10
Discoloration of Teeth
10.1 Introduction
Discoloration of teeth is when the colour of all or several teeth or (part of) a tooth is outside the white-yellow spectrum. The colour (=hue) of an object is determined by which wavelengths of white light it absorbs and reflects, for instance a red object only reflects the red wavelength and absorbs the rest. Chroma (=saturation) refers to the strength of the colour, its purity, that is, how more or less intense it is. Brilliance (=value) is the brightness of colours on a scale from black (=0) to white (=100). The amount and spectral composition of the light co-determine the hue and brilliance, for instance the differences in blue colour of the northern sky in the day or at dusk. The colour that is perceived is affected by a number of factors, including the observer.115
The permanent teeth are commonly white-yellow in colour, with hints of brown, pink and grey-green. The deciduous teeth are bluish white. Inheritance is responsible for inter-individual tooth colour differences.114 Intra-individually, the colours of the different classes of teeth differ slightly, for example, the permanent maxillary canines are darker than the permanent incisors.
The enamel surface reflects most wavelengths, but the light that is transmitted through the translucent enamel scatters and is reflected by the dentine before it emerges from the tooth. The impact of the yellow-orange dentine on the perceived tooth colour is greater in the cervical region than in the centre of the crown due to differences in the enamel thickness in these areas. At the incisal edges, the thin enamel is darker, reflecting the lack of light within the mouth, more so when it is worn. Locally, different wavelengths of light may be absorbed, resulting in, for instance, brown spots (combined red, green and yellow wavelengths). Darker skin makes the teeth appear whiter: in one study, 50% of subjects with darker teeth had a fair and 17% had a dark complexion.179 More severe discolorations are expressions of generalized or local pathological processes, which may have diagnostic implications.367
Colour Determination
The colour of a tooth can be determined and recorded by comparing the tooth with a set of artificial teeth, for instance the Vitapan Classical or the Trubyte Bioform colour-ordered shade guide. The Vitapan shade guide has 16 shades divided into four colour groups (“hues”), each one ordered from light to dark, that is, A1–A4 (including A3.5), B1–B4, C1–C4 and D2–D4, The Trubyte Bioform colour-ordered shade guide has 24 shades When used to evaluate the effects of bleaching, the four groups are pooled and ordered from the lightest to the darkest shade, as shown in Figure 10.1. Colour photos or slides may be used to record tooth colours.359
Figure 10.1 Vitapan Classical shade guide: the colours are ordered from light to dark.

The tooth colour also can be determined by photospectrometry, which measures the different colours of the whole labial surface at once. Colorimeters and high-resolution digital cameras may misread the real colours, sometimes considerably.94 The colour measurement is presented as, for instance, the Vitapan shade guide number and as a numerical value. Every colour can be described with the numerical three-dimensional CIE (International Commission on Illumination) L*a*b* colour system, in which:
- L* represents the brilliance (L = 0 is perfect black, and L = 100 is perfect white)
- a* is the parameter for the green-red axis: positive values are red, negative values are green (an object cannot be red and green at the same time)
- b* represents the yellow-blue axis: positive values are yellow, negative values are blue.
Classification of Tooth Discoloration
Discoloration can occur during odontogenesis (endogenous/intrinsic discoloration) due to incorporation of pigments in the developing hard tissues. Developmental hypocalcification also causes the tooth colour to change. Post-eruption, infiltration of the enamel/dentine by pigments can occur via the pulp (endogenous) or the mouth (exogenous/extrinsic).367 Deposits of exogenous pigments on the enamel surface,368 that is, the acquired salivary pellicle, does not discolour the tooth tissues themselves: the term pseudo-discoloration seems more appropriate here. Loss of enamel or dentine underlies other pseudo-discolorations. Based on such considerations, tooth discoloration can be classified as shown in Table 10.1.
Table 10.1 Classification of tooth discoloration
| Type of discoloration | Description |
| 1. Endogenous | |
| 1.1 Developmental | Discolouring pigments are incorporated into the dental hard tissues during odontogenesis |
| Examples: hypocalcification and biliary anomalies | |
| 1.2 Post-eruptive | Infiltration of discolouring pigments into dentine occurs via the pulp |
| Examples: sclerotic dentine, tertiary dentine and necrotic pulp | |
| 2. Exogenous – post-eruption | |
| 2.1 Infiltrative | Discolouring pigments infiltrate the enamel/dentine from the mouth |
| Examples: agents from cavity fillings/root canal fillings infiltrating dentine | |
| 2.2 Pseudo-discoloration | Stains on tooth surfaces |
| Example: chlorhexidine stain | |
| 3. Endogenous or exogenous – post-eruption breakdown | Enamel loss leads to exposed dentine, which is eventually secondarily infiltrated exogenously |
| Example: Pulp showing through after internal or cervical dentine resorption | |
Attribution to a discoloration category may be difficult. For instance, enamel that is opaque due to irradiation with high-intensity laser which causes water loss with light scattering, and brown-coloured dentine due to non-enzymatic collagen denaturation or oxidation of a dentine component.22
10.2 Endogenous Discoloration
Often all the teeth are affected, although occasionally only a few may be discoloured. Development enamel hypocalcification (opacities) and hypoplasia and their numerous causes are described in detail in Chapter 3.
10.2.1 Endogenous Developmental Discoloration
Endogenous developmental tooth discoloration is due to incorporation of discolouring pigments in the dental hard tissues at the time of odontogenesis.
Amelogenesis Imperfecta (pp. 79–86)
The subtypes are associated with different discolorations: brown (to black), mottled brown, (opaque-)white, yellow, glass-like, alternating white and normal coloured bands (Figure 10.2 and Table 3.4).
Figure 10.2 A–D Discoloration in various subtypes of hereditary amelogenesis imperfecta.

Biliary Anomalies
In people with congenitally defective biliary ducts or biliary atresia (1 : 10 000 live births)389 dark green to yellow-brown bile pigments are deposited in both dentitions.97 149 232 316 389 Dentine formed after liver transplantation has a normal colour.144 316
Coeliac Disease (p. 63)
Symmetrical enamel hypoplasia may be accompanied by discoloration, which is chronologically distributed per quadrant.
Molar-Incisor Hypocalcification (Cheese Molars) (pp. 53–4)
The partly brown discoloured first permanent molars may be accompanied by white and yellow opacities in the incisors.
Chemotherapy (pp. 77–8)
Discoloration of teeth, mostly likely brown colour, have been reported in children after chemotherapy.
Congenital Syphilis (pp. 54–5)
The corkscrew-shaped incisors can be dirty grey in colour. The hard tissue between the multiple cusps of the first permanent molars may be brown in colour.
Congenital Porphyria
Porphyrin traces are present in all people. Increased porphyrin levels lead to discoloration of all hard dental tissues. In particular, the dentine in the deciduous dentition discolours a dark yellow-brown, red-brown and purple-brown (erythrodontia), all of which fluoresce red under ultraviolet light.227 The enamel may be thin.
Porphyrin is needed to synthesise haemoglobin. An inherited enzyme disturbance precludes the formation of one of the precursors from which “haem” (=ferroprotoporphyrin, part of haemoglobin) is formed. There are many types of porphyrin and they occur across the whole of the animals and plant kingdoms.
The skin of patients with congenital porphyria is hypersensitive to ultraviolet (UV) light and it blisters and scars under the light in the operating theatre. The oral mucosa is vulnerable to mild trauma. The patients also have haemolytic anaemia. The porphyrin level is raised in faeces, urine (red) and calcified (dental) tissues.98 112 231 Root resorption has been reported.96
The “Swedish” variant, acute intermittent porphyria, a rare condition that includes mental retardation, peripheral neuropathy and acute respiratory paralysis, is probably due to decreased levels of uroporphyrinogen-I synthase. In such patients, use of substances such as ethanol, erythromycin, corticosteroids and some anaesthetic agents (lidocaine) is life-threatening.48
Dentine Dysplasia (DD) (pp. 86–8)
In type II DD, the crowns of the deciduous teeth show a translucent amber colour,334 and the permanent teeth may be grey or brown.280 In radicular type I DD yellow-brown319 and light blue-brown discoloration of the crowns is occasionally observed.225
Dentinogenesis Imperfecta (pp. 88–93)
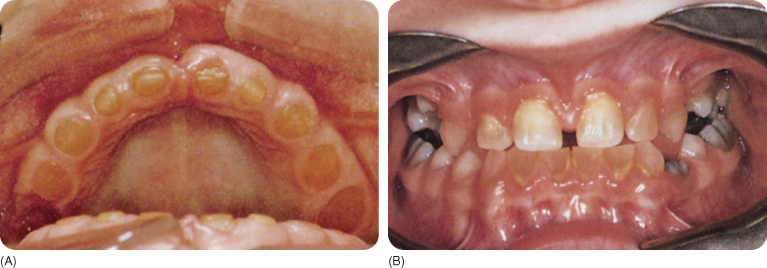
The crowns in type I and II dentinogenesis imperfecta are amber and opal coloured,319 but not all teeth are necessarily affected. Violet, red-brown, purple-brown,123 grey-blue305 and grey-green123 colours have been reported and such discolorations are caused by secondary deposition of minerals in the hypocalcified dentine (Figure 10.3). Ongoing rapid dentinogenesis with pulpal obliteration intensifies the stains.312 The enamel tends to chip away.
Figure 10.3 Dentinogenesis imperfecta. The anterior teeth are amber in colour (A) and the molars are somewhat blue (B).
(Courtesy of Department of Oral Surgery, University of Groningen.)
The grey or amber opalescent enamel in type III dentinogenesis imperfecta crumbles rapidly, exposing the shiny, amber dentine.178
Fluorosis (pp. 68–75)
Fluorotic enamel shows fine or merging white lines due to superficial porosities, which in more severe cases extend into the dentine. Very porous enamel breaks down, which causes pitting. Brown discoloration probably develops due to the post-eruption infiltration of the porosities by dietary pigments.270 The white and brown colours (Figure 10.4) might also be due to causes other than fluorosis, which are then diagnosed as “discoloration possibly associated with excessive fluoride”.79
Figure 10.4 (A) Fluorotic opacities in a deciduous dentition, (B) mild fluorosis, (C) opacities and brown discoloration, and (D) severe discoloration due to fluorosis with hypoplasia.

Haemolytic Anaemias
Haemolytic diseases of the newborn produce jaundice.
Erythroblastosis Fetalis (Rh Incompatibility) (pp. 56–7)
Mild neonatal jaundice is common, but jaundice can be severe in cases of rhesus incompatibility, which is diagnosed when the bilirubin concentration is 1.5 mg/100 mL in the serum. It is clinically visible at 7 mg/100 mL.171 The liver of the neonate is unable to process the large amounts of haemoglobin degradation products: the reddish yellow bilirubin of the destroyed erythrocytes is oxidised to the yellow-green biliverdin. Incorporation of these pigments in the calcifying dentine of the deciduous teeth is responsible for the discoloration that shows through the enamel if the concentration exceeds 30 mg/100 mL,386 which explains why not all affected children have discoloured teeth. A green (incorrectly named chlorodontia), yellow-green, blue, grey or brown hue is visible.271 374 The discoloration gradually disappears.171 Bilirubin might also be found within the enamel.98
Thalassaemia and Sickle Cell Anaemia (p. 58)
The erythrocytes are broken down in these hereditary diseases and the haemoglobin is released into the blood plasma. The circulating bilirubin is incorporated in the developing dentition and leading to grey discoloration of the permanent dentition in particular.160
The haemoglobin molecule consists of two α- and two β-globulin chains. In thalassaemias the production of the globulin chains is reduced.363 Sickle cell anaemia occurs in homozygotic carriers of the defective gene.
Maternal–Fetal ABO Incompatibility (p. 57)
Blood group incompatibility is accompanied with jaundice in the infant, but tooth discoloration has been only occasionally reported, including green (bilirubin)102 and black and grey stains.30 232
Transfusion Reaction Haemolysis
In this condition, the teeth are discoloured grey due to haemosiderin deposition.136
Hypophosphataemic Vitamin D-Resistant rickets (pp. 63–6) and Hypovitaminosis D (pp. 62–3)
In both these conditions, the (hypoplastic) enamel in affected children may be discoloured yellow and brown.
Inborn Metabolism Errors
Ochronosis (p. 58)
In this condition, abnormal phenylalanine degradation leads to blue-black discoloration of the permanent teeth, occasionally dark brown due to the presence of homogentisic acid.160 191 368 377
Primary Hyperoxaluria and Oxalosis (p. 188)
Hyperoxaluria is an inherited disorder of glyoxylate metabolism with renal failure. In oxalosis, oxalate crystals accumulate in extrarenal sites such as the muscles and skin,384 pulp and dentine, and initiate a foreign body reaction in the periodontal ligament, resulting in root resorption.254 384 Grey coloured teeth have also been reported.137 279
Phenylketonuria (p. 58)
Inhibition of the transformation of the amino acid phenylalanine (toxic to the brain) to tyrosine results in phenylalanine accumulation, which discolours the permanent teeth brown.
Infection and Trauma in the Deciduous Teeth (p. 79)
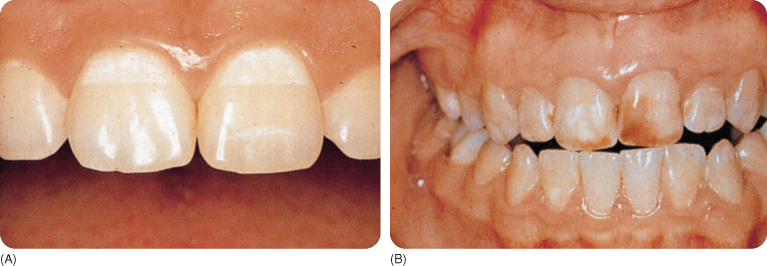
Periradicular pathology of the deciduous teeth after trauma or caries may disturb the developing enamel structure of the succedaneous teeth (occasionally with deposition of cementum on the enamel), which secondarily stain brown due to infiltration of dietary chromogenic pigments.129 White discolorations are seen in Turner teeth46 and yellow and brown discoloration also occurs (Figure 10.5).
Figure 10.5 (A) These opacities developed following (mild) trauma to the deciduous predecessors. (B) Brown discoloration, following possibly more severe trauma and/or infection in the predecessors.
Low Birthweight and Prematurely Born Children (p. 59)
The enamel may show yellow-brown bands.
Orotracheal Intubation (p. 57)
Children may have yellow-brown discoloured enamel on the side on which the tube was inserted.
(Pseudo)Hypoparathyroidism (p. 67)
Both hypoparathyroidism and a lack of response to parathormone are accompanied by hypoplastic yellow enamel.
Regional Odontodysplasia (ghost teeth, pp. 93–5)
If the teeth erupt, the (thin) enamel of the teeth is yellow to brown.
Syndromes
Enamel hypoplasia seen in many syndromes may resemble that seen in hereditary amelogenesis imperfecta. In tuberous sclerosis, small brown pits appear on the teeth. In the Crigler–Najjar syndrome, glucuronidation of bilirubin is absent, whereby the teeth become green to brown.98
Tetracyclines (pp. 75–7) and Ciprofloxacin
The earliest tetracyclines caused yellow discoloration of the teeth, which fluoresces under UV light. Tetracycline use in pregnancy or in children leads to discoloration of the children’s teeth. Due to oxidation under daylight, the yellow colour changes to brown (purple-red dentine).65 88 The posterior teeth, which are least exposed to light, remain yellow for longer. Use of other tetracyclines caused yellow, grey-brown, blue-grey, (brown-)yellow/ cream-white discolorations (Figure 10.6).
Figure 10.6 A–E Discoloration caused by different tetracyclines.

Three degrees of severity of tetracycline discoloration have been distinguished:
A fourth degree has been proposed,115 which is too dark a discoloration to attempt vital bleaching. In a sample of cystic fibrosis patients, 25% had tetracycline-discoloured teeth, mainly in the permanent dentition. About two-thirds of them had grey teeth, one-quarter had yellow teeth, and one-tenth had brown teeth.110
Later generations of tetracyclines are less discolouring, but the more severely discolouring earlier tetracyclines continued to be used in some countries. Severely affected dentitions are now mostly found in people older than 35 years. The new generation of tetracyclines (doxycycline (Vibramycin and Doxymycin)) only incidentally discolour the teeth and this is usually not severe. Minocycline (see Section 10.2.2) is an exception.
10.2.2 Endogenous Post-Eruption Discoloration
Endogenous post-eruption tooth discoloration occurs due to infiltration of the dental hard tissues by chromatic agents via the pulp, with the discoloured dentine showing through the enamel. A second category of causes includes dentinal sclerosis and pulpal obliteration.
(Capillary) Bleeding
Trauma to a newly erupted tooth may cause pulpal bleeding. A pinkish red colour shines through the enamel, becomes grey-blue within a few days, dark-grey after a few weeks, fading after 2–3 months once the pulp has healed and the blood products have been resorbed.12 153
In a sample of traumatised deciduous teeth, 15% (or less)173 showed transitory discoloration,41 and the rest remained grey: the pulp either became necrotic or was obliterated. The transient character of the discoloration has been questioned because all pulps in another sample of discoloured deciduous teeth showed irreversible pathological changes, including obliteration.331 Left untreated, the majority of discoloured deciduous teeth will function until their normal exfoliation time.283 328 Holan observed that about half of such teeth become lighter in colour. Infection was present when the teeth remained dark. In some dark teeth, root growth was arrested and in others inflammatory external root resorption developed. In the majority of the teeth that became lighter, the pulp was obliterated, which happened in only a few teeth that remained dark. Expansion of the dental follicle of the succedaneous tooth occurred in nearly all cases, which may signify a dentigerous cyst indicating the need to remove the deciduous tooth; the permanent tooth was deflected from its position and failed to continue erupting. 173
Drowning/Suffocation
Blood accumulating passively in the head because of a head-down position after drowning and, less likely, suffocation, leads to red discoloration of the teeth after some time (“pink teeth”): haemolytic derivates from pulpal blood penetrate the dentine. Exposure to sunlight changes the red colour to brown within a few days. In some archaeological material, such discoloration was absent.47
Lepromatous Leprosy
Leprosy is a chronic infectious disease affecting the nerves, skeleton and skin. Leprosy is classified into different types, based on clinical, bacteriological, immunological and histopathological criteria. Depending on the innate capacity of the host to mount a cellular reaction, at least three types are recognised: a malignant lepromatous type, a benign tuberculoid type and a dimorphous (mixed) type.304 In the lepromatous type, Mycobacterium leprae are abundant in the pulps and tubules, leading to discoloration of the incisors, which are reddish in about 10% to possibly one-third of the patients.52 304 The pulps often become necrotic. Premaxillary bone recession leads to loss of the anterior teeth in all types.288 304 333
Necrotic Pulp
A necrotic pulp causes progressive darkening of the dentine (Figure 10.7). The root is darker than the crown because the enamel partly masks the dark dentine.
- Following trauma (or application of excessive orthodontic force)157 erythrocyte breakdown products from the ruptured pulpal blood vessels penetrate the dentinal tubules.233 With time, the products become yellow-brown to blue-black. Iron from the erythrocytes forms a coloured compound with hydrogen sulfide. Formation of a haematoma prior to the breakdown of the erythrocytes may first give rise to light-pink discoloration. A similar discoloration develops after endodontic treatment of vital pulps when pulpal remnants are left behind.
- When the pulp became necrotic because of caries, blood will be absent. The grey-brown discoloration of the crown in such cases is caused by degradation of proteins (Figure 10.8).115
Figure 10.7 A dark non-vital tooth.

Figure 10.8 Brown discoloration (see text) in a non-vital tooth and amalgam discoloration of the first left maxillary premolar.

Pulpal Obliteration (Ageing and Trauma)
Ongoing dentinogenesis with age and dentine sclerosis make the crowns yellow and brown, respectively.98 179 249 327 Solheim reported the correlation between tooth yellowing and age to be 0.85 for the maxillary incisors and 0.6 for mandibular counterparts.327 An alternative explanation for yellowing of dentine with age is the incorporation of nitrogen and blood derivates into the tissue. Enamel, especially enamel cracks and lamellae, darkens also because of infiltration of dietary pigments (Figure 10.9).
Figure 10.9 Discolouring pigments infiltrate cracks in the enamel or the enamel lamellae.

After (sub)luxation, the pulp of deciduous teeth may be obliterated (partially or totally), causing a mild yellow discoloration.182 Andreasen reported partial and total obliteration in 15% and 1% of teeth, respectively, after periodontal trauma.11
Tetracycline and Other Antibiotics
Tetracycline products, when these drugs are administered to adults for extended periods, are incorporated in the secondary dentine and may slightly discolour the teeth.
Minocycline
Minocycline is used to treat severe inflammatory acne and systemic infections including atypical pneumonias and sexually transmitted diseases.354 It stains the bone and nail beds, breast milk (black colour), the lips (brown) and causes blue-black pigmentation (macules) of the tongue. Cutaneous hyperpigmentations have different colours and are divided into several types. Roots of erupted teeth become dark-green. Roots of extracted teeth exposed to the drugs during their development appear black.55 70 264 354 379 Brown-black minocycline pigment (spherical structures) has been observed within the oral mucosa overlying the hard palate,354 but the attached gingiva usually appears blackish-blue,55 116 due to the dark-green alveolar bone showing through.
Minocycline is completely absorbed in the gastrointestinal tract even when administered with dairy products. Once inside the tissues, the drug is oxidised and transformed into a coloured product. There are other theories of discoloration, such as chelation of iron by haemosiderin (a degradation product of minocycline), forming a melanin-like molecule.45 55 70 175
Minocycline is rapidly bound by plasma proteins and collagen binds minocycline to a significant degree, so that pigmentation occurs in tissues rich in collagen: scars, bones, teeth.45 Use of minocycline >100 mg daily leads to darkening of the crowns of already erupted teeth, to green-grey, grey, black, yellow or a striking blue-grey hue of the incisal three-quarters of the crowns, especially the middle third, fading incisally. The teeth are affected in only 3–6% of long-term users of the drug. Staining may already develop after 1 month and even 1 week of using the drug.45 55 63 65 142 175 266 354 379
Palliative treatment of rheumatoid arthritis and management of periodontal disease with minocycline may increase the prevalence of stained teeth in the future.55 175 354 379
Other Antibiotics
Staining following use of antibiotics such as amoxicillin has been reported a few times,93 but this is disputable. Ciprofloxacin, which is given intravenously to young children with Klebsiella pneumoniae infection, stains the teeth green.351
Typhus/Cholera
The pink discoloration seen in some typhus and cholera victims98 may be categorised as endogenous post-eruption discoloration.
10.3 Exogenous Discoloration
10.3.1 Exogenous-Infiltrative Discoloration
Exogenous-infiltrative discoloration of teeth is due to post-eruption penetration of the teeth by chromogenic agents from the environment (mouth). A filling in a tooth cavity and an endodontic filling in the pulp cavity are considered as belonging to the environment of the tooth.
Amalgam and Other Filling Materials
Radiographs sometimes show opaque areas underneath amalgam fillings.300 362 This is because metal ions from the corroding restorations, in particular stannic ions, penetrate the demineralised dentine and to a lesser degree the enamel.98 154 204 236 362 377 Besides stannic ions, some silver ions,377 as well as copper and mercury ions have been observed.236 308 330 Clinically, the tooth appears blue-black,98 sometimes green-black, and further away from the copper-containing amalgams it is green-brown.236 The opaque areas on the radiographs become larger with time236 due to ongoing infiltration by corrosion products. Contact with other metals worsens the corrosion,40 308 as well as with the non-γ-2 and copper-rich amalgams.6 282
Condensation may lead to pushing of amalgam components into the dentinal tubules,315 but metal ions may be displaced by galvanic action.236 Conventional amalgams may be less able to conduct electric currents than copper-containing amalgams.181
The layer of unfilled bonding agent between the enamel surface and the composite restorations may discolour brown after some time. A grey hue may develop around pins, and composite and glass ionomer cement fillings.
Diet
Infiltration of enamel by dietary pigments from foods and beverages – into the enamel lamellae, cracks, and carious and developmental opacities – and the exposed dentine cause a permanent brown discoloration of these tissues. The teeth of many older people also have accumulated brown-orange-yellow stains, leading to an unaesthetic appearance.68
Filling Materials in the Pulp Cavity
Tooth discoloration of various types (Table 10.2) has been reported within days to weeks of obturating the pulp cavity with an endodontic filling material; the discoloration becomes more severe with time.267 346 360 361
Table 10.2 Tooth discoloration produced by various endodontic cements/pastes
| Discoloration | Material |
| Brown-yellow | Iodoform paste |
| Grey (moderate discoloration) | AH26 (silver free), Duopercha |
| Light pink | Diaket, gutta-percha |
| Orange-red/yellow-brown | Grossman’s cement, zinc oxide-eugenol cement, N2, Tubli Seal, Endomethasone |
| Pinkish (later becomes dark red) | Riebler paste |
| Yellow-green (moderate discoloration) | Cavit |
Ions liberated by corrosion of a silver root canal post cause a grey-black discoloration.138 Use of Durelon, Fuji glass ionomer cement, Fletcher’s cement and zinc phosphate cement does not alter the tooth colour. IRM and Dycal make the teeth slightly darker.
Industrial Discoloration
Incorporation of air-borne dust particles and fumes of metallic salts causes characteristic discoloration of the teeth (Table 10.3).89 98
Table 10.3 Tooth discoloration due to exposure to various industrial chemical dusts
| Colour | Chemical |
| Black | Silver, iron, manganese |
| Grey | Mercury, lead |
| (Blue-)green | Copper, nickel, antimony |
| Orange | Chromic acid fumes |
| Bright yellow | Cadmium |
| Green, red, orange | Para-amino salicylic acid, copper, nickel |
Silver Nitrate and Silver Diamine Fluoride
Silver nitrate (AgNO3), which was used in the past to arrest dentine caries, resulted in an intense black discoloration.98 368
Below a superficial layer of the black precipitate, carious dentine is brown stained by free silver colloid. The deeper dentine and the pulp became black due to reduced silver globules. Sclerotic dentine remains stain-free,98 and the discoloration is well defined.236
Nowadays, application of silver diamine fluoride to carious tissue causes black discoloration of the dentine. Yellow silver phosphate is formed and turns black under sunlight.222
10.3.2 Exogenous Pseudo-Discolorations: Superficial Stains
Exogenous superficial pseudo-discoloration is due to adherence of environmental chromogenic agents to the salivary pellicle or plaque. Most cases of “tooth discoloration” are due to the coating of the tooth surface, i.e. pigments adhering to the pellicle (and plaque). The pigments originate from the diet, e.g. tea, coffee, wine, tobacco, etc., or are associated with cationic antiseptics and metal salts that interact with dietary chromogens and precipitate on the tooth surface.376 Some of the staining agents also penetrate the tooth tissues.
Indices have been developed to evaluate the colour, intensity and distribution of such stains.103 The stains have also been classified according to their origin, metallic or non-metallic,376 but neither the mechanism nor the variable extent of the stain, or the fact that not all metals stain the teeth, have been accounted for in these classifications. To overcome these problems, Nathoo classified extrinsic stains as follows:255
Betel Chewing (p. 209)
The betel nut is derived from the orange-red nut of the areca, arang, betel and pinang palms, and is wrapped in a fresh or fermented betel leaf coated with lime and sometimes tobacco or other ingredients.284 Betel chewing is widespread in southern Asia.385 It stains the lips, tongue and mucosa a mahogany brown, with a red-brown to black coating on the teeth (Figure 10.10). Oxidation of polyphenols (tannins and gallotannins) accounts for the red colour. Brown to black, complex polymeric end-products precipitate on the teeth.247 The rather thick layer has a tartar-like structure.285 Tooth wear is common. Frequent use leads to pathological, cancerous changes in the oral mucosa.284 313
Figure 10.10 Relatively mildly discoloured teeth in a person with a betel chewing habit.
(Courtesy of N.A.M. Rosema.)

In Thailand, many rural people are betel chewers, but most are older.287 In many other countries betel-chewing is also quite common. In the city of Kaohsiung in Taiwan, some 13% of men, mainly of low educational level, chew betel, although unawareness of the negative consequences has been reported.64 Among a sample of 16–18-year-old Taiwanese adolescents, 10% reported chewing betel and 31% reported doing so in the past.385
Calculus
Calculus is mineralised plaque, the calcium salts being derived from the salivary film which covers the plaque.
- The yellow-white supragingival calculus may become brown due to stains of dietary origin, smoking and so on. This calculus, in particular, is found on tooth surfaces near the orifices of the salivary glands, especially on the lingual surfaces of the mandibular anterior teeth and the buccal surfaces of the maxillary molars. Starting just above the gingiva, the calculus extends over the tooth surface.
- The brown to black (haemoglobin-derived) discoloured subgingival calculus may be visible through the gingiva. Compared with supragingival deposits, it is harder, more “stone”-like,224 more evenly distributed over the dentition and more firmly attached to irregularities in the root surface.224
The proportion of the population with calculus increases with age to some 80%. Dialysis patients have abundant calculus deposits due to their high salivary urea concentration. Use of some medicaments decreases the formation of calculus.224
Chlorhexidine and Other Mouthwashes
The brown-discolouring chlorhexidine (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


