Applied Surgical Anatomy of the Head and Neck
Because traumatic injuries disrupt the anatomy, the surgeon who is to repair and replace these traumatized structures must have an in-depth knowledge of normal anatomy. In addition, the operator must consider possible variations of normal and other associated structures that may be in close relationship to the traumatized area. Although numerous texts have been written on basic anatomy,1–11 it is thought that for completeness, this textbook should include a review of major head and neck anatomy. Details on specific problems and treatment modalities are found in the appropriate chapters. It is the intent of this chapter to discuss the general anatomy, its inherent relationships, and some technical problem areas that should be considered in the management of traumatic facial injuries.
Skin Lines and Lines of Langer
The natural skin lines and wrinkle lines are different from the lines of Langer, which denote the direction of the collagen fibers within the dermis. Langer believed that the skin was less extensible in the direction of the lines of tension that cross them.2,12 In the face, Langer’s lines have been shown to run across natural creases and flexion lines, thus making scars generated by incisions and trauma along those lines more noticeable. It is therefore recommended that elective incisions be made in or parallel to the lines of facial expression or the natural skin lines, when possible (Fig. 10-1).13 Skin wrinkles provide an excellent template for areas of relaxed skin tension. Old scar lines and hairlines can also direct a surgeon to the most appropriate placement of an incision. Considerations as the ethnicity of the patient must also be taken into account because hyperpigmentation and hypopigmentation issues might arise.
Scalp
The scalp is made up of five layers, three of which are closely bound together. These are the skin, dense connective tissue, and galea aponeurotica. Beneath these layers are the loose connective tissue and the periosteum or pericranial layer.1,6,8 The scalp bleeds freely because the vessels are bound firmly in the dense connective tissue layer (Fig. 10-2). This firm union and the extensive blood supply frequently make bleeding excessive and often difficult to control rapidly with hemostats. Pressure usually controls the open bleeders, and the rapid application of Raney’s clips controls full-thickness lacerations or elective incisions. Because of the nature of the loose connective tissue layer, dissection of the scalp is rather easy in this tissue plane. In a similar manner, however, the effusion of fluid spreads rapidly in this plane, leading to a boglike edema.

FIGURE 10-2 Layers of scalp. (From Aehlert B: Paramedic practice today, St. Louis, 2010, Mosby/JEMS.)
The innervation of the scalp comes from the trigeminal nerve anteriorly and laterally and from the cervical nerves (C2 and C3) posteriorly.1,4 If dissection is kept within the loose connective tissue layer, these nerves are avoided. In the supraorbital region, the superior orbital branch of the trigeminal nerve passes through a notch or foramen to innervate this area of the scalp. The supratrochlear nerve is located slightly medially and innervates the upper lid and the medial area of the forehead.14 Care should be taken when elevating flaps and managing lacerations in this area. As with most areas of the anatomy, when the skeleton makes angles or muscles insert, there is a denser attachment of the skin and soft tissue. In the scalp, this attachment is most notable in the glabella and supraorbital regions.
Skin of the Face
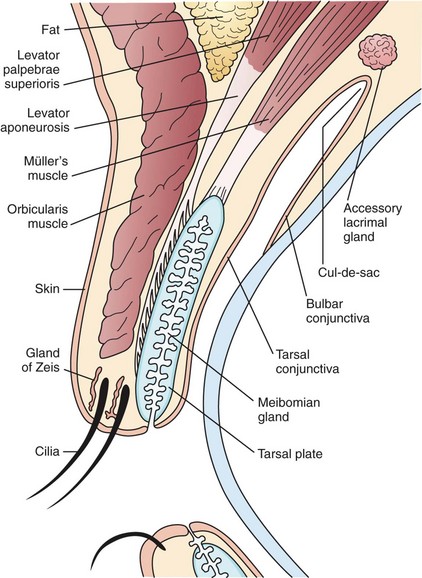
The skin of the face becomes specialized in the area of the eyelids, which are comprised of two structural lamellae: the external lamellae formed by the orbicularis muscle and its overlying skin and the internal lamellae of the tarsal plate and conjunctiva.15 The skin of the eyelid is extremely thin and delicate and contains small lacrimal, sweat, and sebaceous glands and hair follicles (Fig. 10-3).16
The skin of the nose is tightly attached to the lower lateral cartilage in the tip area. In other areas, the skin is less tightly adhered to the underlying infrastructure. The skin is thin in the nasal root and tip areas and thicker in the supratip region.4
Osteology
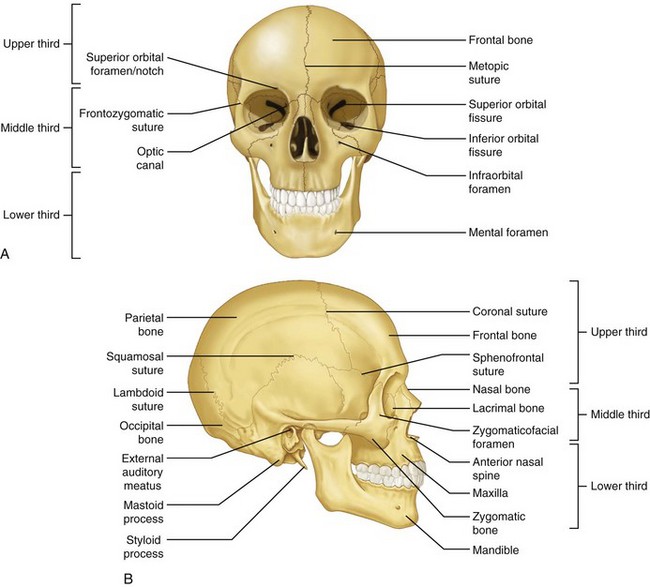
The bones will be considered in the traditional facial thirds (Fig. 10-4).3,5
Midface
The maxilla, zygoma, lacrimal, nasal, palatine, inferior nasal concha, and vomer bones are collectively referred to as the middle third of the facial skeleton.4,17,18 Although the sphenoid, frontal, and ethmoid bones are not classically facial skeleton bones, they are frequently traumatized in midfacial fractures and thus should be considered in the midfacial skeleton. The bones will be discussed separately, but their interconnections are of utmost importance.
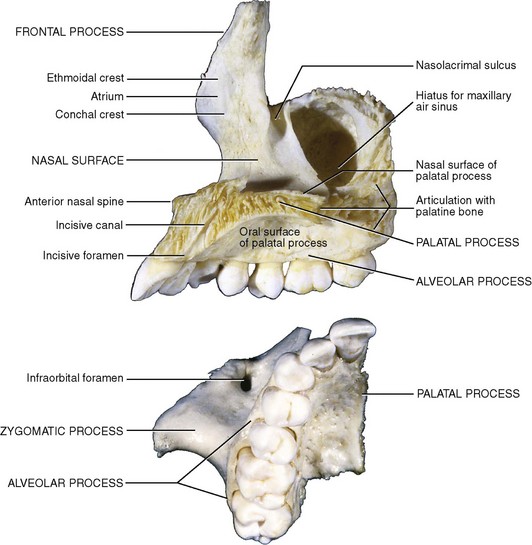
Maxilla
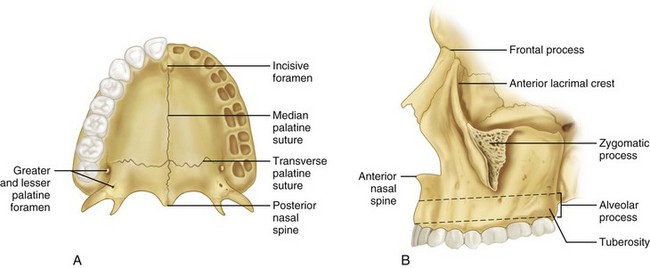
The maxilla (Figs. 10-5 and 10-6) is a paired bone of the upper jaw,* fused to form one bone, and is the central focus of the middle third of the face. Each hemimaxilla contains a large pyramid-shaped body, the maxillary sinus (antrum of Highmore), and four prominent processes—the frontal, alveolar, zygomatic, and palatine processes.
Zygoma
The zygoma (zygomatic bone, malar bone) is a paired bone that makes up the essence of the cheek prominence (Fig. 10-7; see also Fig. 10-4).* This thick, strong, diamond-shaped bone forms the lateral and anterior projections to the midface and is composed of four processes. The frontal process forms the lateral orbital wall and articulates with the frontal bone at the frontozygomatic suture. It is this articulation that is separated or rotated in isolated zygomatic fractures. The temporal process forms the zygomatic arch and articulates with the temporal bone. The maxillary process articulates with the maxilla to form the infraorbital rim and part of the floor of the orbit. Finally, the fourth process joins the maxilla on the lateral wall, producing the zygomatic eminence. This is an area of thickened bone that is usually available for fixation in the treatment of zygomaticomaxillary complex (ZMC) fractures. Along the crest of the zygoma, on the inferior aspect, is the insertion of the masseter muscle. The direction of force for this muscle is down and backward and its contraction contributes to displacement of the complex fracture of the zygoma, which may precipitate redisplacement in the improperly fixated fracture.

FIGURE 10-7 Zygoma (malar) showing articulations.
Surgical Note: The classic zygomaticomaxillary fracture (tripod, zygomaticomaxillary complex, and trimalar) involves this bone and its articulations. Details on the fracture and its management are found in Chapter 16. The options of surgical manipulation for reduction are discussed in the following sections.
Temporal Fossa Approach.
The Gillies approach is made via an incision in the hair-bearing area of the scalp, approximately 2 cm above and 1 cm anterior to the ear.14,20–23 This incision is carried down to the level of the temporalis fascia. The only structure of anatomic importance is the superficial temporal artery. This vessel courses across the area of the incision and can be identified through palpation and thus avoided by the properly placed incision. If it is encountered, it can be ligated and cut without complications. The temporalis fascia runs to the arch of the zygoma. An incision is made through this fascia to expose the muscle and develop a path for the passage of instruments to manipulate the zygoma. The main anatomic concern is being too superficial to the fascia, thus introducing the elevator lateral to the arch.
Lateral Brow Approach.
The lateral brow incision* is made to allow easy access to the frontozygomatic suture, because this area frequently requires open inspection, manipulation, and stabilization. Again, no major anatomic structures lie in close approximation. The incision is made full thickness to the bone, and the periosteum is reflected to expose the fracture. Generally, some form of elevator is placed posteriorly in the infratemporal fossa to aid in elevation of the fracture. Care should be taken not to lever against the temporal bone and displace any nondiagnosed, nondisplaced skull fractures. The incision is generally placed in the hair of the brow. The usual rule of making an incision perpendicular to the skin margin can be altered in this area because the incision should be made with the long axis of the hair follicle to prevent damaging the follicles, which could prevent the regrowth of hair. This hair should not be shaved for numerous reasons. The hair will grow back, but slowly, and it will be of a different texture and may often be sparse. The most notable problem is that of aligning the hair-bearing skin margins during suturing. If this is not performed properly, there will be an unsightly step in the brow when the hair does regrow.
Approaches to the Inferior Rim.
The multiple surgical approaches to the inferior rim† and articulation of the zygoma and maxilla are described in Chapter 16. These approaches provide access to the inferior orbital rim, orbital floor, lacrimal duct area and, in some cases, medial and lateral orbital walls. There are few anatomic problems if care is used to locate the layers of the inferior lid, most specifically the orbicularis oculi muscle, orbital septum, and inferior orbital rim. The approaches from the skin include the infraciliary incision and a lower incision through an existing skin crease. The infraciliary incision is aesthetically pleasing but may result in excessive and prolonged edema of the eyelid. The lateral extent of this incision, combined with the frequently needed lateral brow incision, compromises the lymphatic drainage of the lower lid. The skin is thin in this area and the skin flap must be developed carefully. The incision through the orbicularis oculi muscle is performed longitudinally to expose the inferior orbital rim. The incision through the periosteum should be on the facial aspect of the bone but above the infraorbital nerve.
Transoral Approach.
The floor of the orbit and infratemporal fossa can be approached through a buccal mucosa incision in the posterior maxillary vestibule.15,17–19 The eminence of the zygoma becomes available for stabilization via this approach. The maxillary sinus can be entered and the floor of the orbit, inferior rim, and eminence of the zygoma can be elevated from within. The infratemporal fossa can be entered posteriorly and superiorly, and the zygomatic arch and zygomatic body may be elevated. The buccal fat pad often interferes with visualization but is generally of no notable anatomic concern.
Transconjunctival Approach.
The final approach to the orbital floor is via the transconjunctival incision.5,14,21 Its only advantage is the avoidance of the slight facial scar from the infraciliary approaches. In the case of trauma, this is usually not a major factor. The incision is made through the conjunctiva at the lower border of the inferior tarsal plate, with the lower lid retracted inferiorly. A preseptal or retroseptal dissection can be made, although the preseptal dissection offers better control of the orbital fat. The approach to the orbital floor is otherwise the same and there are no notable anatomic problems associated with any of these approaches.
Nasal Bones
The nasal bones (Fig. 10-8; see also Fig. 10-4)1,2,4,6 are rectangular and articulate with the frontal bone superiorly and with each other at the midline. At the superior articulation, they are relatively thick, but inferiorly, they are much thinner. It is in this area that most fractures occur. The nasal bones articulate posteriorly with the frontal process of the maxilla.
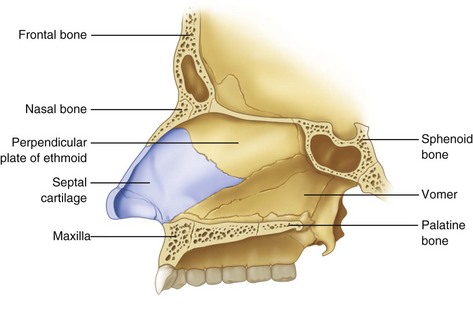
Ethmoid Bone
The ethmoid bone is an unpaired bone that is central to the facial structure (Fig. 10-9),* and it is an integral part of the nasal structure, to both orbits and to the anterior cranial base. The perpendicular plate forms the superior and anterior portions of the nasal septum and attaches to the cribriform plate. It articulates posteroinferiorly with the vomer and posterosuperiorly with the sphenoid bone.
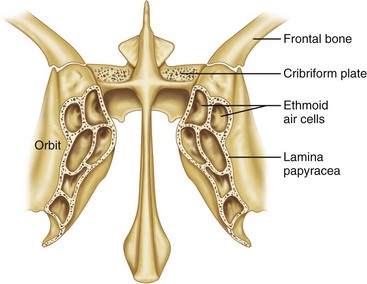
FIGURE 10-9 Frontal section of ethmoid bone.
Surgical Note: The thin lamina orbitalis may be fractured in blunt orbital trauma.11,15,17 The anterior ethmoid artery is a point for ligation as it passes from the orbital to the nasal aspect of the ethmoid bone. Because this artery is one of the terminal branches of the ophthalmic artery, which is a branch of the internal carotid artery, it is not affected by the usual measures to control facial bleeding and may require direct ligation via a medial canthal approach. The anterior ethmoid foramen is approximately 1.5 cm deep, measured from the medial orbital rim. Rarely is any surgical manipulation of this bone necessary or possible.
Vomer
The vomer (see Fig. 10-8)1,4,7 is a plow-shaped bone that is located in the midline of the nasal fossa and forms the posterior portion of the nasal septum. It articulates with the palatine, maxillary, and ethmoid bones and rarely is of notable concern in the primary management of facial trauma.
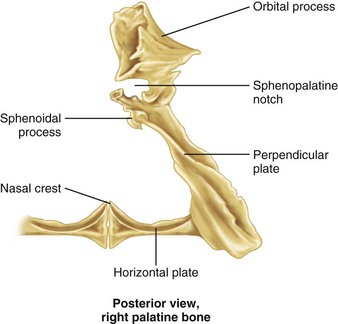
Palatine Bones
The paired palatine bones connect the maxilla with the sphenoid bone (Fig. 10-10; see also Figs. 10-5A and 10-6).1,2,4,5 This extremely irregularly shaped bone is composed of a major horizontal portion and vertical perpendicular plates. The horizontal plate articulates anteriorly with the maxilla and with the palatine bone of the opposite side in the midline to form the posterior aspect of the hard palate.
Surgical Note: Manipulation of the maxilla generally accomplishes adequate reduction of the palatine bones.8,17 It is important to remember the small contribution of the palatines to the orbital floor because extreme trauma to the maxilla and palate may cause some displacement or involvement of the orbital contents.
Inferior Nasal Concha
The inferior nasal concha is a paired bone2 that forms the bony support of the inferior turbinate bilaterally. It is of surgical importance only when it obstructs the inferior meatus and the nasal lacrimal duct.
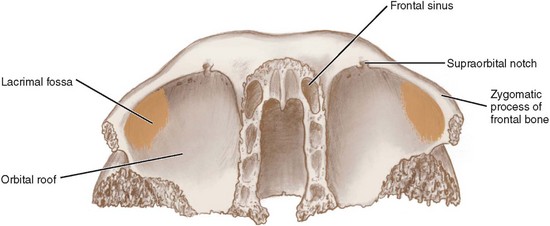
Frontal Bone
The frontal bone (Fig. 10-11; see also Fig. 10-4)* is a cranial bone that is unpaired and forms the anterior portion of the calvaria. The importance of this bone in facial trauma is its relationship to the anterior midfacial skeleton and the paranasal sinuses. The frontal bone articulates laterally with the zygoma and medially with the maxilla and nasal bones. Inferiorly and deep in the middle of the face, it articulates with the ethmoid and lacrimal bones and posteroinferiorly articulates with the wings of the sphenoid bone. The frontal bone articulates posterolaterally with the parietal bones.
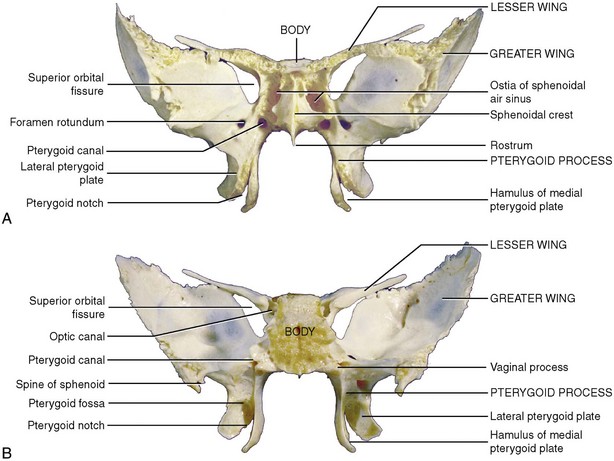
Sphenoid Bone
The sphenoid bone (Fig. 10-12)* is a single midline bone situated at the base of the skull that creates the anteroinferior extent of the cranial base and the posterior transition from facial bones to cranial bones. This complex bone has many processes that have delicate articulations with the adjacent cranial and facial bones.
Lower Face
Mandible
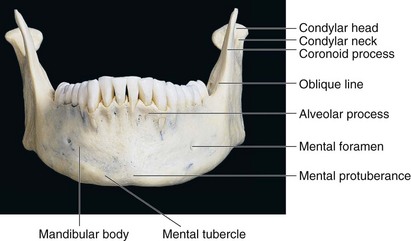
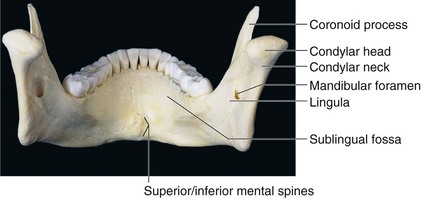
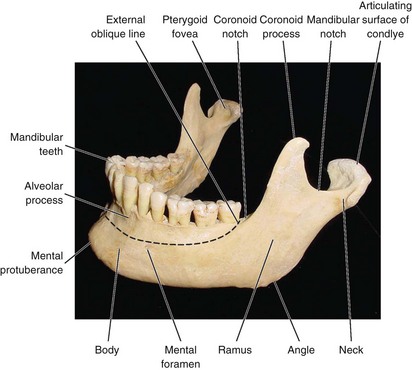
Despite the fact that the mandible (Figs. 10-13 to 10-15)* is the largest and strongest facial bone by virtue of its position on the face and its prominence, it is commonly fractured when maxillofacial trauma has been sustained. Mandibular fractures occur twice as often as midfacial fractures29,32; however, it has been shown in cadaver experiments that almost four times as much force is required to fracture the mandible versus the maxilla.30 The osteology of the mandible, various muscle attachments and their influence, and the presence of developing or completed dentition all play a notable role in producing inherent weaknesses. Therefore, fractures are seen more frequently in certain isolated areas.
The mandible is composed of the body and two rami, with their junction or angle forming the prominent gonion. The angle formed may vary between 110 and 140 degrees (mean, 125 degrees).15 The angle decreases slightly during growth because of changes in the condylar process, shape, and size. With aging, the angle becomes more obtuse.30 The body is U-shaped and has an external and internal cortical surface. The external cortical plate is thickest at the mental protuberance and in the region of the third molar. There is also a thickened triangular mental protuberance bounded laterally by the mental tubercles. The mental foramen is located on the external surface in the vicinity of the root apices of the first and second premolars. There are variations in the exact location of the foramen, as noted by Tebo and Telford.33 The opening is directed backward and laterally and transmits the mental nerves and vessels.18,34 The oblique line runs from just inferior to the mental foramen posteriorly and superiorly to the ascending ramus.
The mandibular notch is located on the superior edge of the ramus. It is bounded anteriorly by the coronoid process and its temporalis attachments, while also bound posteriorly by the neck and head of the mandibular condyle. A detailed description of condylar head anatomy is given later (see “Temporomandibular Joint”). Attached anteriorly to the neck of the condyle is the insertion of the lateral pterygoid muscle and attached laterally is the lateral ligament.
The strengths of the mandible are apparent when one evaluates the thick, round inferior border and the mental protuberance. The periodontal ligament and bone alveolus also combine with the trabecular pattern in the cancellous bone and are directed in a parallel fashion up the ramus to transmit pressures up to the condylar region.35,36 The thickening on the inner aspect of the condylar neck or crest of the neck apparently acts as a main buttress of the mandible as it transmits pressure to the temporomandibular joint (TMJ) and the base of the skull.29,32 The temporal crest runs from the coronoid process to the retromolar triangle distal to the terminal molar. The thickened posterior border of the mandible may act as an additional crest.28
Major structural forces are created at the angle of the mandible because of the cantilevered nature of its shape. The bone height at this angle is therefore critical in determining its strength and the presence of the perfectly aligned muscle sling created by the masseter and medial pterygoid muscles.37 Thus, aging, with its potential for bone and alveolar resorption, weakens this area.
Areas that exhibit weakness include the area lateral to the mental protuberance, mental foramen, mandibular angle, and condylar neck.29 If teeth are present, the socket is a weak zone, especially if teeth are impacted or unerupted. This would seem to indicate that a child in the mixed dentition stage may be highly susceptible; the fact that the child’s bones are so resilient and flexible offsets the disadvantage of the unerupted teeth.30
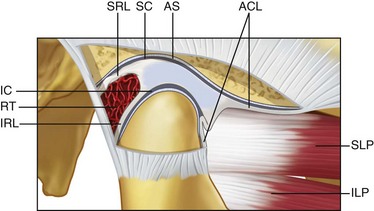
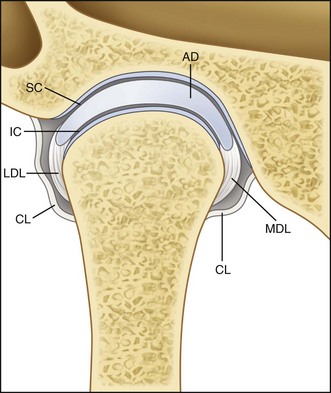
Temporomandibular Joint
The TMJ (Figs. 10-16 and 10-17)* is a freely movable synovial joint located between the glenoid fossa of the temporal bone and the head of the mandibular condyle below. The anatomic classification of the TMJ is a diarthrodial joint, with independent discontinuous movement between the two bones. An articular disc (meniscus) divides the joint into two cavities. The superior compartment permits hinge or rotational movement, whereas the inferior joint space permits translatory motion. The bony surfaces within the joint spaces are lined by synovial membrane, which is responsible for secreting synovial fluid that functions as nutritional support and a lubricating medium. This membrane is extremely thin, smooth, and highly vascular. Cells in the synovial membrane have the ability to differentiate into chondrocytes and provide the synovium’s ability to regenerate following injury. The articular surfaces of the joint and condyle and the central portion of the meniscus are composed of collagen. This feature differentiates this joint from most other articulations because the surfaces are not covered by hyaline cartilage. Histologically, this avascular fibrous tissue may contain cartilage cells and therefore may be termed fibrocartilage.10,17 This tissue has the ability to regenerate and to remodel under functional stress or following anatomic alteration, such as fracture.
The articular disc or meniscus, a dense fibrocartilaginous structure, histologically may show varying degrees and locations of cartilage cells.1 The meniscus is nonvascular and has no sensory innervation. When viewed from the lateral direction, there are three anatomic divisions or zones—the anterior band, intermediate zone, and posterior band. The thin intermediate or central zone corresponds to the functional area between the mandibular condyle and posterior slope of the articular eminence. When viewed from above, the meniscus is an oval biconcave structure that is thicker posteriorly. The posterior tissues are highly vascularized and innervated and are referred to as the bilaminar zone. The superior elastic fibers of the retrodiscal tissue attach to the tympanic plate and function to restrict anterior meniscus movement during extreme translation.43 The inferior fibers of the retrodiscal tissue are composed of collagen and attach to the articular surface of the condyle. They act as a check ligament to prevent extreme rotation of the meniscus during rotational movement of the mandible. The anterior attachment of the meniscus is contiguous with the lateral pterygoid muscle. The overall shape and size of the meniscus, therefore, vary depending on age, functional remodeling, and pathologic condition.
Mandibular Fracture Location
The mandible has various strengths and weaknesses, as noted.* The common sites of mandibular fracture, therefore, are the mandibular condyle region, mandibular angle region (especially in the presence of an impacted or semierupted third molar), mental foramen or body region, mandibular parasymphysis, and any component of the dental alveolus. In the very young and older patient with mandibular atrophy,30 other factors such as tooth buds developing in the child or a decrease in the cancellous-to-cortical ratio in older adults come into play. Because of the U shape of the mandible, eccentric forces often create bilateral fractures—one at the site of injury and the other contralaterally. Nahum36 has shown that forces in excess of 800 lb are required to fracture the symphysis and both condylar necks, and further demonstrated that the mandible is more sensitive to lateral impact than to impact from the front.
Anatomic Factors in Fracture Displacement
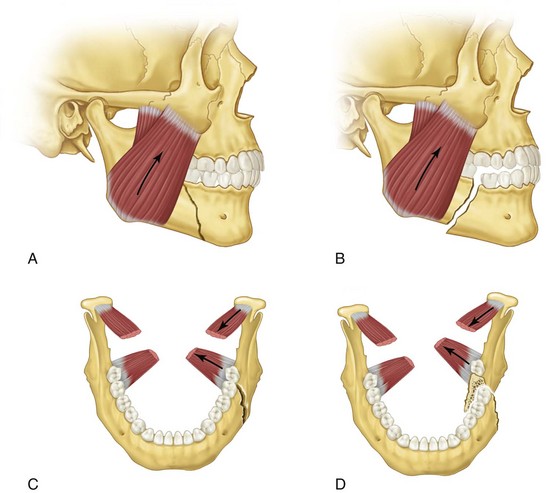
The direction of the causative blow, the direction of the line of fracture, and muscle pull all influence the amount and direction of bone displacement.† Muscle forces acting in the anterior region of the mandible, including those inserting in the mental region on the inner surface, are the geniohyoid, genioglossus, digastric, and mylohyoid muscles. These forces act to displace anterior segments inferiorly and posteriorly, with some possible medial component.13,41
The fracture angulation or direction of the mandibular angle and body region can vary. Depending on its orientation, muscle influence may be enhanced or prevented from actively displacing the proximal segment (Fig. 10-18). A fracture is regarded as favorable if it is in a downward and forward direction horizontally because of locking effects at the fracture site. If the horizontal direction is downward and posterior, the active pull of the posterior elevator muscles, such as the temporalis, masseter, medial pterygoid, and lateral pterygoid muscles, will displace the proximal segment superiorly. The vertical angulation of the fracture or bevel will inhibit the medial forces of the elevator group if the fracture direction is posterior and medial. This condition is regarded as vertically favorable. The opposite is true of the vertically unfavorable fracture traveling anteriorly and medially.
Mandibular Surgical Approaches
Mandibular surgical approaches are as follows (Fig. 10-19): extraoral approaches include the (1) Risdon, (2) condylar, and (3) symphysis approaches; intraoral approaches are the (1) angle and (2) mental or parasymphysis approaches.
Extraoral Surgical Approaches
An absolute description of various surgical procedures is possible in an elective situation. However, when dealing with a trauma patient, each approach is designed while taking into consideration the location of the injury, extent of the injury, method of stabilization to be used, possible coexisting soft tissue injuries, and potential anatomic factors.* The basic principles of making soft tissue incisions in natural skin folds may be more difficult to apply in the presence of severe edema and lacerations. In dealing with mandibular trauma in this section, the more common surgical approaches used for open reduction and exploration are discussed.
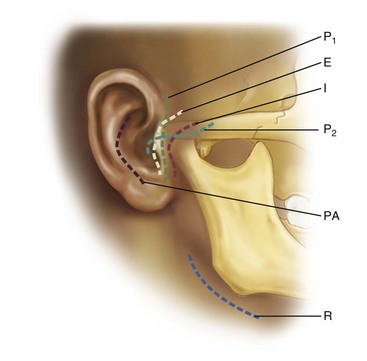
Preauricular and Condylar Approaches
Several soft tissue incision designs have been described, including the inverted L, as described by Blair,38 the T, as described by Wakely,46 and the endaural approach advocated by Lempert.47 Dingman and Moorman1 slightly modified Lempert’s approach and reported it in 1951. The facial nerve, when damaged, poses the most notable obstacle and potentially the most serious complications. A detailed description of the facial nerve appears later in this chapter (see “Facial Nerve”). Other anatomic structures that must be considered in the overall dissection in the preauricular approach include the parotid gland, superficial temporal vessels, and auriculotemporal nerves.
Risdon and Submandibular Approaches
During the procedures to reduce and stabilize mandibular angle fractures and, in some cases, low subcondylar fractures, some form of approach from the inferior mandible is required (Fig. 10-20). Parameters used to establish an incision include the following:
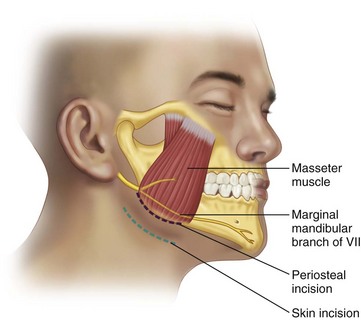
FIGURE 10-20 Risdon approach illustrat/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses