Chapter 10
Immediate Nonocclusal Loading Provisional Restoration: Intraoral Scanning, CADCAM Abutment, and Definitive Restoration Maxillary Central Incisor
LITERATURE REVIEW
Since the advent of Brånemark’s concept of osseointegration, the two-stage surgical approach has been the accepted protocol for endosseous implants (Brånemark et al. 1977). Other researchers questioned the validity of this protocol by introducing the concept of a single-stage surgical protocol but using the original unloaded healing times of 3–6 months (Buser et al. 1988). More current reports suggest that implants designed for two-stage surgical protocols can osseointegrate in predictable fashion, with high cumulative survival rates (CSRs), using various single-stage surgical protocols (Becker et al. 1997; Cooper et al. 2001; Garber et al. 2001).
Gelb et al. (2013) reported the results of a clinical study where one hundred seven implants (80 maxillary, 27 mandibular) in 52 patients were followed for 7–8 years post occlusal loading. One- and two-stage protocols were used for 38 and 69 implants, respectively. Thirty-eight single-tooth restorations and 22 fixed partial prostheses were delivered. All of the implants were subjected to delayed loading protocol, 4–12 months post implant placement. All implants were stable at insertion and at the long-term follow-up visits 7 and 8 years after functional loading. Mean marginal bone level change at the long-term follow-up appointments, when compared to baseline, was 1.49 ± 1.03 mm. The researchers reported no implant failures. Gelb and others concluded that this study demonstrated that dental implants with the TiUnite (Nobel Biocare, Yorba Linda, CA, USA) anodized surface demonstrated excellent long-term clinical and radiographic outcomes.
Immediate occlusal loading (IOL) of multiple, splinted implants has already been discussed in Chapter 9 and will not be repeated here. The reader is reminded that IOL, with high CSRs, has been recognized as a protocol involving multiple, splinted implants placed and restored within 3 days of the surgical procedures (Schnitman et al. 1997; Testori et al. 2003; Ostman et al. 2012; Romanos et al. 2013).
Treatment in the aesthetic zones of partially edentulous patients presents clinicians with numerous challenges including, but not limited to, the presence or absence of gingival papillae, gingival symmetry, three-dimensional (3D) locations of implant restorative platforms, emergence profiles of the implant restorations, and clinical restorations that replicate the remaining natural teeth (Saadoun and Sebbag 2004).
Alterations of the hard and soft tissues after tooth extraction or secondary to trauma and/or dental disease and in the contours of the adjacent natural teeth may result in edentulous sites that are not appropriate for implant placement without additional surgical procedures (Figure 10.1). With older protocols, a healing time of 9–12 months was recommended after extraction prior to implant placement (Adell et al. 1981). Other researchers have advocated immediate or delayed immediate implant placement (Schulte and Heimke 1976; Tarnow and Fletcher 1993; Cooper et al. 2001).
Penarrocha et al. (2008) reported on the results of a study that included maxillary lateral incisor implants with nonocclusal loading provisional crowns. Their clinical report series described a treatment modality that involved immediately dental implants in maxillary lateral incisor sites using noncemented immediate provisional crowns retained with calcinable copings (prosthetic components used in preparing the metal for the definitive prosthesis). Ten implants were placed in eight patients for the replacement of maxillary lateral incisors: two immediate and eight corresponding to cases of agenesis. All were subjected to immediate rehabilitation with provisional acrylic resin crowns without occlusal loading. One implant failed 3 weeks after placement due to acute local trauma. The other nine remained functional, with normal clinical and radiological characteristics after a minimum of 12 months post placement and immediate restoration. The authors stated that immediate placement of fixed provisional restorations retained by friction in maxillary lateral incisor areas offered an aesthetic solution, eliminated removable provisional restorations, and avoided implant failures associated with excess cement or screw loosening. Moreover, in the case of extractions, immediate placement and provisionalization of implants in maxillary lateral incisor areas can effectively optimize the peri-implant aesthetic results by maintaining the existing hard and soft tissue architecture of the missing tooth. The authors also stated that since cement was not used and the authors did not use screw retention, and the provisional crowns were not functionally loaded, the risk of complications was minimized. Aesthetic success in the aesthetic zone depends on harmony and anatomic contours of the hard and soft tissues (Wohrle 1998).
Figure 10.1 Occlusal view of a partially edentulous anterior maxillary ridge 14 months post extraction. Note the collapse of the ridge in the area of the missing right central incisor.

Wohrle (1998) reported on the success of 14 consecutive cases where nonrestorable maxillary lateral incisor teeth were extracted and tapered implants with various surfaces were placed and restored with provisional restorations on the same day (Wohrle 1998). None of the restorations had any occlusal contacts; patients were instructed to avoid functioning with/on the implants and restorations for periods up to 6 months postoperatively. All of the implants achieved insertional torque values of at least 45 N cm. This was a quantitative measurement of implant primary stability. Two of the implants were followed for 31–36 months, 2 for 25–30 months, 5 for 19–24 months, 12 for 13–18 months, 14 for 7–12 months, and 14 for 0–6 months. None of the implants were lost; changes in the levels of the soft tissues surrounding the restorations were greater than 1 mm in just two patients. Soft tissue loss never exceeded 1.5 mm; Wohrle considered that the harmony and continuity of the hard and soft tissues were predictably achieved in all cases (Figures 10.2 and 10.3).
In the case of certain anatomic defects, some patients are not candidates for immediate implant placement and provisional restoration (Figure 10.4). In these cases, grafting needs to be accomplished first and may entail two or more surgical procedures to harmonize the hard and soft tissues prior to fabrication of a definitive abutment and crown (Figure 10.5).
Figure 10.2 Intraoral view of a provisional restoration without occlusal contacts (INOL) that restored an implant that replaced a maxillary left lateral incisor on the day of surgery.

Figure 10.3 Definitive restoration 12 months post insertion of the implant in Figure 10.2. The implant replacing the maxillary left canine tooth had previously experienced gingival recession and crestal bone loss prior to implant placement for the maxillary lateral incisor.

Hui et al. (2001) reported on the results of a clinical study that provided immediate nonocclusal loading (INOL)-type restorations in the anterior maxillary aesthetic zone for 24 patients. Thirteen of the 24 patients had immediate implant placement after tooth extraction. Primary implant stability was defined as insertion torque values of at least 40 N cm; none of the restorations had occlusal contacts in centric or eccentric positions. The follow-up periods ranged from 1 to 15 months. Hui et al. (2001) reported that all of the implants were stable. The aesthetic results were considered to be satisfactory by all patients.
Figure 10.4 Clinical occlusal image of a relatively large labial defect in the maxillary left central incisor edentulous area. This patient was not a candidate for an implant immediately; grafting was needed prior to implant placement.

Figure 10.5 Clinical labial image of the implant restoration from Figure 10.4. After osseous healing occurred post grafting, the patient was a candidate for implant placement and immediate provisional restoration.

Kan et al. (2003) performed a similar study as those noted previously with 35 patients. Thirty-five, threaded, hydroxyapatite-coated implants were placed and restored with nonocclusal loading-type provisional restorations immediately post implant placement. The implants were placed with primary stability, but the authors did not define this term quantitatively. Kan and others reported that, at 12 months, all implants were osseointegrated with mean midfacial gingival level and mesial/distal papillae level changes from pretreatment to 12 months post treatment of −0.55 ± 0.53 mm, −0.53 ± 0.39 mm, and −0.39 ± 0.40 mm, respectively. Kan et al. (2003) reported that all of the patients were pleased with the aesthetic results. The researchers concluded that favorable CSRs, peri-implant tissue responses, and aesthetic outcomes could be achieved predictably with this protocol.
Figure 10.6 Intraoral view of a large fenestration within the alveolus after extraction of the maxillary right second premolar. Due to the defect and the need for bone grafting prior to implant placement, this patient was not a candidate for immediate implant placement.
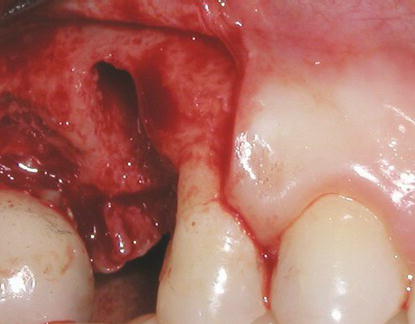
Other authors have also demonstrated predictable, high CSRs with minor variations of the INOL protocols identified previously (Drago and Lazzara 2004; Saadoun and Sebbag 2004; Wilson et al. 2013). Successful treatment appears to be dependent on implant primary stability (insertional torque values of at least 35 N cm at implant placement); the absence of infection or anatomic defects within the alveolus (Figure 10.6). Provisional restorations must not have occlusal contacts in centric or eccentric mandibular positions.
However, there are also several studies that restored immediate, single-tooth, unsplinted provisional restorations with occlusal contacts at the time of implant placement (Ericcson et al. 2000; Chaushu et al. 2001; Cricchio et al. 2013). Ericcson reported that 2 of the 12 implants restored with this protocol failed within 5 months of implant placement. Chaushu reported that the 1-year CSR for the immediately loaded single-unit implants placed into fresh extraction sites was 82.4%. For those implants that were placed into healed edentulous sites, the CSR was 100%. Chaushu and others concluded that an IOL protocol for single-unit implants may have higher than acceptable failure rates and that this protocol, if used, should only be used in healed extraction sites. Cricchio et al. (2013) concluded that within the limits of their study, maxillary sinus membrane elevation with simultaneous placement and immediate loading of implants without the use of additional grafting material demonstrated predictable results after 2 years of functional loading. Moreover, they also concluded that evidence of intrasinus bone formation around the implants was found in all patients.
Table 10.1 INOL protocol for single, unsplinted provisional implant restorations.
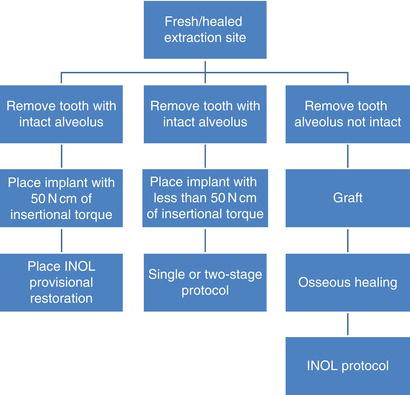
INOL is a protocol that is generally restorative driven, in that a fixed restoration is placed at the time of implant surgery. With this protocol, patients will not have to wear any sort of removable prosthesis. The implant surgeon and restorative dentist have to be prepared for multiple contingencies related to the proposed surgery: quality and quantity of bone, implant primary stability (at least 35 N cm of insertion torque), and location of the gingival margins. If any of the aforementioned criteria are not satisfied in a given situation, an implant may or may not be placed; a provisional implant restoration may or may not be placed (Table 10.1). This protocol may be said to be restorative driven, but surgically determined.
CLINICAL CASE PRESENTATION
Appointment 1: Initial Clinical Visit (3/4 Hour)
A 45-year-old female patient presented to the attending clinician with a chief complaint of “I need someone to look at one of my front teeth.”
Figure 10.7 Preoperative clinical view of the patient smiling, as she presented to the attending clinician. The patient exposed approximately 1–2 mm of maxillary anterior gingiva with smiling.

Figure 10.8 Preoperative labial view of the anterior maxillary segment that demonstrated adequate restorative volume for an implant restoration for tooth #9; it also demonstrated the lack of interproximal papilla between the two maxillary central incisors.

History of the Present Illness
The dental history relative to tooth #9 included trauma to the anterior maxillae approximately 5 years previously. The tooth had been getting darker over the last 2–3 years (Figures 10.7 and 10.8).
Radiographs
Preoperative radiographs consisted of periapical and panoramic radiographs (Figure 10.9). Based on the clinical examination and anatomic location, the implant surgeon decided that a computed tomography (CT) scan was not necessary.
Figure 10.9 Radiograph at the time of the initial presentation that demonstrated crestal bone loss interproximally between the two central incisors and horizontal bone loss between the left maxillary central and lateral incisors.

Figure 10.10 Preoperative occlusal view of the anterior maxillary teeth. It was determined that there likely would be adequate buccal/lingual width for implant placement regarding the nonrestorable left central incisor.

Physical Examination
This patient presented with an otherwise intact dentition and mild gingivitis and was caries-free. The maxillary left central incisor was in a satisfactory labial/lingual position (Figure 10.10).
Figure 10.11 Labial view of the maxillary diagnostic cast with denture tooth in place prior to making the surgical guide.

Figure 10.12 Laboratory occlusal view of the diagnostic cast with denture tooth in place prior to making the surgical guide.

Diagnostic Casts
Diagnostic casts were fabricated from alginate impressions. The original supraerupted maxillary left central incisor was removed from the cast; a denture tooth was used to identify the optimal location for the implant restoration (Figures 10.11 and 10.12).
Surgical Guide
A surgical guide was fabricated to assist the surgeon in identifying the optimal location of the planned implant restoration. The surgeon needed to know the 3D position of the planned implant restoration in order to place the implant in its correct location. The surgical guide was made by duplicating the diagnostic cast with the denture tooth in place, pouring that impression in dental stone, and then making a vacuum-formed matrix (125 mm Biocryl Material, Great Lakes Orthodontics, Tonawanda, NY, USA) (Figure 10.13). The author has found it prudent to make the surgical guide on a duplicate cast because the cast is generally damaged during fabrication of the surgical guide.
Figure 10.13 Surgical guide in place on the diagnostic cast. The guide was modified specifically to include the optimal location of the gingival margin for the implant restoration. The surgeon needed this landmark to place the implant in its proper vertical position.

Diagnoses
The following diagnoses were established:
Prognosis
Based on the patient’s age, residual alveolar ridge, occlusion, and overall general health, the attending clinician felt that the prognosis for this patient’s treatment was excellent.
Appointment 2: Consultation Restorative Dentist/Patient (1/2 Hour)
The patient returned for the definitive consultation appointment where three treatment plans were presented: The first treatment option described placement of a 4 or 5 mm diameter implant with primary stability (at least 50 N cm insertion torque), placement of an interim abutment and provisional crown without occlusal contacts, and osseointegration and fabrication of the definitive implant-retained crown (Table 10.2). The second treatment option described the replacement of the maxillary left central incisor with a 3-unit fixed partial denture (FPD) (Table 10.3). The third treatment option deferred prosthetic treatment at this time (Table 10.4).
Benefits and limitations of each treatment option were described in detail in the written treatment plans. The prosthodontic fees or ranges of fees for each procedure were also listed on each treatment plan. The patient was given copies of the treatment plans. The patient consented to proceed with the first treatment plan including extraction and immediate implant placement and was referred to an oral surgeon for the surgical diagnostic work-up.
Appointment 3: Consultation Restorative Dentist/Surgeon (1/2 Hour)
This appointment should precede the surgeon’s examination appointment. This consultation is critical for the long-term functional and aesthetic success of implant treatment. It is essential that the restorative dentist explain to the surgeon the physical and radiographic findings, the diagnosis, and the treatment options that were explained to the patient. This particular case presentation was technically demanding, and the consultation between restorative dentist and the oral surgeon was completed within 45 minutes.
Size and Type of Implant
In this case, the patient was missing a single tooth and appeared to have adequate space for both the surgical and prosthetic phases of implant treatment. The attending clinician suggested a 5 mm diameter implant with an internal connection be placed since this size implant most closely approximated the size of the missing tooth. This implant was machined with a restorative platform that was 4.1 mm in diameter; the body of the implant was 5 mm in diameter (Tapered Certain® PREVAIL® Implant, Biomet 3i, Palm Beach Gardens, FL, USA). This implant system incorporated platform switching into the implant/abutment connection. This implant system, per the manufacturer, featured integrated platform switching by incorporating a coronal bevel design that medialized the implant/abutment junction (IAJ) (Figure 10.14).
Platform switching has been correlated with decreased crestal bone loss by altering the 3D position of the inflammatory response associated with IAJ (Figure 10.15). Vandeweghe and De Bruyn (2012) conducted a randomized controlled clinical trial to evaluate whether platform-switched implants could preserve marginal, crestal bone around implants up to 6 months post occlusal loading. Vandeweghe and De Bruyn selected 15 patients; each patient received one customized wide body implant, with external hex connections located eccentrically within the edentulous sites that allowed an extra 1 mm switch on one side. The hexes were positioned at random at the mesial or distal side; the implants were loaded after 6 months of nonsubmerged healing. Patients were examined at 3, 6, and 12 months after surgery, when radiographs were taken to evaluate bone levels. At 12 months, the mucosal thickness was measured using a periodontal probe. All implants survived, and the mean overall bone loss, calculated from both the switched and nonswitched sides, was 0.39 mm (SD 0.33, range 0.00–1.45), 0.85 mm (SD 0.59, range 0.10–2.50), and 0.80 mm (SD 0.46, 0.26–1.89) after 3, 6, and 12 months, respectively. Significantly more bone loss was observed at the nonswitched sides compared to the switched sides at 3 months (0.51 mm vs. 0.28 mm, P = 0.019), 6 months (1.05 mm vs. 0.64 mm, P = 0.002), and 12 months (0.94 mm vs. 0.66 mm, P = 0.002). The authors concluded that the outcomes of this randomized trial were similar to the results reported in earlier studies and suggested that platform switching may decrease crestal bone loss by 30%. Although the sample size was limited, the authors also concluded that it seemed that the creation of a biologic width affected peri-implant bone loss to a significant extent and that platform switching was only effective when peri-implant mucosal thickness allowed the establishment of a physiologic biologic width. Similar results were reported by Telleman et al. (2012) and Al-Nsour et al. (2012).
Table 10.2 Treatment plan #1 (implant restoration).
| Diagnosis: Nonrestorable maxillary left central incisor secondary to trauma | ||
| Restorative services | Insurance code | Fee |
| Comprehensive oral evaluation | ______ | ______ |
| Diagnostic casts | ______ | ______ |
| Panoramic radiograph | ______ | ______ |
| Diagnostic wax pattern (#9) | ______ | ______ |
| Surgical guide | ______ | ______ |
| Referral to oral surgical office: | ||
|
1. Evaluate and treat for replacement of the nonrestorable maxillary left central incisor with an INOL.
2. Place a 4 or 5 mm diameter internal connection implant with a single-stage protocol, if possible.
3. The implant should have primary stability as defined by insertional torque value of at least 50 Ncm. If the implant does not achieve this insertional torque value, place a healing abutment with the following dimensions: 5 mm restorative platform, 6 mm emergence profile, and 2–4 mm collar height.
4. An interim abutment (PreFormance Post 5 mm restorative platform, 6 mm emergence profile, 4 mm collar height, IWPP564G) should be placed at the time of surgery. The abutment screw (IUNIHG) should be hand-tightened. Please make sure that the interim abutment is not in occlusion in centric occlusion and eccentric excursions.
5. Discharge the patient back to the author for fabrication of the INOL provisional restoration.
6. Postoperative instructions
|
||
| Insurance code | Fee | |
| Restorative reevaluation | ______ | ______ |
| Premachined interim implant | ||
| Abutment and INOL provisional | ||
| Restoration | ______ | ______ |
| Osseointegration | ||
| Custom implant abutment | ______ | ______ |
| Abutment-supported porcelain-fused | ||
| crown (noble metal) | ______ | ______ |
| Yearly recall appointment | ______ | ______ |
| Periapical radiograph | ______ | ______ |
| Benefits of Treatment Plan #1 The nonrestorable tooth in the front part of the upper jaw will be replaced with an implant restoration that will not be removable by the patient. Occlusion (bite) will be optimized. Patient should enjoy improved function with good aesthetics on a long-term basis. Some of the services may be eligible for payment under your medical insurance policy as the permanent tooth was lost secondary to an accident. The teeth adjacent to the missing tooth will not have to be prepared for crowns (caps). |
||
| Limitations of Treatment Plan #1 Cost, Complexity, and Length of Treatment (4–12 Months). Implants are generally successful in the front part of the upper jaw approximately 96–99% of the time. For this protocol to be successful, the patient must agree to completely avoid placing food anywhere near or on the temporary crown for at least 2 months after the implant has been placed. Chewing on the temporary crown before the implant has bonded into the bone will jeopardize healing and may result in loss of the implant. If you admit to chewing on the implant, additional fees will be charged to you for redoing the treatment. Additional treatment, including bone grafting, may be necessary. The implant has to be placed optimally and be secure enough at the time of placement for the aforementioned treatments to be accomplished. If the implant cannot be placed optimally or it is not secure enough in the bone, changes in the treatments (surgical and prosthetic), fees, and designs will be likely. After the treatment has been completed, the patient needs to return to this office at least once per year (may be in conjunction with planned recall appointments) for follow-up which will include radiographs (X-rays) to assess osseointegration of the implant, status of the occlusion, health of the soft tissues, and the integrity of the implant/abutment connection. This treatment plan itemizes only the prosthetic phase of treatment. |
||
| Patient signature ____________________ | ||
| Date ____________________ | ||
| Witness ____________________ | ||
| Date ____________________ | ||
Table 10.3 Treatment plan #2 (fixed bridge).
| Diagnosis: Nonrestorable maxillary left central incisor secondary to trauma | ||
| Restorative services | Insurance code | Fee |
| Comprehensive oral evaluation | ______ | ______ |
| Diagnostic casts | ______ | ______ |
| Panoramic radiograph | ______ | ______ |
| Diagnostic wax pattern (#9) | ______ | ______ |
| Tooth #9 (upper left front tooth) | ||
| Porcelain-fused-to-metal (PFM) pontic | ______ | ______ |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


