Oral Cavity
• To describe the boundaries and sub-boundaries of the oral cavity and the structures in each area
• To define the terms vestibule, oral cavity proper, mucobuccal fold, frenum, alveolar mucosa, gingiva, exostoses, torus palatinus, and torus mandibularis
• To define the landmarks in the floor of the mouth and the hard and soft palate and the structures that form them
• To be able to tell the normal from the abnormal in the oral cavity and to ensure a follow-up examination
VESTIBULE
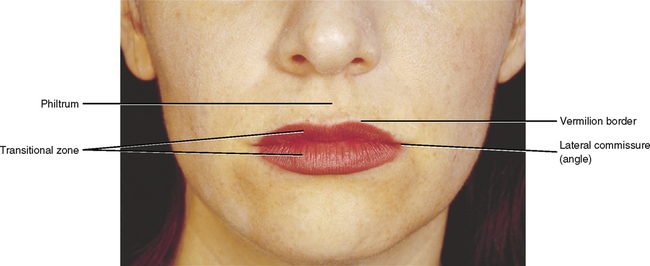
In considering the vestibular area, you should begin by examining the lips. The lips are the junction between the skin of the face, which is a dry tissue, and the mucosa of the oral cavity, which is a moist tissue. Between these two areas lies a transitional zone of reddish tissue known as the vermilion zone of the lip. It is along the border between the skin and the vermilion zone that one commonly encounters cold sores, which are generally caused by a herpesvirus. The skin of the upper lip has an indentation at the midline known as the philtrum, which is derived from the embryonic medial nasal processes (Fig. 1-1). It is at the lateral junction of this philtrum that a cleft lip might be formed.
Superior and Inferior Borders
The point at which the mucosa of the lips or cheeks turns to go toward the gingival or gum tissue is known as the mucobuccal fold or mucolabial fold. The mucosa lying against the alveolar bone is loosely attached and movable and known as alveolar mucosa. This mucosa is generally reddish because of the presence of blood vessels underneath the relatively thin mucosa. The point at which it becomes tightly attached to the bone is the beginning of the gingiva. This is known as the mucogingival junction (Fig. 1-2). The normal color of the gingiva is pink because the mucosal layer is thicker and therefore the blood vessels do not impart as much color. In patients with darker skin color, generally some pigmentation to the gingiva is evident.
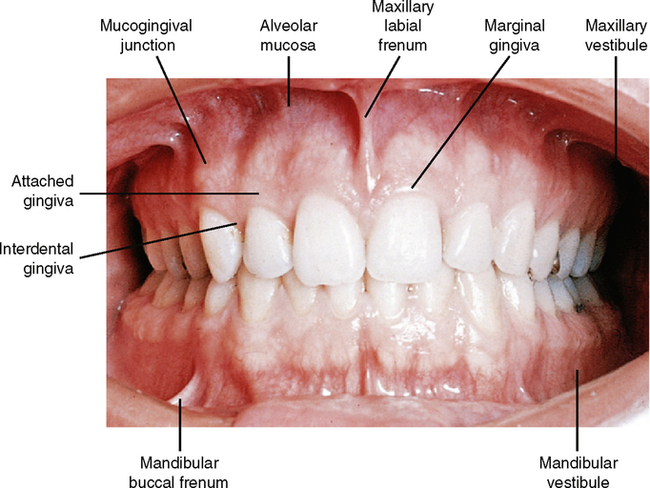
Pulling outward on the lips or corners of the mouth shows several areas where the tissue is attached in folds to the alveolar mucosa. At the midline in both the upper and lower lips, a fold of connective tissue known as the labial frenum can be found. The frenum contains no muscle tissue, only connective tissue. The upper frenum is usually more pronounced than the lower, but problems may occur with either one. The attachment of the upper (maxillary) frenum may extend to the crest of the alveolar ridge and even over the ridge. This band of tissue is so firm that the erupting central incisors might not penetrate it but may be pushed slightly aside so that a space exists between them. This space is known as a diastema (Fig. 1-3, A). Correction of a diastema usually involves the surgical removal, or cutting, of the frenum tissue between the teeth. After this the teeth will generally move together into normal contact. If they do not come back into normal contact, minor orthodontic treatment may be required. This procedure is best done when a child is 6 to 12 years old.
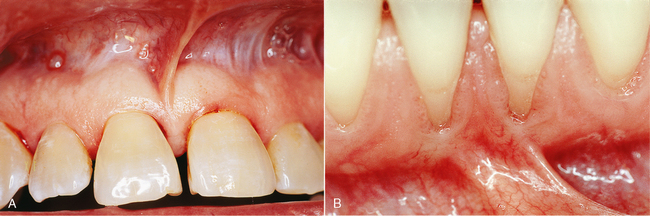
The mandibular labial frenum seldom extends up between the teeth, but it often extends close enough to the gingiva to contribute to gingival recession in that area by pulling downward on the tissue when the lip is tensed (Fig. 1-3, B). In this instance the frenum attachment needs to be incised with possible periodontal follow-up to restore the original gingival contours.
Less well-defined frena are evident in the maxillary and mandibular canine areas. These can be seen in Fig. 1-2 at the area labeled mucobuccal fold and in a similar area above it in the maxillary arch. Although these are not as well developed, they and the midline frena still have to be taken into consideration in the construction of a denture. If a groove is not reproduced in the flange, or edge, of the denture at that point, the appliance will cause irritation and possible ulceration of the frenular tissue.
Other Clinical Manifestations of the Vestibule
The coronoid process
Alveolar bone loss
Other problems arise in edentulous patients (see Figs. 26-12 and 26-15; dotted lines mark the alveolar process, or alveolar bone). When teeth are lost, some loss of the alveolar bone that formed the sockets for the teeth occurs. It tends to happen to a greater extent in the mandible than in the maxilla. If the bone loss is too great, problems occur in constructing a lower denture that will be stable. You will learn many ways to solve these problems as you progress in your studies.
Mucosa
Study the texture of the inner surface of the lip. Pull the lower lip down, dry it with a tissue and stretch it. Notice the small drops of fluid on the lip, indicating the openings of many small salivary glands. These of course are also found in many other areas of the oral cavity (see Chapter 25).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


