Soft tissue manipulation around implants in the esthetic zone
![]() Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
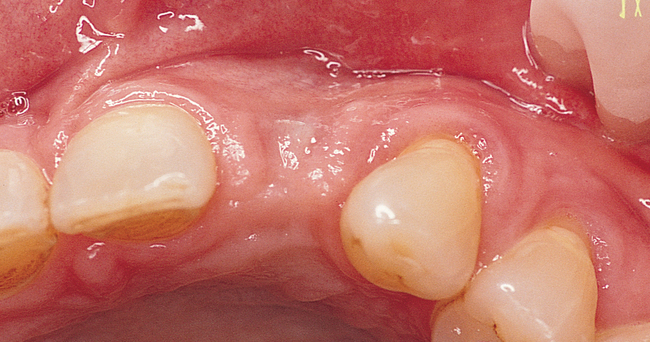
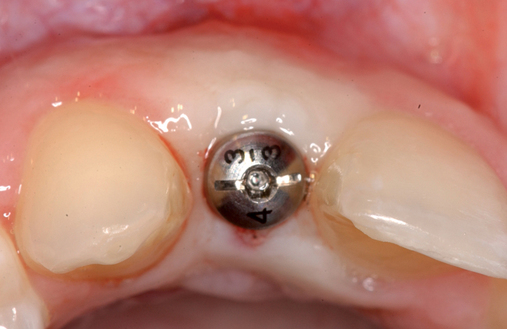
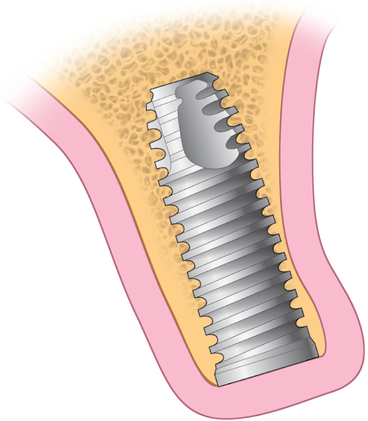
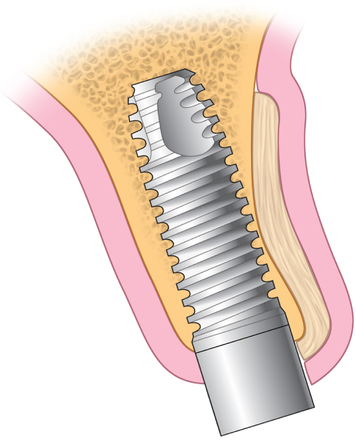
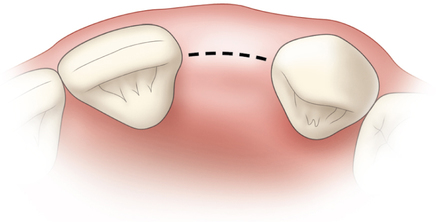
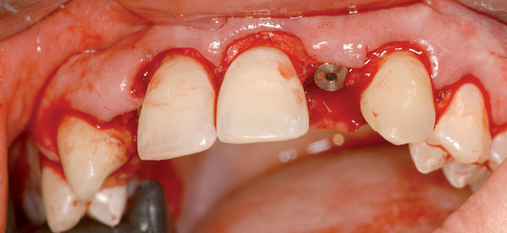
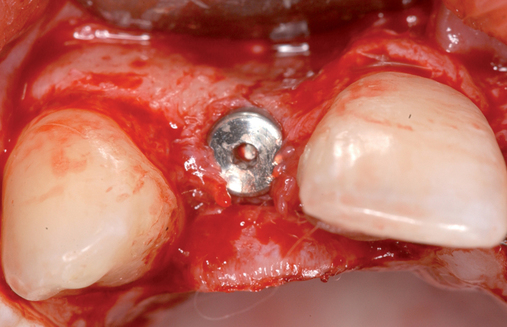
After an implant has been placed and all hard tissue grafting procedures have been completed, the implant site is evaluated to determine the need for additional soft tissue manipulation (Figure 10-1). Adjunctive procedures may be necessary to complete the surgical preparation of the implant site or to modify an existing implant restoration to achieve an esthetic restoration. The initial diagnostic esthetic setup or an esthetic temporary prosthesis can be used to assess the need for further ridge augmentation with soft tissue or for modification of the position of the gingival margin.
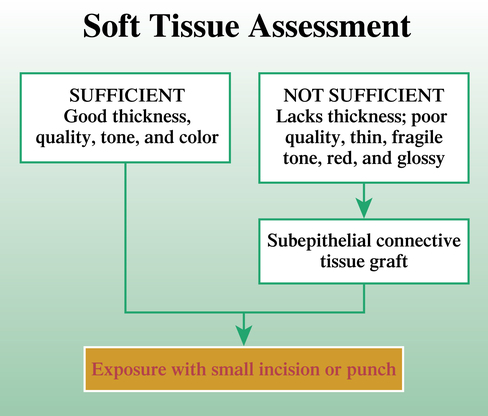
Physical examination of the patient is necessary, with attention given to specific anatomic and restorative details (Box 10-1). After the examination has revealed tissue characteristics that would benefit from an adjunctive soft tissue procedure, the specific soft tissue procedure is performed to correct the soft tissue deficiency or to modify the gingival margins, resulting in symmetry and an esthetic smile. Soft tissue deficiency usually involves thin gingiva, which benefits from increasing its thickness with connective tissue grafting. When the connective tissue thickness is normal or thick, the resulting texture, tone, color, and general appearance become similar to adjacent normal gingiva around natural, esthetic teeth.
A recommended course is to perform the hard tissue grafting first and establish the hard tissue foundation for the implant site. The implant can be placed at the time of hard tissue grafting (see Chapter 9). The connective tissue grafting can be placed after implant placement as a separate procedure. Six weeks after placement of the connective tissue graft, the implant can be exposed with minimal incisions, usually using a circular gingivectomy. Placement of connective tissue grafts at the time of hard tissue grafting or at implant exposure may yield satisfactory results in select cases, but this timing may also result in an esthetic problem if the connective tissue graft does not become revascularized and, as a result, becomes necrotic.
Soft tissue manipulation for ridge augmentation
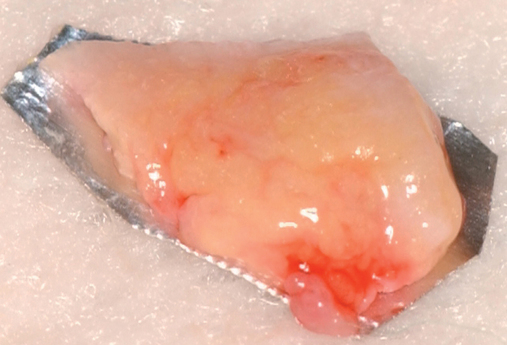
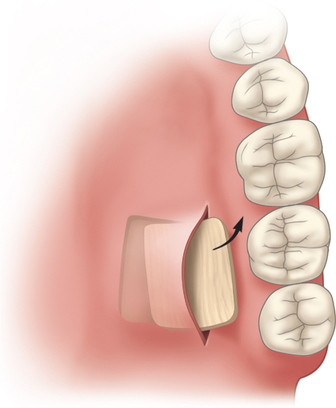
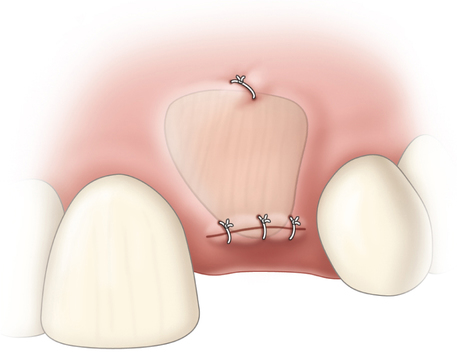
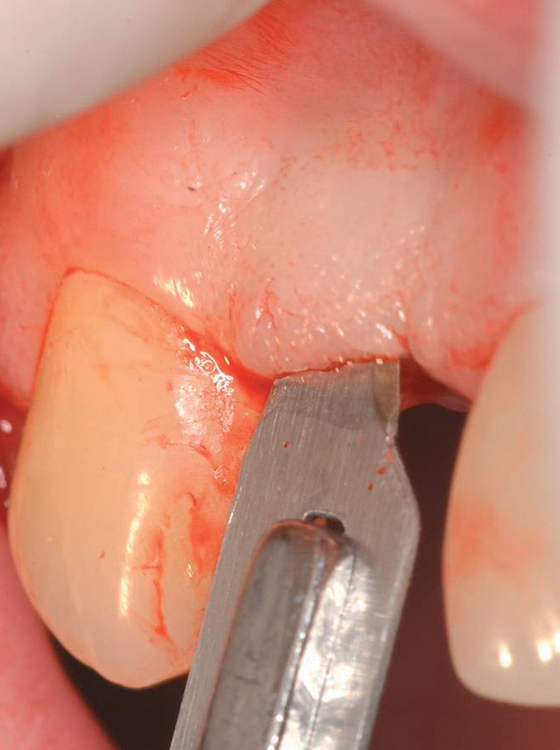
The subepithelial connective tissue graft is a sheet of connective tissue harvested from the palate (Figure 10-2). This soft tissue graft initially was described by Langer et al.
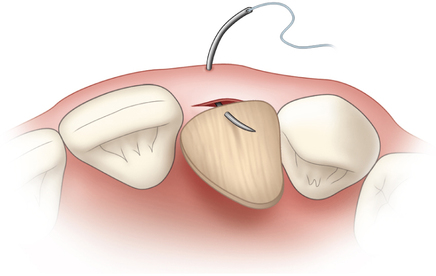
1–3 to correct ridge concavities and for root coverage, without deepithelialization of the palate.4,5 The connective tissue graft is quite versatile and flexible in its uses. Indications for use of a subepithelial connective tissue graft in dental implant sites include the following:
1. Thickening the gingiva to eliminate metal show from an underlying dental implant. The subepithelial connective tissue graft can thicken the gingiva 1 to 2 mm, depending on the thickness of the graft and contracture or shrinkage of the graft during healing.
2. Improving poor quality of the crestal gingiva. The gingiva’s appearance may be glossy rather than normal, healthy gingiva. The subepithelial connective tissue graft can change the appearance of thin, red, glossy gingiva to thick, pink, and normal stippled gingiva.
3. Increasing the labial convex contours of the soft tissue for a natural appearance of the final esthetic, implant-supported restoration. The 1 to 2 mm of additional crestal width provided by the subepithelial connective tissue graft can allow the restorative dentist to achieve an esthetic and symmetric soft tissue profile on the restoration.
4. Increasing the thickness of the gingiva to allow for sculpting. The restorative dentist can create an ideal gingival form for the esthetic restoration. By using the additional soft tissue thickness, the dentist can carve an esthetic form of the gingiva.
5. Correcting vertical height. The subepithelial connective tissue graft can be placed on the alveolar crest to augment the vertical height of the ridge 1 to 2 mm. The limit of this technique is not known at this time.
Subepithelial connective tissue grafting for ridge augmentation
The use of the subepithelial connective tissue graft to augment dental implant sites is based on the premise that after a tooth has been extracted, both the hard and the soft tissues change in form and quantity (see previous chapters for discussions on hard tissue). Interpositional soft tissue grafts can augment approximately 2 to 3 mm of width, but they contract over time and may lose 20% to 40% of their original thickness.6 Therefore, the clinician should expect some shrinkage from these grafts. The exact amount of shrinkage is not well documented and may vary from patient to patient.
Palatal roll technique
The palatal roll technique uses local tissue to augment the labial aspect of the alveolar ridge. The palatal roll technique was introduced by Abrams7 as a way to augment edentulous pontic sites for fixed prostheses. Tarnow and Scharf8 described a modified palatal roll technique for smaller ridge defects and for use when implants are exposed. Its use to augment implant sites has also been described by Block.9,10
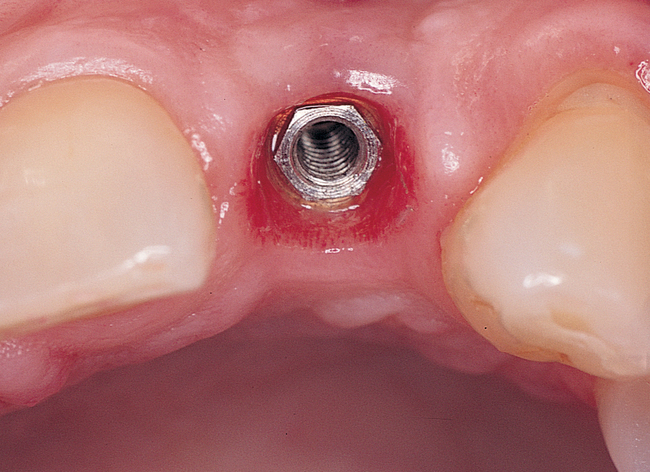
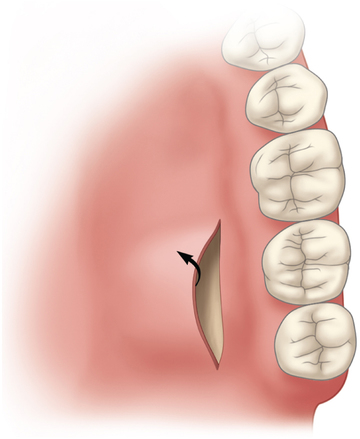
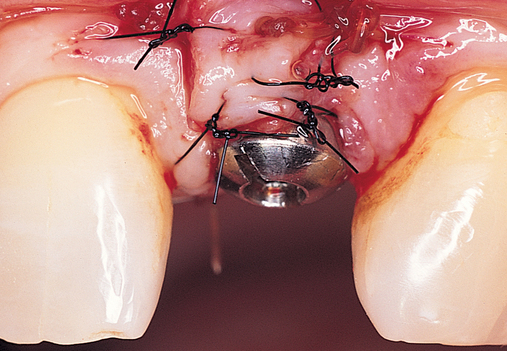
The indications for use of this technique have been narrowed. The use of subepithelial connective tissue grafts with a pouch procedure can predictably result in augmentations 2 mm thick, but the palatal roll may result in a gingival augmentation only 1 mm thick, with an occasional augmentation of 2 mm. Therefore, the palatal roll technique is reserved for small defects that primarily need small increases in gingival thickness to eliminate implant metal show through thin gingiva or for 2-mm horizontal gingival defects (Figure 10-3). This augmentation technique is useful at the time of implant exposure. When it is properly performed, papillae are preserved, and scars from incisions do not show because they are palatal in location with minimal labial reflection. The palatal roll technique is difficult to perform in regions where the palatal rugae are thick, preventing elevation of a thin palatal flap. For patients with thick rugae, a subepithelial connective tissue graft is used.




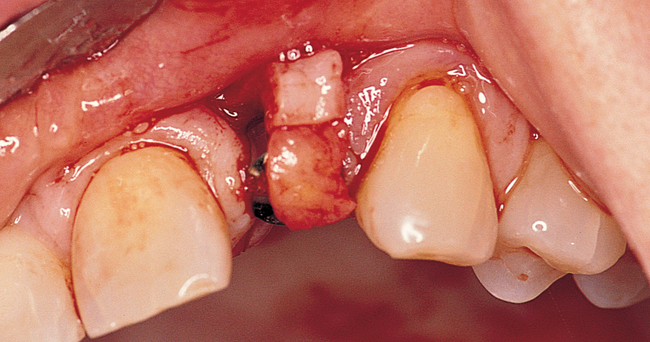


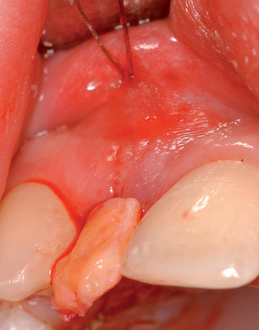
The palatal roll technique is useful after a tooth has been subluxed and lost from trauma without alveolar bone loss. Many of these patients have minor gingival tearing at the time of injury; when the gingiva heals, it is thinner than normal (see Figure 10-3).
At the time of implant placement, which may be 8 weeks or longer after the injury, the choice of incision design is no different than for any other implant placement. If the contact area between the teeth is less than 6 mm from the crestal bone, a sulcular incision from canine to premolar can be used. If the distance from the contact area to the crestal bone is 6 to 7 mm or more, a papilla-sparing incision is recommended.11 After it has been determined that adequate bone is present, the implant is placed. The esthetic stent is used to guide the surgeon on the vertical positioning of the implant with regard to the planned gingival margin and the labial position of the implant emerging just palatal to the incisal edge of the planned restoration. The implant usually is placed 3 mm apical to the gingival margin of the planned restoration, and the incision is closed without tension.
Transposition of palatal tissue for exposure of implants
When the patient has adequate bone for implant placement, it is prudent for the clinician to assess whether a connective tissue graft is indicated. Not every patient requires a connective tissue graft for an esthetic result. If the bone support is adequate, the color, tone, and thickness of the overlying tissue may be sufficient for routine exposure, eliminating the need for a soft tissue graft. A crestal incision can be made and the palatal keratinized tissue can be transposed to the labial aspect of the abutment and implant restoration, or a gingivectomy can be used to expose the implant. Papillae can be raised during exposure of the implant only if less than 7 mm of space is present between the proposed contact area and the crestal bone.11
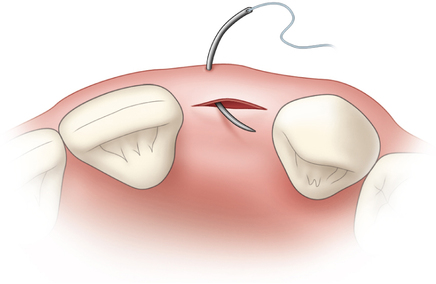
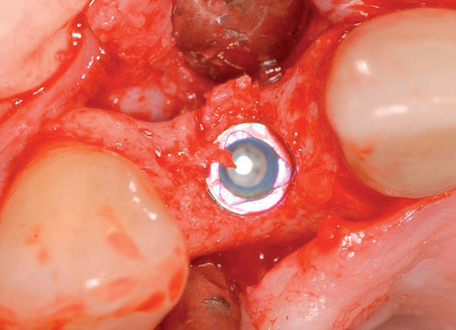
Recipient site preparation: Placement of a subepithelial connective tissue graft
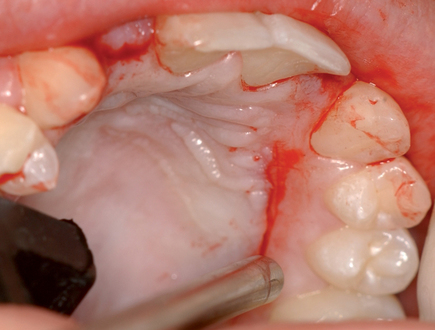
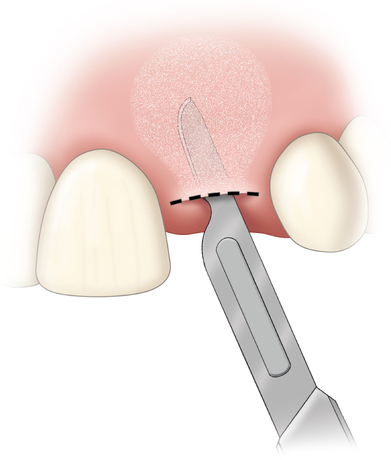
Placement of a subepithelial connective tissue graft without the need for removal of a membrane requires minimal incisions. Vertical release incisions are rarely needed, especially in the hands of an experienced clinician (see Figure 10-2). The goal is the placement of the soft tissue graft without creating vertical incisions, thus preventing scars. If vertical, inverted scars are present from a prior surgery, these scars can be undermined carefully and leveled with the development of the subcutaneous pocket and graft placement. A gingivoplasty of the tissue is performed to remove scar lines after the thickness of the gingiva has been increased to allow the surgical procedure.
Subepithelial connective tissue graft harvesting
The subepithelial connective tissue graft can be harvested with either an open or a closed technique. The open technique involves elevating a palatal flap of tissue with two vertical and one horizontal incision and excising a sheet of the underlying subepithelial palatal tissue (see Figure 10-2). For the closed technique, the connective tissue graft is harvested without developing a palatal flap. To avoid a flap, a single horizontal incision is made, and the pocket is developed without the vertical incisions, avoiding a flap. The underlying palatal mucosa is harvested after four incisions have been made through the periosteum within the pocket.
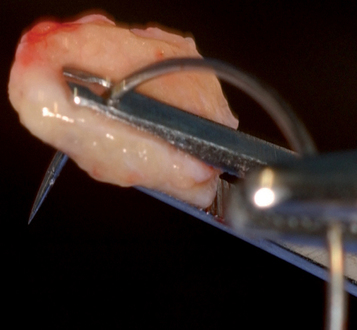
Open technique
For the open technique, the palatal mucosa is incised, and a pocket or flap is raised, exposing the underlying submucosal palatal tissue (see Figure 10-2, B). Three incisions are made on the palate. The first two incisions are made only through the palatal mucosa. These two incisions run vertically and determine the width of the graft. An extra 2 mm of width on both the anterior and the posterior vertical edge is recommended to avoid harvesting a graft that is too small. A horizontal incision is made approximately 2 mm from the gingival sulcus of the maxillary teeth. This horizontal incision can be made to bone or superficially to aid in the reflection of the thin palatal flap. To raise a thin palatal flap based on medial palatal tissue, a scalpel blade (typically #15c) is used to undermine the palatal tissue, with the blade kept parallel to the palatal mucosa. The palatal flap should be quite thin because preserving the thickness of the underlying palatal connective tissue is desirable. The palatal flap is elevated, with its base kept intact. From the inside aspect of the dissection, incisions are made to bone along the four edges of the planned subepithelial connective tissue graft. Because the incisions through the connective tissue graft are made through periosteum, a small periosteal elevator is used to separate the graft from the bone. The periosteum is raised and harvested as the undersurface of the graft. The connective tissue graft is removed with minimal instrument pressure placed on the tissue. Hemostasis is achieved with the aid of sutures or pressure. The palatal flap is sutured to its original position with resorbable 4-0 chromic sutures on a tapered needle.
The palatal vessels in the mesial posterior corner of the harvest site may bleed, especially when a large graft is harvested from a shallow palate.4,5 Often the graft’s longer length is taken anteroposteriorly, and the width is oriented toward the medial aspect of the palate, with the edge of the eventual graft kept away from the palatal vessels. If bleeding is encountered, the vessel may be identified and sutured, cauterized, or stick tied through the posterior palatal tissue to gain pressure hemostasis. A collagen hemostatic material can be placed within the confines of the flap. The overlying palatal tissue may become necrotic if excessive pressure is applied.
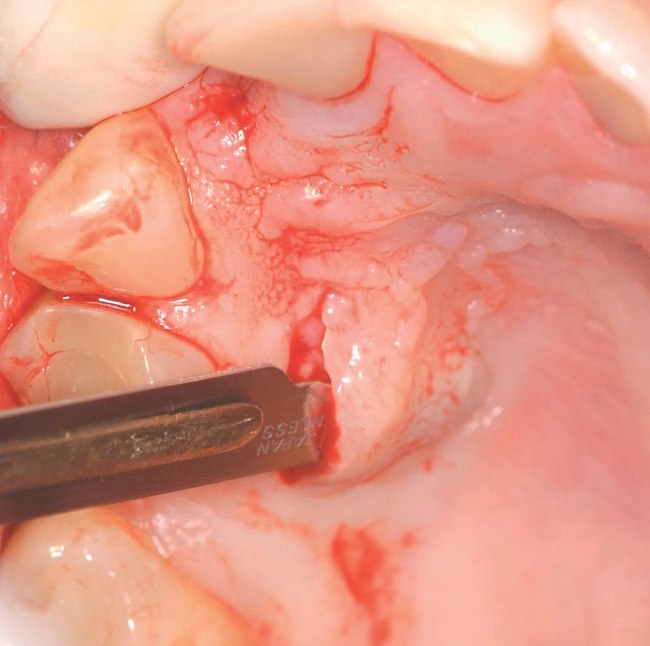
Closed technique
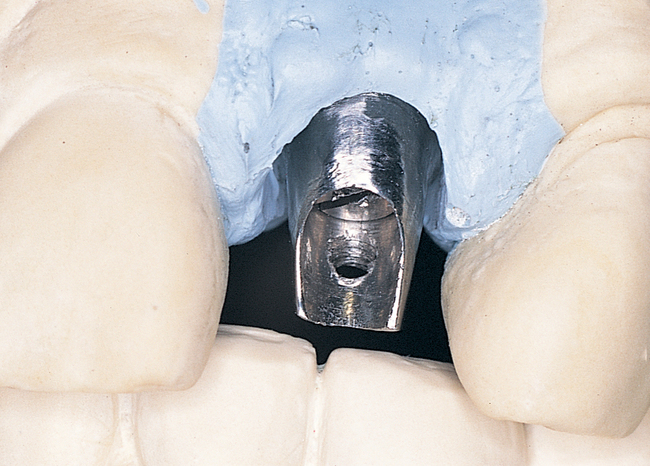
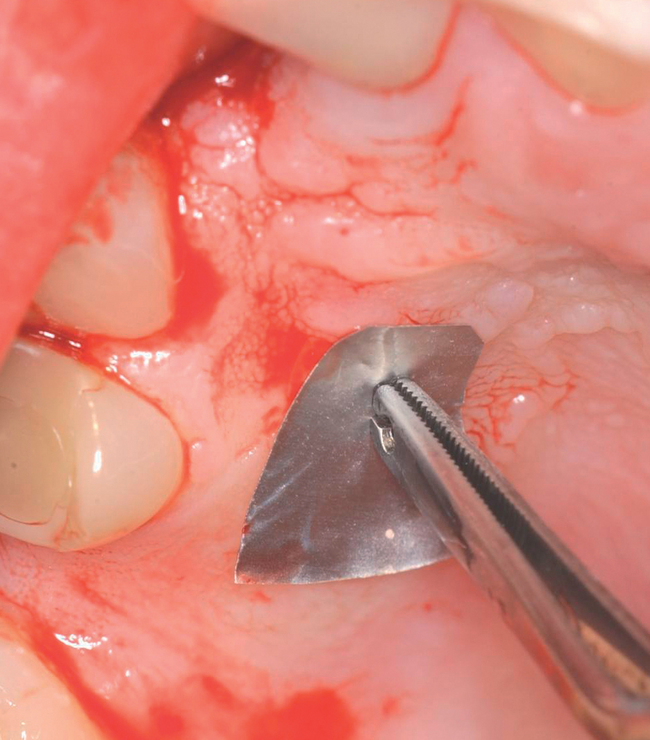
The closed technique for harvesting subepithelial connective tissue grafts was developed and popularized by Bruno.4,5 The closed technique uses one horizontal palatal incision without the need for additional vertical incisions (Figures 10-4 and
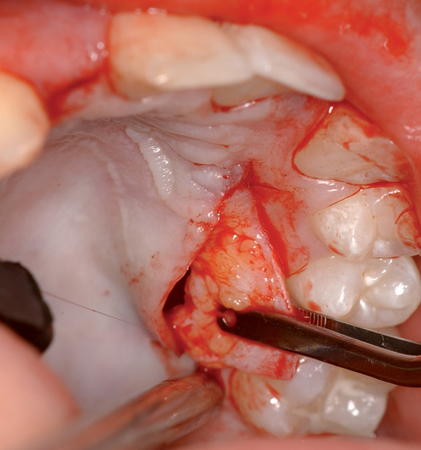



10-5). This technique allows the graft to be harvested with minimal postoperative morbidity. The closed technique results in a graft that is thickest along the edge of the horizontal incision and becomes thinner as it reaches the edge close to the depth of the graft site.



Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses