible pulpitis.
- Otherwise, the cavity will continue to enlarge and the caries will progress towards the pulp chamber, as the production of secondary dentine is overrun by the speed of the bacterial attack.
- The patient will be experiencing more severe pain of longer duration, and will eventually be unable to bite with the affected tooth.
- When the carious attack reaches the immediate surroundings of the pulp chamber, the level of inflammation is too great to be resolved simply by removing the caries – this is called irreversible pulpitis.
- The pain will become constant and throbbing in nature, often disturbing the patient’s sleep.
- Once the pulp chamber itself is breached by the caries, a carious exposure of the contents occurs and the pulp will eventually die.
- The tooth can now only be treated by undergoing an endodontic procedure (see Chapter 15) or by extraction (see Chapter 17).
Figure 11.1 Cavity formation.
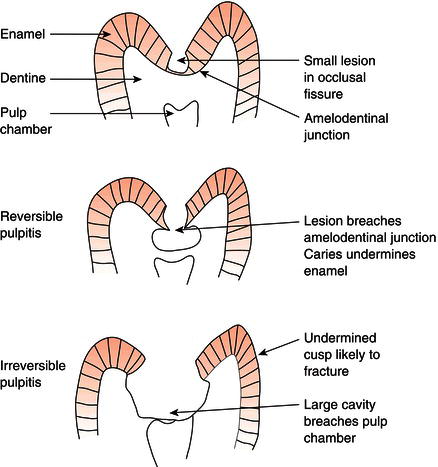
Figure 11.2 Brown spot lesion.

Figure 11.3 Cavity.

Irreversible pulpitis
Pulpitis occurs when caries extends through the dentine to reach the pulp. The pulp is then said to be cariously exposed and the sequence of events described under inflammation (see Chapter 7) follows.
- There is an increased blood flow through the apical foramen into the pulp.
- Swelling cannot occur, however, as the pulp is confined within the rigid walls of the root canal and pulp chamber.
- Pressure therefore builds up instead and causes intense pain.
- A much more important result of this pressure, however, is the compression of blood vessels passing through the tiny apical foramen – this cuts off the blood supply and causes death of the pulp.
- When the pulp dies, its nerves die too, and the severe toothache stops abruptly.
- The respite is short, however, as pulp death leads to another very painful condition called alveolar abscess.
Pulpitis may be acute or chronic. It has many causes, apart from caries, but almost always ends in pulp death. Other causes of pulpitis are covered in Chapter 15.
Alveolar abscess
When pulpitis occurs, the pulp eventually dies as its blood supply is cut off by inflammatory pressure. The dead pulp decomposes and infected material passes out of the tooth through the apical foramen and into the alveolar bone at the apex of the tooth. These irritant products give rise to another inflammatory reaction in the tissues surrounding the apex. Pus formation occurs and an acute alveolar abscess develops.
- This is an extremely painful condition.
- The affected tooth becomes loose and very tender to the slightest pressure.
- There is a continual throbbing pain and the surrounding gum is red and swollen.
- Frequently the whole side of the face is involved in inflammatory swelling and the patient may have a raised temperature.
- Looseness is caused by swelling of the periodontal ligament.
- Pain is caused by the increased pressure of blood within the rigid confines of the periodontal ligament and alveolar bone. The tooth is so tender that it cannot be used for eating.
- Thus an acute alveolar abscess may show all the cardinal signs of acute inflammation:
- pain
- swelling
- redness
- heat
- loss of function
- raised body temperature.
Pulp death is sometimes followed by the development of a chronic alveolar abscess instead of an acute one. This usually gives rise to very little pain and most patients are quite unaware of its presence. It may often be detected by the presence of a small hole in the gum called a sinus, which is a track leading from the abscess cavity in the alveolar bone to the surface of the gum. Pus drains from the abscess through the sinus into the mouth. This outlet prevents a build-up of pressure inside the bone and explains the lack of pain. Patients often refer to this lesion as a ‘gum boil’.
If an acute abscess is not treated, it eventually turns into a chronic abscess by the drainage of pus through a sinus (see Figure 7.3). This relieves the pain and the features of acute inflammation largely disappear. The relative freedom from pain does not last indefinitely, however, as a chronic alveolar abscess is liable to revert into an acute abscess at any time.
It should now be clear that pulpitis is followed by pulp death, and this eventually leads to an acute alveolar abscess, either directly or via a chronic abscess.
It was formerly taught that all carious dentine should be removed, but this is now considered unnecessary. Adequate preparation, filling and sealing of a cavity cuts it off from further plaque and acid formation, and allows a vital pulp to remineralise the deeper underlying dentine. Removal of carious dentine should therefore stop short of exposing the pulp when possible.
Role of saliva in oral health
The oral soft tissues in health are constantly bathed in saliva, the watery secretion from the three pairs of major salivary glands as well as from the numerous minor salivary glands present in the cheeks and lips (see Chapter 10).
Saliva contains the following components.
- Water, as a transport agent for all the other constituents.
- Inorganic ions and minerals, such as calcium ions and phosphate.
- Ptyalin, a digestive enzyme which acts on carbohydrates (also called salivary amylase).
- Antibodies, as part of the defensive immune system, and known as immunoglobulins.
- Leucocytes or white blood cells, also part of the body’s defence system.
These constituents all have important functions in the maintenance of a healthy oral environment.
- The inorganic ions and minerals are released as required to act as buffering agents to help control the pH of the oral environment, by neutralising the organic acids produced by bacteria.
- A high inorganic ion/mineral content produces thick, stringy saliva which gives the teeth good protection against caries, but allows dental calculus (tartar) to form easily and in large amounts.
- A low inorganic ion/mineral content produces watery saliva, which offers little protection against caries to the teeth, but prevents large amounts of calculus from forming.
- Calculus formation is associated with periodontal disease.
- Water forms the carrying agent for the other salivary constituents, and allows self-cleansing of the oral environment to occur by dislodging food debris from the teeth before being swallowed.
- The water also moistens the food bolus and the soft tissues, allowing swallowing (deglutition) and speech to occur.
- It also dissolves food particles, so that the sensation of taste is produced – the taste buds on the tongue can only detect the taste of food when it is in solution.
- Both antibodies and leucocytes help to protect and defend the oral environment from infection by micro-organisms.
Reduced salivary flow
The condition of reduced salivary flow is called xerostomia or dry mouth. There are many reasons why a patient can suffer from this, apart from it being the result of normal age-related changes of the salivary glands themselves.
- Normal age-related changes to the salivary glands and their ability to function.
- Low fluid intake over a period of time, or even dehydration.
- Some autoimmune disorders, especially Sjögren’s syndrome which specifically affects the salivary glands and the lacrimal glands of the eyes, which produce tears.
- Several routinely prescribed drugs, including diuretics (prescribed to alleviate water retention in patients with heart failure), some antidepressants (prescribed to alleviate anxiety), and beta-blockers (prescribed to slow down the heart rate, especially in angina sufferers).
Reduced salivary flow has several important consequences for the patient and for the oral health team.
- Reduced self-cleansing allows more food debris to accumulate around the teeth, increasing plaque production and the likelihood of caries and periodontal disease developing.
- It will also allow food debris to stagnate in the mouth, causing halitosis (bad breath).
- Reduced buffering of the oral environment allows longer and more frequent acid attacks, increasing the likelihood of caries developing.
- Poor lubrication of the oral soft tissues makes speech and swallowing more difficult.
- Reduced amounts of water in the saliva affects the sensation of taste.
- Reduced flow and amounts of saliva in the mouth will make the retention of dentures more difficult.
The opposite condition to xerostomia, that of excessive saliva production, is called ptyalism, which is often seen in patients with periodontal disease. It can also occur in Parkinson’s disease and in pregnancy.
Diagnosis of caries
Before caries is treated, it must first be detected. Early diagnosis is very important in controlling the extent of the damage done, as well as the level of discomfort experienced by the patient. The earlier a cavity is detected, the better the chance of saving the tooth. This is why regular dental examinations are recommended, and the frequency of attendance should be determined by the caries experience of the patient – those with a high caries incidence need to be examined more frequently than others. Unfortunately, these are often the very patients who do not attend regularly for dental examination, for whatever reason.
Large cavities are obvious to the naked eye but it is easier to treat caries before cavities reach such a size. The dentist has various methods available for detecting smaller carious les/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


