Chapter 11 Applied Anatomy
Applied Anatomy
1 Anatomy of Local Anesthesia
TYPES OF LOCAL ANESTHESIA
The two basic types of local anesthetic injections are local infiltration and nerve block.
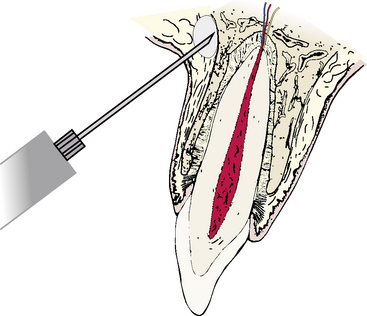
Local Infiltration
Small areas of soft tissue or bone may be anesthetized by injecting a small amount of anesthetic fluid directly into the area (Figure 11-1). The fluid diffuses through a small, localized area and blocks the terminal nerve fibers there. Most maxillary teeth may be anesthetized in this manner. Anesthetic fluid is injected deep to the vestibular fold and deposited on the periosteum of the alveolar bone overlying the root apex (supraperiosteal injection). The fluid diffuses through the bone to reach and block the terminal nerve fibers at the apical foramen of the tooth. In general, a localized tooth block may be attempted on any tooth that has a vestibular alveolar plate of bone thin enough to permit diffusion of the solution to the apical nerves.
LOCAL ANESTHESIA OF MAXILLARY STRUCTURES
Local Infiltration
Teeth
Injection Sites
The upper lip or the cheek is retracted to expose the vestibular fold and the root apex or root apices of the tooth involved, and this is noted as the penetration site (Figure 11-2). The needle is introduced through the vestibular mucosa with the bevel of the needle pointing toward the mucosa. The syringe is aspirated. The bevel of the needle should come to rest facing and on the periosteal surface of the vestibular alveolar bone directly overlying the root apex. The proper amount of fluid is slowly injected at the site, and the fluid percolates through the alveolar bone to reach and block the terminal branches of the maxillary nerve entering the apical foramen.
Complications
There are relatively few complications associated with local infiltration techniques.
Palatal Gingiva and Mucosa
Injection Sites
The injection sites for palatal local infiltration are at a point midway between the gingival crest of the tooth and the midline palatal raphé (Figure 11-3). This ensures that the needle will enter a relatively thick portion of the palatal mucosa to minimize pain.
Block Anesthesia
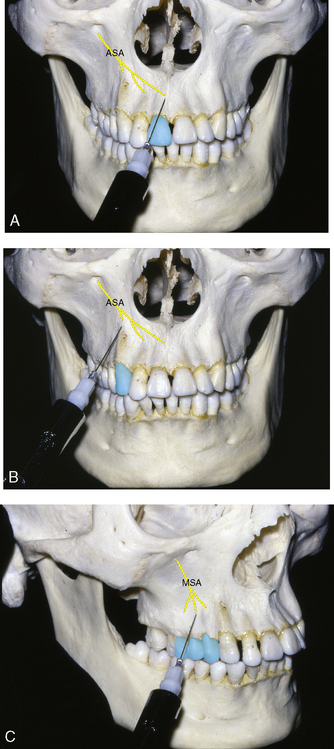
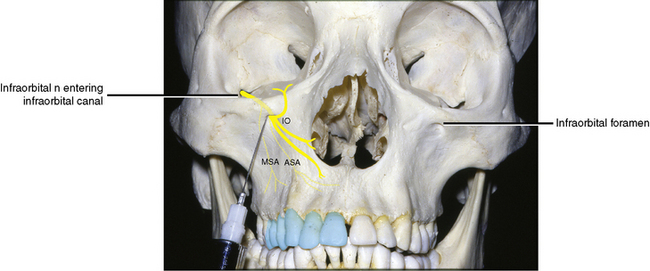
Anterior and Middle Superior Alveolar Blocks (Infraorbital Block)
The maxillary nerve enters the infraorbital groove in the floor of the orbit and changes its name to the infraorbital nerve. The maxillary nerve passes forward, giving off the middle superior and anterior superior alveolar nerves before exiting through the infraorbital foramen as facial branches (see Figure 7-58).
Injection Site
The site of injection is the mouth of the infraorbital canal (Figure 11-4). At this point, the middle superior and anterior superior alveolar nerves have branched from the main infraorbital nerve and are descending to their respective destinations. At the mouth of the canal, the terminal branches issue onto the face.
Complications
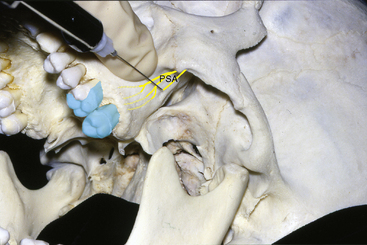
Posterior Superior Alveolar Block
The posterior superior alveolar nerve arises from the maxillary nerve just before it enters the infraorbital canal (see Figure 7-58). The nerve passes downward, along with corresponding branches of the maxillary artery, to the posterior or infratemporal surface of the maxilla.
Injection Site
The site of injection is the point where the posterior superior alveolar nerve enters the posterior superior alveolar foramen on the infratemporal surface of the maxilla (Figure 11-5). On the skull, this may be seen as several tiny foramina on the gently rounded, convex, posterior surface of the maxilla. In the living person, the area may be located by palpating the prominent zygomatic process of the maxilla in the vestibular fold. Posterior to this, the posterior surface of the maxilla may be palpated. If the mouth is opened too widely, the palpating finger is displaced by the coronoid process of the mandible and the attached temporalis tendon.
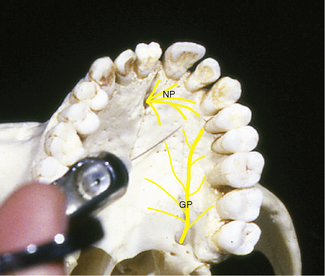
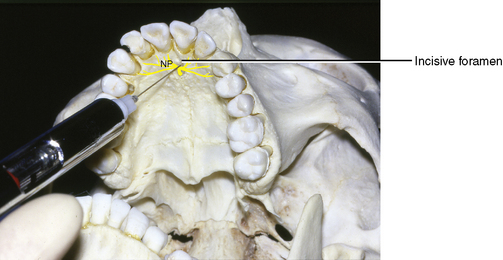
Nasopalatine Block
The nasopalatine nerve branches from the pterygopalatine ganglion and enters the nasal cavity through the sphenopalatine foramen (see Figures 7-60 and 7-82). It passes anteriorly and inferiorly along the nasal septum and exits onto the hard palate through the incisive foramen.
Injection Site
The injection site is the mouth of the incisive canal immediately posterior to the central incisor teeth (Figure 11-6). From the canal opening, branches of the nasopalatine nerve pass laterally and posteriorly. The right and left incisive canals merge on the palate as one incisive foramen. The opening on the dried skull is approximately 1.5 cm posterior to the alveolar crest between the central incisors. From this point, it funnels anteriorly behind the incisors. In the mouth, it lies in the midline immediately posterior to the incisive papilla. Topical anesthetic is used before injection. A very quick initial injection is performed just to one side of the incisive papilla. This eliminates the discomfort when the needle is subsequently placed into the incisive foramen through the incisive papilla.
Complications
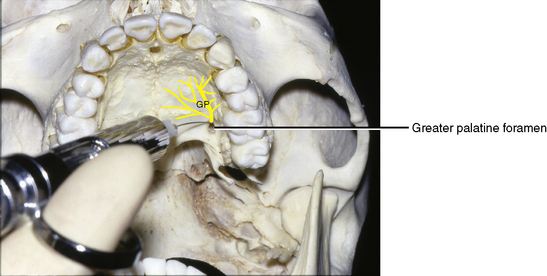
Greater Palatine Block
Nerves Blocked
The greater palatine nerve arises from the pterygopalatine ganglion of the maxillary nerve. It drops through the greater palatine canal and descends to emerge on the posterior aspect of the hard palate (see Figure 7-60).
Injection Site
The injection site is the mouth of the greater palatine canal (Figure 11-7). At this point, the greater palatine nerve emerges on the hard palate between the second and third molars, about 1 cm superior to the margin of the palatal gingiva. From here the nerve passes anteriorly in a groove to supply structures of the palate. The groove and foramen may be palpated under the palatal mucosa.
LOCAL ANESTHESIA OF MANDIBULAR STRUCTURES
Block Anesthesia
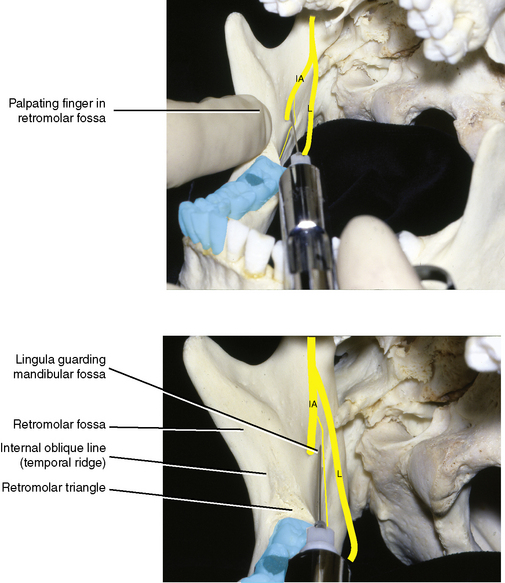
Standard Inferior Alveolar Block
The inferior alveolar nerve arises from the posterior division of the mandibular nerve and passes inferiorly laterally, and slightly anteriorly toward the midpoint of the internal aspect of the ramus of the mandible (see Figure 7-53). Here it enters the inferior alveolar canal, or mandibular canal, and travels anteriorly and medially in an arc below the roots of the mandibular teeth. It ends at the midline, as does its counterpart of the opposite side. At the level of the second premolar, the inferior alveolar nerve gives off the mental nerve, which passes through the mental foramen to emerge on the face.
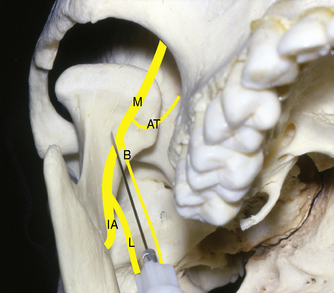
Injection Site
The mouth of the mandibular canal is the site accessible for injection (Figure 11-8). It is situated on the medial aspect of the ramus of the mandible. On the dried skull, if one were to ignore the coronoid and condylar processes, the ramus is roughly rectangular, and two imaginary diagonal lines intersect approximately at the mandibular foramen. The opening is large and funnels down into the canal within the bone. The anterior border of the foramen is guarded by a variable-sized, tongue-shaped projection of bone called the lingula. An imaginary line drawn posteriorly from the molar occlusal plane would lie approximately 0.5 cm above the foramen.
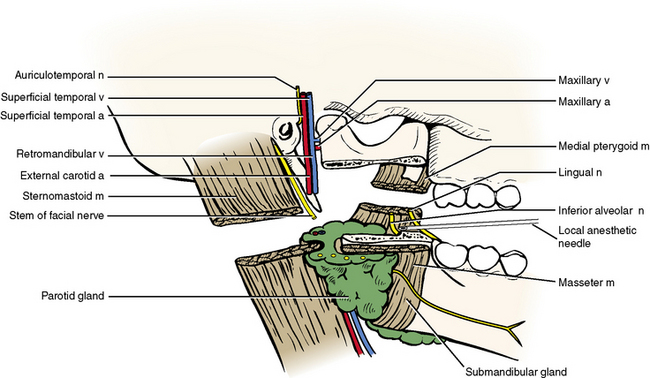
Relationships at Injection Site
Lateral. The tip of the needle should rest on the bone of the mandibular ramus at the funnel-shaped opening of the mandibular foramen, just above the neurovascular bundle (Figure 11-9).
Teeth Affected
All the mandibular teeth are anesthetized to the midline (pulps and periodontal ligaments).
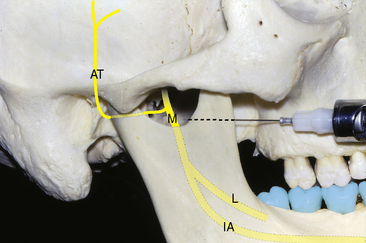
Gow-Gates Mandibular Nerve Block
Injection Site
The injection site for the Gow-Gates mandibular nerve block is considerably higher than that of the standard inferior alveolar. The needle tip in this method is placed in the infratemporal region below the insertion of the lateral pterygoid muscle at the anterior aspect of the condylar neck (Figure 11-10).
Akenosi (Closed-Mouth) Mandibular Nerve Block
Injection Site
The injection site for this technique lies within the infratemporal or pterygomandibular space but between the site for the standard inferior alveolar block and the Gow-Gates mandibular block (Figure 11-11). It is a preferred technique when opening the mouth is either painful or limited.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses