Local Anesthetic Agents
1. Define ester and amide local anesthetics.
2. List and describe the composition of local anesthetic solutions.
3. Discuss the properties and ionization factors of local anesthetics.
4. Discuss the biotransformation of each local anesthetic currently used in dentistry and how esters differ from amides.
5. List and discuss all ester and amide local anesthetics using their generic and proprietary names.
6. List the ester and amide local anesthetics and their formulations.
7. Discuss the selection considerations when choosing a local anesthetic.
8. Describe the factors that determine the duration of a local anesthetic.
9. Correctly complete the review questions and activities for this Chapter.
Composition Of Local Anesthetic Solutions
Local anesthetics used in dentistry are manufactured in single-use cartridges, also referred to as carpules. Local anesthetic cartridges are designed to contain 2.0 mL of solution. However, when the silicone rubber stopper is added to the cartridge, it is capable of containing 1.8 mL of solution. Although most local anesthetic cartridges contain 1.8 mL of solution, not all are labeled as such. Some manufacturers label and market their anesthetics as containing 1.7 mL of solution. (See Box 5-1.) Local anesthetics are formulated in 2% solutions (36 mg per cartridge), 3% solutions (54 mg per cartridge), 4% solutions (72 mg per cartridge), and 0.5% solutions (9 mg per cartridge). (See Chapter 8 for dosaging facts and calculations.) In addition to the local anesthetic drug, the dental cartridge may contain several other ingredients such as:
• Vasoconstrictor: As discussed in Chapter 4, there are two vasoconstrictors currently added to local anesthetic solutions in the United States : epinephrine and levonordefrin. Epinephrine is available in 1 : 50,000, 1 : 100,000, and 1 : 200,000 dilutions, and levonordefrin is available in a 1 : 20,000 dilution and only with mepivacaine 2%. All local anesthetics are vasodilators, and vasoconstrictors are added to local anesthetic solutions to delay the absorption of local anesthetics, which reduces the potential for systemic toxicity and prolongs the duration of action. Because vasoconstrictors counteract the vasodilatory properties of local anesthetics, they are also beneficial for providing hemostasis.
• Vasoconstrictor preservative: Sodium bisulfite, metabisulfite, or acetone sodium bisulfite is only added to local anesthetic solutions that contain vasoconstrictors.1 Since vasoconstrictors are unstable and have a short shelf life, sodium bisulfite is added to delay the deterioration of the vasoconstrictor. Sodium bisulfite is manufactured as an acid salt rendering it soluble in water and decreasing the pH of the solution, making it significantly more acidic than the same solution without a vasoconstrictor. As discussed in Chapter 3, local anesthetic solutions that are more acidic have a greater quantity of charged cation molecules (RNH+) than the uncharged base (anion) molecules (RH). This slows the efficiency of the local anesthetic solution to diffuse into the axoplasm, delaying the onset of action.
• Sodium hydroxide: Sodium hydroxide is a buffer that alkalinizes, or adjusts, the pH of the solution between 6 and 7.2
• Sodium chloride: Sodium chloride is a buffer which when added to a local anesthetic creates an injectable isotonic solution.
Selection Of Local Anesthetic Agents
There are two main classifications of local anesthetic agents: esters and amides. Esters are metabolized in the plasma by plasma cholinesterase, and most amides are metabolized in the liver, the exception being articaine which is metabolized in the blood similar to esters. Because there is a greater propensity of patients who are hypersensitive to injectable esters, all injectable local anesthetics manufactured for dentistry today are in the amide group. As discussed in Chapter 3, the intermediate hydrocarbon chain of the anesthetic molecule determines whether the anesthetic is classified as an ester or an amide. There are five generic classifications of amide local anesthetics available in North America for use in dentistry. Table 5-1 lists some generic and proprietary names. These amide local anesthetic preparations come in various concentrations, with or without vasoconstrictors. The preparations are as follows:
TABLE 5-1
| GENERIC NAME | PROPRIETARY NAME |
| Lidocaine | Xylocaine, Alphacaine, Octocaine |
| Mepivacaine | Carbocaine, Arestocaine, Isocaine, Polocaine, Scandonest |
| Prilocaine | Citanest |
| Articaine | Septocaine, Zorcaine, Articadent |
| Bupivacaine | Marcaine |
Modified from Darby M, Walsh M: Dental hygiene theory and practice, ed 3, St Louis, 2010, Saunders.
• Lidocaine: 2% Plain; 2% 1 : 50,000 epinephrine; 2% 1 : 100,000 epinephrine
• Mepivacaine: 3% Plain; 2% 1 : 20,000 levonordefrin
• Prilocaine: 4% Plain; 4% 1 : 200,000 epinephrine
• Articaine: 4% 1 : 100,000 epinephrine; 4% 1 : 200,000 epinephrine
• The duration of pain control based upon the length of the procedure
• The need for post-treatment pain control
• The patient’s health assessment, and current patient medications
• A local anesthetic, sodium bisulfite, or metabisulfite allergy
Duration of Action and Operative Pain Control
As discussed in Chapter 3, there are several physical properties that determine the local anesthetic’s onset and duration of action. Table 5-2 lists the properties for the local anesthetic agents that are currently available. The drug’s pKa determines the anesthetic’s distribution of cations and anions. The lower the pKa, the more anions are present in base form for better penetration through the lipid rich nerve, which provides a more rapid onset of action. The protein-binding capacity and the lipid solubility of the anesthetic are related to its duration of action. The lipid solubility also determines the anesthetic’s potency. Bupivacaine has the highest percentage of protein binding and is the most lipid-soluble of all the local anesthetics; it therefore has the longest duration and is the most potent. However, bupivacaine has the highest pKa and therefore the slowest onset of action. The vasodilating properties of anesthetics also play a significant role in both the potency and duration of action. Mepivacaine and prilocaine have the least vasodilating effects, allowing the anesthetic to remain in the area of disposition longer, especially following a nerve block3,4 (Table 5-3). For this reason, both anesthetics are quite effective without a vasoconstrictor, and both are good alternatives when a vasoconstrictor is contraindicated.
TABLE 5-2
Physical Properties of Local Anesthetics
| LOCAL ANESTHETIC | PKA* | VASODILATING† | T  ‡ ‡ |
LIPID SOLUBILITY§ | PROTEIN BINDING‖ (5%) |
| Lidocaine | 7.7 | 1 | 1.6 | 2.9 | 65 |
| Mepivacaine | 7.7 | 0.8 | 1.9¶ | 0.8 | 75 |
| Prilocaine | 7.7 | 0.5 | 1.6 | 0.9 | 55 |
| Bupivacaine | 8.1 | 2.5 | 3.5 | 27.5 | 95 |
| Articaine | 7.8 | 1¶ | .75 | 1.5 | 54 |
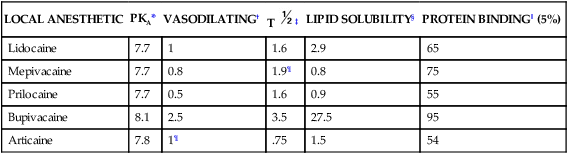
*pKa, Dissociation constant; rate of onset.
†Vasodilating lidocaine given value of 1.
§Lipid solubility oil/water solubility; intrinsic potency, increased penetrability.
‖Protein binding duration of action
Modified from Haveles B: Applied pharmacology for the dental hygienist, ed 6, St Louis, 2011, Mosby.
TABLE 5-3
Duration of Pulpal Anesthesia of Local Anesthetics Without Vasoconstrictors by Injection Type
| LOCAL ANESTHETIC | INFILTRATION (DURATION IN MINUTES) | NERVE BLOCK (DURATION IN MINUTES) |
| Lidocaine 2% | 5–10 | 10–20 |
| Mepivacaine 3% | 20 | 40 |
| Prilocaine 4% | 10–15 | 40–60 |
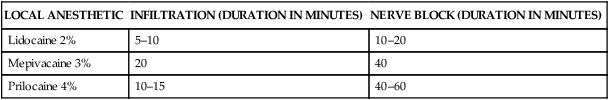
From Malamed SF: Handbook of local anesthesia, ed 5, St Louis, 2004, Mosby.
1. Short-acting anesthetics provide pulpal anesthesia of approximately 30 minutes and do not contain a vasoconstrictor. These include:
2. Intermediate-acting anesthetics provide pulpal anesthesia of approximately 60 minutes and contain a vasoconstrictor, except for prilocaine 4% when administered as a nerve block. These include:
• Lidocaine 2%; 1 : 50,000 epinephrine
• Lidocaine 2%; 1 : 100,000 epinephrine
• Mepivacaine 2%; 1 : 20,000 levonordefrin
• Prilocaine 4% (intermediate only when administering a nerve block, may provide 60 minutes of pulpal anesthesia in some patients)
• Prilocaine 4%; 1 : 200,000 epinephrine
3. Long-acting anesthetics provide pulpal anesthesia of approximately 90 minutes or more and contain a vasoconstrictor. Bupivacaine is the only long-acting anesthetic available in the United States.
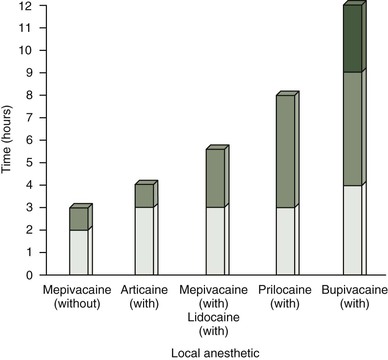
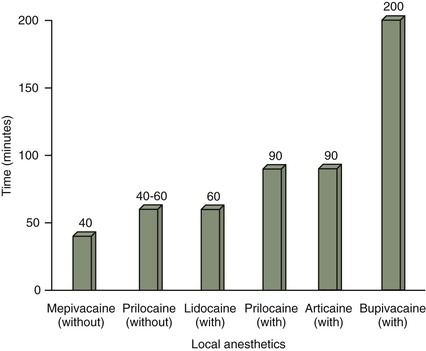
Table 5-4 lists the local anesthetics by their duration of action categorized by short, intermediate, and long acting, and both pulpal and soft tissue anesthesia. Figure 5-1 illustrates the duration of action for soft tissue anesthesia following the administration of a nerve block, and Figure 5-2 illustrates the duration of action for pulpal anesthesia following the administration of a nerve block.
TABLE 5-4
| GENERAL CATEGORIES | ||
| SHORT DURATION (PULPAL = APPROXIMATELY 30 MIN) | INTERMEDIATE DURATION (PULPAL APPROXIMATELY 60 MIN) | LONG DURATION (PULPAL >90 MIN) |
| Lidocaine 2% plain | Lidocaine 2% 1 : 50,000 or 1 : 100,000 epinephrine | Bupivacaine 0.5% 1 : 200,000 epinephrine |
| Mepivacaine 3% plain (infiltration/nerve block)* | Mepivacaine 2% 1 : 20,000 levonordefrin | |
| Prilocaine 4% plain (infiltration)*† | Prilocaine plain (nerve block)*† | |
| Prilocaine 4% 1 : 200,000 epinephrine‡ | ||
| Articaine 4% 1 : 100,000 epinephrine‡ | ||
| Articaine 4% 1 : 200,000 epinephrine | ||
| PULPAL AND SOFT TISSUE ANESTHESIA | ||
| LOCAL ANESTHETICS | PULPAL (MIN) | SOFT TISSUE (MIN) |
| Lidocaine 2% plain | 5–10 | 60–120 |
| Lidocaine 2% 1 : 50,000 or 1 : 100,000 epinephrine | 60 | 180–300 |
| Mepivacaine 3% plain (infiltration/block)* | 20 (infiltration) 40 (nerve block) |
120–180 |
| Mepivacaine 2% 1 : 20,000 levonordefrin | 60 | 180–300 |
| Prilocaine 4% plain (infiltration/block)*† | 10–15 (infiltration) 40–60 (nerve block) |
90–120 120–240 |
| Prilocaine 4% 1 : 200,000 epinephrine† | 60–90 | 180–480 |
| Articaine 4% 1 : 100,000 epinephrine† | 60–75 | 180–360 |
| Articaine 4% 1 : 200,000 epinephrine | 45–60 | 120–300 |
| Bupivacaine 0.5% 1 : 200,000 epinephrine | 90–180 | 240–540 |
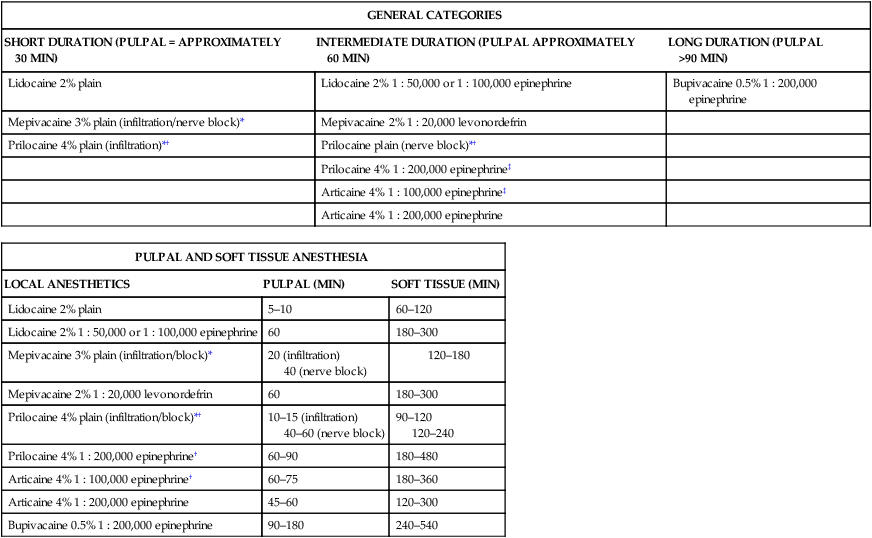
*Mepivacaine plain is a short-acting anesthetic when administered by infiltration or nerve blocks, but the duration is increased with a nerve block.
*†Prilocaine plain administered as an infiltration is a short acting anesthetic. When administered as a nerve block it increases its duration to an intermediate action.
‡4% Prilocaine 1 : 200,000 and 4% articaine 1 : 100,000 are categorized as intermediate durations, but provides a slightly longer duration than the other intermediate drugs, extending the duration to 60–90 minutes.
Modified from Haveles B: Applied pharmacology for the dental hygienist, ed 6, St Louis, 2011, Mosby.
• Individual response to anesthetic. In general, individuals respond as expected to the onset and duration of action as listed in Table 5-4. However, some individuals are less or more sensitive to the administered anesthetic and expected duration is either decreased or increased, accordingly. Malamed4 states that there are three types of individual responses to the administration of local anesthetics, normal responders, hyper-responders, and hypo-responders. These categories are utilized to determine the duration of action of a local anesthetic. Using lidocaine 2% with epinephrine 1 : 100,000 as an example, approximately 70% of patients would fall in the normal responder category, representing a typical duration of 60 minutes of pulpal anesthesia. Hyper-responders represent approximately 15% of individuals who overly-respond to local anesthetics, and may have pulpal anesthesia of approximately 70 to 80 minutes or longer. Hypo-responders represent the final 15% of individuals who under-respond to local anesthetics and may have pulpal anesthesia of approximately 45 minutes or less. Individual patient responses should be anticipated from time to time. Once it is determined that a patient does not respond to the anesthetic drug as expected, a notation should be made in the patient’s chart to signal the practitioner of the variation in the patient’s response to the anesthetic and to document any modifications that were made to achieve appropriate duration of anesthesia (Box 5-2).
• Accuracy of anesthetic administration. Accuracy of anesthetic administration is most difficult when administering a nerve block, an injection of local anesthetic in the vicinity of a nerve trunk to anesthetize the nerve’s area of innervations, such as with the inferior alveola (IA) block; it is least difficult when administering supraperiosteal injections, an injection that anesthetizes a small area by depositing anesthetic near the terminal nerve endings. To successfully achieve profound anesthesia of the IA block, the anesthetic solution should be deposited as close to the nerve trunk as possible. Because of the depth of penetration required for IA block, it is necessary to advance the needle through significant soft tissue, allowing a greater possibility for needle deflection, which can influence the accuracy of the injection.
• Vascularity of tissue. In healthy tissues, the onset of action and the duration of the anesthetic are more predictable. However, inflamed tissue has increased vascularity due to infection, slowing the onset of action and decreasing the duration because of rapid absorption.
• Variation of anatomic structure. Anatomic variations are difficult to predict and often decrease the duration of local anesthetic action. Decreased anesthetic duration and effectiveness in the maxillae may be caused by5:
• Density of bone. The density of the alveolar bone of the maxillae is typically less than the alveolar bone of the mandible, providing easy anesthetic diffusion and increased duration of pain control. Extra dense bone in this area decreases the success and duration of pain control.
• Flaring of palatal roots of maxillary molars may affect the anesthetic’s action.
• A lower than normal zygomatic arch, commonly seen in children, may prevent or decrease the duration of the anesthetic’s action in the maxillary molars.
Decreased anesthetic duration and effectiveness in the mandible may include the following5:
Posttreatment Pain Control
For effective pain management, the selection of an appropriate anesthetic agent for a dental procedure should take into consideration posttreatment pain control. For half mouth (two quadrants) nonsurgical periodontal therapy, profound anesthesia and a longer appointment time may be necessary. Although nonsurgical periodontal therapy usually does not require posttreatment pain control, long duration agents may be needed on occasion for some individuals if posttreatment discomfort is anticipated.5 Most dental procedures performed by the dentist and dental hygienist fall within the intermediate range of pain control. Examples of procedures that may require postoperative pain control may include, but are not limited to, extractions (impacted third molars) and periodontal surgeries. If the dental hygienist is administering anesthesia for a non–dental hygiene procedure, consultation with the dentist before selecting the local anesthetic is appropriate. Anesthetics that provide longer posttreatment durations of pulpal and soft tissue anesthesia are 0.5% bupivacaine 1 : 200,000 epinephrine (long acting), and 4% prilocaine 1 : 200,000 epinephrine (which can provide intermediate to long) (see Table 5-4). Longer acting local anesthetic agents should be avoided for children and individuals with special needs to prevent the possibility of self-mutilation by accidentally biting or chewing on the lip or tongue.
Patient Health Assessment and Current Patient Medications
Local anesthetics used in dentistry today are reliable, and when administered correctly produce effective pain control with little toxicity.6 However, certain medical conditions, such as cardiovascular disease, liver disease, hyperthyroidism, brittle diabetes, allergies, etc. and drug interactions, such as tricyclic antidepressants, cimetidine, beta blockers, etc. may influence the type and volume of anesthetic or vasoconstrictor that the patient may safely receive. The patient’s medical history must be thoroughly evaluated and discussed at each dental hygiene appointment to determine if a relative or absolute contraindication exists for the local anesthetic agent or vasoconstrictor. A relative contraindication means that the administration of the offending drug may be used judiciously, and an absolute contraindication means the offending drug should not be administered to the individual under any circumstances. Once the dental hygienist determines if any contraindications exist utilizing consultations as needed, the maximum recommended dose (MRD) for the individual patient can be determined. The maximum reco/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses