1
Pulp and Periradicular Pathways, Pathosis, and Closure
Mahmoud Torabinejad
Department of Endodontics, Loma Linda University School of Dentistry, USA
PULP AND PERIRADICULAR PATHWAYS
The root canal system and the periodontium communicate through natural and artificial (iatrogenic) pathways. The pulp tissue is encased in the root canal system, is surrounded by dentin, and communicates with the periodontium through the apical foramen and occasionally, small channels known as accessory or lateral canals. Iatrogenic pathways of communication between the root canal system and the periodontium are created during accidental procedures such as perforations during root canal treatment. In addition, removal of enamel and dentin by decay or by traumatic injuries as well as removal of cementum during periodontal treatment may result in communication between the root canal system, its dental pulp, and the periodontium.
NATURAL PATHWAYS
The natural pathways of communication between the root canal system and the periodontium include the apical foramen, lateral canals, and dentinal tubules.
Apical foramen
The apical openings of roots are the main pathways between the root canal system, its contents, and the periradicular tissues (cementum, periodontal ligament, and alveolar bone). The apical foramen is initially very large (Fig. 1.1). As tooth eruption and its formation continue, the root canal space is narrowed by apposition of dentin and the apical foramen is modified by cementum apposition (Fig. 1.2). Continuous passive eruption of the teeth and mesial drifting cause apposition of new layers of cementum at the root apices. As the tooth matures, the apical foramen is reduced in size. Single-rooted teeth usually have a single foramen. However, multi-rooted teeth often contain multiple foramina at each apex (Green 1956, 1960).
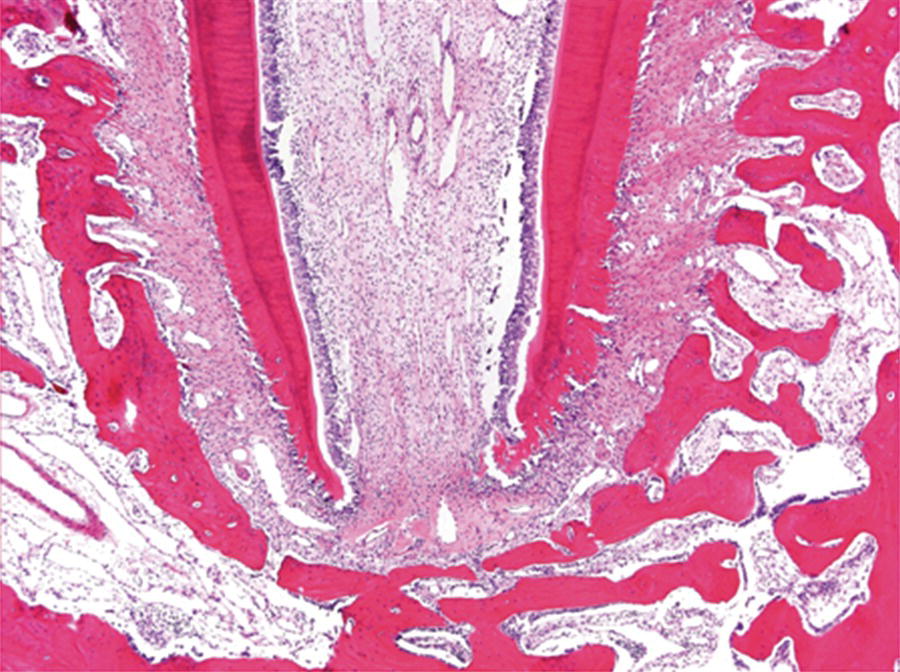
Fig. 1.1 Newly erupted teeth have large root canals with wide-open apices.
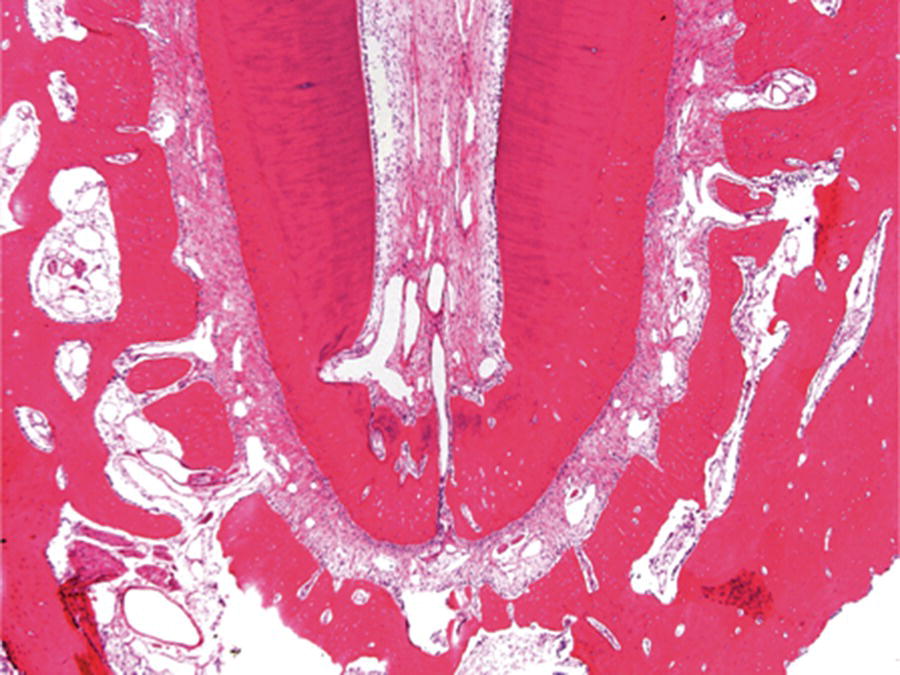
Fig. 1.2 As a tooth erupts, its root canal space is narrowed by apposition of dentin and its apical foramen is modified by cementum apposition.
Egress of irritants from pathologically involved necrotic pulps via the apical foramen into periapical tissues initiates and perpetuates an inflammatory response and its consequences, such as destruction of apical periodontal ligament and resorption of bone, cementum, and even dentin (Fig. 1.3).

Fig. 1.3 Egress of irritants through the apical foramen into periapical tissues initiates a periapical lesion and destruction of periradicular tissues.
Lateral canals
When the epithelial root sheath breaks down before the root dentin is formed, or the blood vessels that run between the dental papilla and dental sac persist, a direct contact may be established between the periodontal ligament and the dental pulp. This channel of communication is called a lateral or accessory canal. In general, lateral canals occur more frequently in posterior teeth than in anterior teeth and more frequently in the apical portions of roots than in their coronal segments (Hess 1925; Green 1955; Seltzer et al., 1963) (Fig. 1.4). The incidence of lateral canals in the furcation of multi-rooted teeth is reported to be as low as 2 to 3% and as high as 76.8% (Burch & Hulen 1974; De Deus 1975; Vertucci & Anthony 1986). Despite these variations, there is no doubt that a patent lateral canal can contain and carry toxic substances from the root canal system into the periodontium and induce periradicular inflammation.

Fig. 1.4 Presence of multiple lateral canals at the end of the mesiobuccal root of a maxillary first molar. Courtesy of Dr. John West.
Dentinal tubules
The dentinal tubules extend from the pulp to the dentinoenamel and cementodentinal junctions. The diameters of these tubules are approximately 2.5 µm near the pulp and about 1 µm at the dentinoenamel and cementodentinal junctions (Garberoglio & Brännström 1976). Although an actual count of the dentinal tubules has not been performed, their numbers are high, with approximately 15,000 dentinal tubules present in a square millimeter of dentin near the cementoenamel junction (Harrington 1979). The dentinal tubules contain tissue fluid, odontoblastic processes, and nerve fibers (Fig. 1.5). As the tooth ages or experiences irritation, these tubules tend to reduce in diameter or calcify, thus reducing patency. A continuous layer of cementum on the root surface is an effective barrier for the penetration of bacteria and their byproducts into the root canal system. Congenital absence of cementum, caries, or removal of the cementum during periodontal treatment or vigorous tooth-brushing may result in the opening of numerous patent small channels of communication between the pulp and the periodontium. Theoretically, these tubules could carry the toxic metabolites produced during pulpal or periodontal disease in both directions.
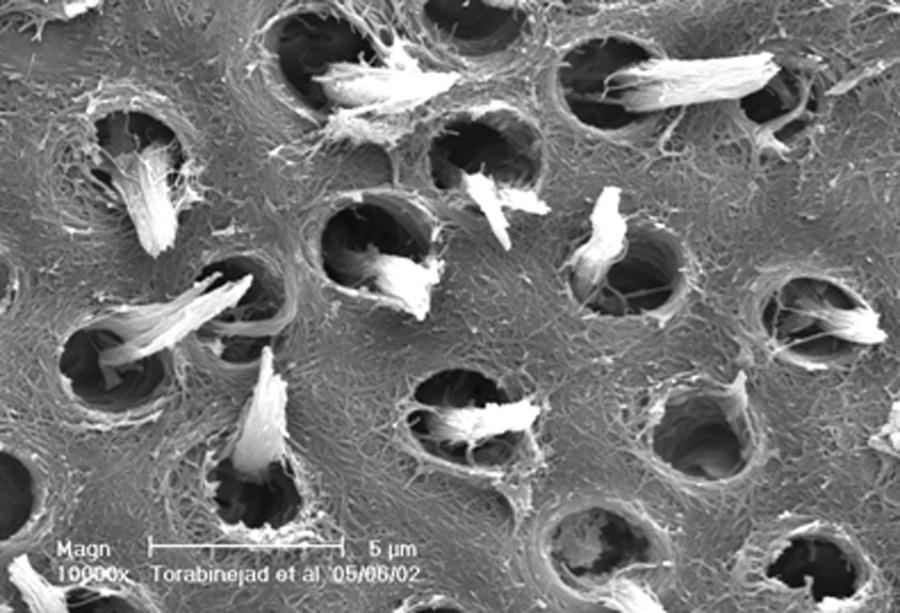
Fig. 1.5 An SEM picture of dentinal tubules containing odontoblastic processes.
PATHOLOGICAL AND IATROGENIC PATHWAYS
The pathological and iatrogenic pathways of communication between the root canal system and the oral cavity as well as the root canal system and the periodontium include carious pulp exposure, root perforation during access preparation, cleaning and shaping, post preparation and vertical fracture during obturation.
Dental caries
Carious dentin and enamel contain numerous species of bacteria such as Streptococcus mutans, lactobacilli, and actinomyces (McKay 1976). The presence of these microbes elicits toxins that penetrate through the dentinal tubules into the pulp. Studies have shown that even small lesions in the enamel are capable of attracting inflammatory cells into the pulp tissue (Brännström & Lind 1965; Baume 1970). As a result of the presence of microorganisms and their byproducts in dentin, the pulp tissue is infiltrated locally (at the base of tubules involved in the caries) by chronic inflammatory cells such as macrophages, lymphocytes, and plasma cells. As the decay progresses toward the pulp, the inflammatory process markedly changes in intensity and character (Fig. 1.6). Upon exposure, the pulp is infiltrated predominantly by polymorphonuclear (PMN) leukocytes to form an area of liquefaction necrosis at the site of pulp exposure (Lin & Langeland 1981). Bacteria can colonize in the area of liquefaction necrosis and persist. Pulpal tissue may stay inflamed for long periods before undergoing eventual necrosis, while in other instances the pulp may die quickly. Virulence of bacteria, host resistance, amount of circulation, and most importantly, the amount of drainage play a major role in this process.
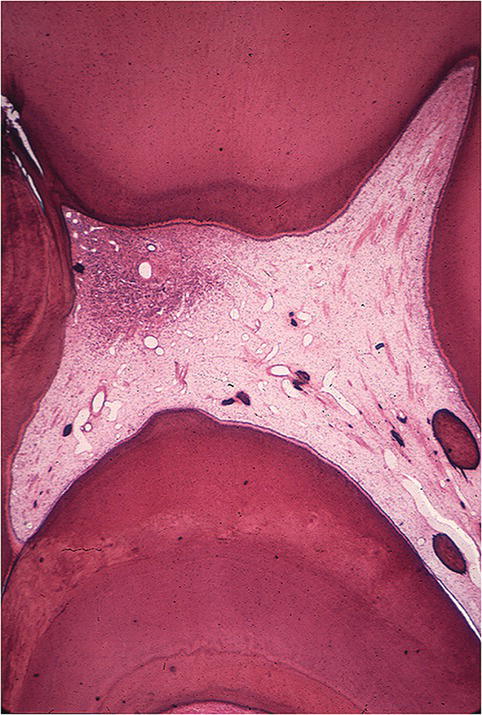
Fig. 1.6 Presence of severe inflammatory response at the site of carious exposure in a human molar.
Role of microorganisms
As a consequence of pulp exposure to the oral cavity, the root canal system acquires the ability to harbor bacteria and their byproducts. Because of its location, general lack of collateral circulation, and its low compliance (Van Hassel 1971; Heyeraas 1989), the pulp does not have the ability to defend itself against the invading bacteria. Sooner or later the bacterial infection will spread throughout the root canal system and the bacteria and/or bacterial byproducts will diffuse from the root canal into the periradicular tissues with resultant development of a periradicular lesion.
To show the importance of bacteria in pathogenesis of pulp and periradicular diseases, Kakehashi et al. (1966) exposed the dental pulps of conventional and germ-free rats to their oral flora. Pulpal and periapical lesions were developed in conventional rats. In contrast, they were absent in germ-free rats. (Fig. 1.7). Möller and associates (1981) sealed sterile and contaminated dental pulps in the root canals of monkeys. After 6–7 months, their clinical, radiographic, and histological examinations showed absence of any pathologic changes in the periapical tissues in teeth that had been sealed with sterile amputated pulps. In contrast, teeth sealed with infected pulps had developed inflammatory reactions in their periapical tissues. These studies show the importance of microorganisms in the pathogenesis of pulpal and periapical lesions.
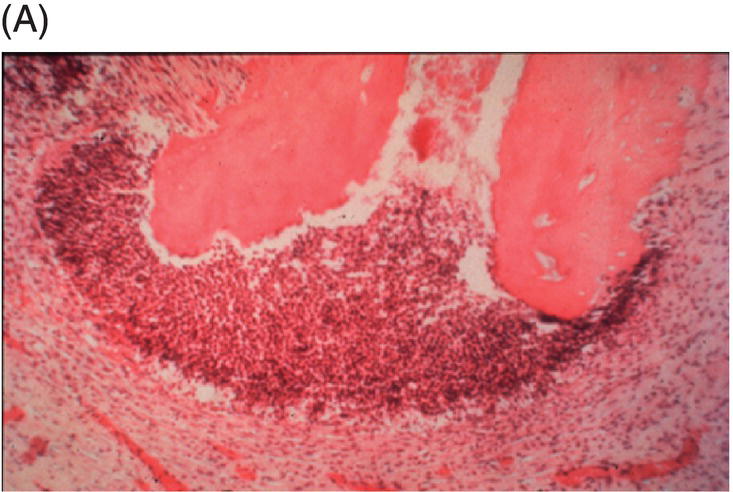

Fig. 1.7 (A) Presence of a periapical lesion in the molar of a rat exposed to bacteria present in its normal micro flora. (B) Absence of pulp and periapical pathosis in a molar of a germ-free rat exposed to its oral cavity.
Source: Kakehashi 1965. Reproduced with permission of Elsevier.
Root perforations
Roots may be perforated during access p/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


