Basic Injection Techniques
1. Describe the four anesthetic administration techniques.
2. Describe patient preparation and rapport strategies inherent in stress reduction protocol used for all anesthetic procedures.
3. Describe the steps to providing a successful injection and the importance of each.
4. Successfully complete review questions and activities for this chapter.
Administration Techniques
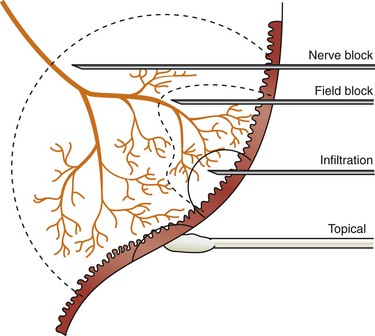
When choosing the appropriate administration technique, the dental hygienist must consider the area to be treated, the duration of anesthesia needed, and the comfort needs of the patient. Local anesthesia administration techniques are divided into four major categories: surface anesthesia, local infiltration, field block, and nerve block (Figure 11-1).
Surface Anesthesia
Surface anesthesia is used when topical anesthetics are applied to the surface by gels, creams, or sprays to block the free nerve endings supplying the mucosal surfaces. The effect is short lasting and limited to the direct area of contact. Topical anesthetics are used as a preinjection technique to obtund the pain associated with needle insertion.1
Local Infiltration
Local infiltration techniques are used when soft tissue anesthesia is needed in a limited area. The anesthesia is deposited close to the smaller terminal nerve endings providing pain relief only in the area of anesthetic diffusion. Dental hygienists can use this technique during nonsurgical periodontal therapy when anesthesia is needed only in the immediate area of injection, and for bleeding control provided by the vasoconstrictor.1,2
Field Block
Field block is a form of regional anesthesia deposited near large terminal nerve branches. It is also referred to as supraperiosteal injections. Anesthesia usually involves pulpal and soft tissue anesthesia of a single tooth in the maxilla (by depositing the solution above the apex of the tooth to be anesthetized) except in the area of the anterior superior alveolar block (ASA) and middle superior alveolar block (MSA) where anesthesia is achieved on more than one tooth using this technique (see Chapter 12). Field block injections are most effective in the maxillary arch due to the porous nature of the bone allowing the anesthetic to easily diffuse through the bone to the nerve. However, this technique can be used on the mandibular laterals and incisors, and is an excellent injection technique when crossover anesthesia is needed (see Chapters 12 and 13). In dentistry, field block injections are often referred to incorrectly as infiltration injections.
Nerve Block
Nerve block anesthesia refers to the injection of local anesthetic in the vicinity of a major nerve trunk to anesthetize the nerve’s area of innervations, usually at a greater distance from the area of treatment. This technique offers an advantage over the other techniques by providing profound pulpal and soft tissue anesthesia over a larger area. The disadvantage is that arteries and veins accompany major nerve trunks, and the potential for piercing the artery or vein with this technique is greatly enhanced.1 Examples of nerve blocks are the inferior alveolar, posterior superior alveolar, mental/incisive, and infraorbital blocks.
Steps To Providing A Successful Injection
The administration of local anesthetics will become routine to the experienced dental hygienist, but it is often a very stressful experience for the patient. For many patients, the fear and anticipation of pain from receiving a “shot” could produce an emergency situation.3–5 Vasodepressor syncope is the most common medical emergency observed in the dental office, and it is most frequently linked to the administration of local anesthesia.3–5
Step 1: Preanesthetic Patient Assessment And Consultation
The patient assessment should be conducted as described in Chapter 7, and vital signs should be obtained and recorded. Appropriate medical and dental consultations should be completed before administration of local anesthetics.
Selection of Anesthetic
The physical status of the patient: The choice of local anesthetic agent and vasoconstrictor must be based on the patient’s physical status. Absolute and relative contraindications should be carefully evaluated, and an anesthetic agent with the least adverse effects according to the patient’s physical status should be selected.
Duration of treatment and postoperative pain control: Duration of effect in pulpal and soft tissue varies for each agent, and consideration should be made as to whether profound pulpal anesthesia is indicated. For nonsurgical periodontal therapy in shallow pockets with soft tissue sensitivity but no root sensitivity, a short-acting anesthetic such as 3% mepivacaine may be appropriate. For half-mouth nonsurgical periodontal therapy with deep pockets and heavy deposits, a longer-acting anesthetic may be appropriate.
Volume of anesthetic: Profound pulpal anesthesia necessary for restorative procedures, extractions, and nonsurgical periodontal therapy with heavy deposits, for example, is essential and will require more anesthetic volume than less invasive procedures.
Need for hemostasis: Limited visibility decreases the efficiency in providing thorough deposit removal. If heavy bleeding is anticipated, a vasoconstrictor should be selected to constrict the blood vessels for greater visibility. Caution should be taken when using epinephrine 1 : 50,000 in patients with significant cardiovascular disease. For excessive bleeding, it is recommended to infiltrate epinephrine 1 : 50,000 in small amounts directly into the area of bleeding for greatest visibility and hemostatic control.
Possibility of self-mutilation: Small children and patients with special needs are more prone to bite themselves while numb, causing self-mutilation. Longer acting anesthetics should be avoided.
Determining maximum recommended dose: The patient’s maximum recommended dose (MRD) should be calculated based on the selected anesthetic and the patient’s medical history and documented in the patient’s chart (see Chapter 8).
Step 2: Confirm Care Plan
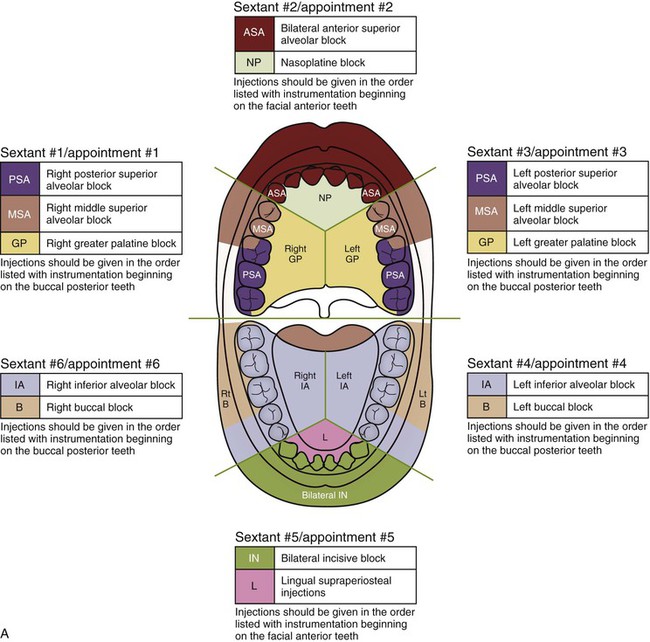
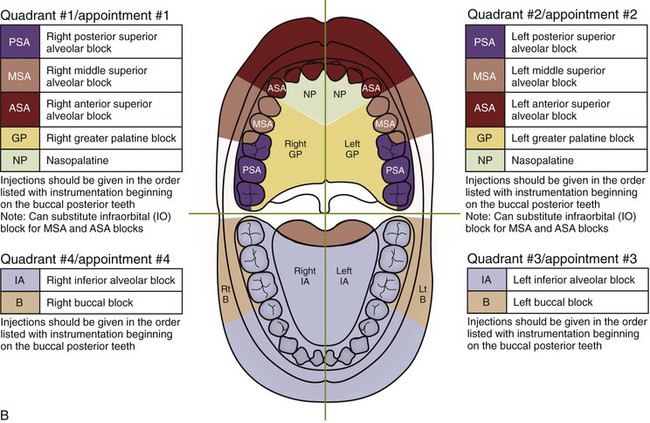
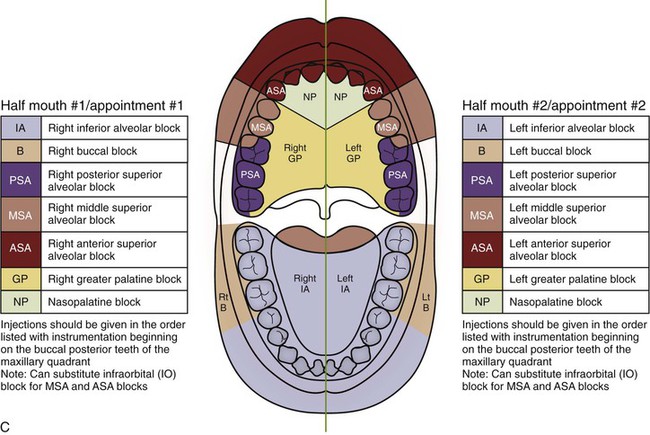
Depending on the time available for treatment and the extent of periodontal involvement, the dental hygienist should design a care plan by dividing the mouth into quadrants or sextants for treatment. Figure 11-2 illustrates examples of nonsurgical periodontal therapy with anesthesia care plan designs. With advanced periodontal disease and heavy deposits the dental hygienist may only realistically be able to complete a few teeth in a single visit. The dental hygienist should then divide the mouth into sextants rather than quadrants for treatment. (see Figures 11-2A,B) If either sextant or quadrant dental hygiene treatment is planned on the maxillary arch, the posterior superior alveolar (PSA) block is given before any of the other maxillary facial injections as well as any maxillary palatal injections to allow the necessary time for the larger molars to become completely anesthetized, with instrumenting proceeding in the same manner. After the PSA block, the middle superior alvolar (MSA) and then the anterior superior alveolar (ASA) block (or infraorbital [IO] block instead) is then given (in that order). For patients with initial to moderate periodontal disease, the dental hygienist may complete one to two quadrants during a single visit. When two quadrants are treated in a single visit, it is recommended to treat upper and lower quadrants on either the right or left side of the patient’s face. (Figure 11-2C) The dental hygienist should avoid administering local anesthetics to both the mandibular right and left quadrants during a single treatment to prevent the inability of the patient to control his or her mandible. Administering bilateral inferior alveolar nerve blocks also increases the possibility of the patient causing self-mutilation of their soft tissues (see Chapter 14). If half-mouth treatment is planned, the inferior alveolar and buccal blocks are given first, then the maxillary facial, and then palatal injections follow in order as described earlier, with instrumenting proceeding first on the maxillary arch. This allows time for the entire mandibular arch to become completely anesthetized. When designing the dental hygiene care plan, the dental hygienist must consider the amount of anesthetic needed to complete the procedure (always staying within the patient’s MRD).
Step 3: Informed Consent
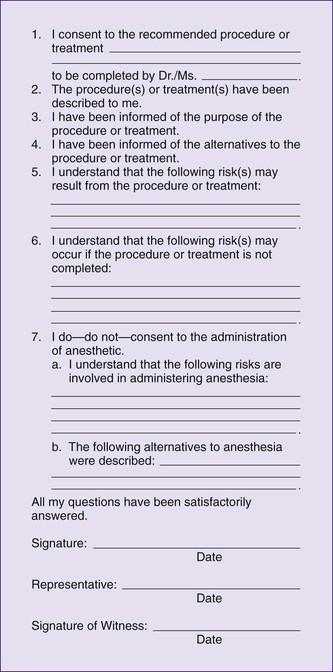
The benefits and risks associated with all treatment including the administration of local anesthetics should be discussed, as should the risks involved in not receiving treatment. The dental hygienist should discuss with the patient the type of anesthetic that will be used, and the injection procedure. The patient should be advised of the temporary numbing feeling associated with the administration of the drug, and the anticipated duration of anesthesia. Following the care plan discussion, informed consent to treatment should be received by the patient. In the case of a minor, the informed consent must be given by the parent or guardian. Figure 11-3 is a sample informed consent form that includes the consent to the administration of anesthetics. The written agreement of the care plan becomes a legal contract between the patient and the dental hygienist.2
Step 4: Selection Of Injection
Areas needing to be anesthetized: For maximum patient comfort, the dental hygienist should select injections to completely anesthetize the areas needed with minimal tissue penetrations, such as choosing nerve blocks rather than field blocks for larger treatment areas. In addition, the dental hygienist should take into consideration the density of the bone in the area of treatment and the selection of injection technique. Supraperiosteal injections are much more effective on the maxilla because the bone is callous. The mandible requires nerve blocks because the cortical plate is thick. The mandibular anterior teeth are more conducive to supraperiosteal injections but to a lesser degree than the maxilla.
Presence of infection: Infection in the area of anesthetic administration will decrease the effectiveness of the anesthetic. The acidic nature of the anesthetic deposited into acidic tissue from the infection decreases the ability of the anesthetic to readily dissociate for nerve penetration. (See Chapter 3.) It is recommended to administer nerve blocks away from the infected area.
Hemostasis: If hemostasis is needed in the area for greater visibility, it is recommended to infiltrate small amounts of anesthetic with a vasoconstrictor directly into the papillary, interdental or marginal gingival. Epinephrine 1 : 50,000 produces the greatest hemostatic control.
Step 5: Preparation Of Equipment
The preparation of equipment should be completed as described in Chapter 9. The appropriate selection of a syringe is important, taking into consideration the hand size of the dental hygienist and the hygienist’s ability to properly conduct the aspiration test (Figure 11-4). The bulkiness of the anesthetic syringe and the length of dental anesthetic needles can be frightening to the patient; therefore, they should be covered or placed out of the patient’s sight (Figure 11-5). The equipment may be set up before the patient’s arrival if the care plan and selection of appropriate anesthetic has already been determined at a previous appointment. However, any recent changes in the patient’s medical history may require a modification in anesthetic selection.

Step 6: Check The Anesthetic Equipment
Before administration of the local anesthetic, the dental hygienist should check the needle bevel orientation for planned injections in close proximity to the periosteum. The bevel should be oriented toward the bone. For these injections, the bevel indicator (Figure 9-21) should be turned opposite the large window. This will ensure that when the dental hygienist is holding the syringe palm up with the large window facing him or her, the bevel will be toward the bone when the injection is commenced. Although the bevel of the needle does not affect success rates of the injection, it will provide added comfort to the patient and less trauma to the periosteum if the bone is contacted.
Step 7: Patient Position
Supine positioning (head and heart parallel to the floor) (Figure 11-6) with the patient’s feet slightly elevated is the most effective position to administer anesthesia. Because supine positioning is the recommended position to treat vasodepressor syncope, this adds the benefit of decreasing the risk of a patient fainting before, during, or after the administration of the anesthetic.3,4 The dental hygienist should ask the patient to turn his or her head appropriately for the greatest visibilty of the penetration site.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses