CHAPTER 1
INTRODUCTION TO SALIVARY GLAND LESIONS CYTOLOGY
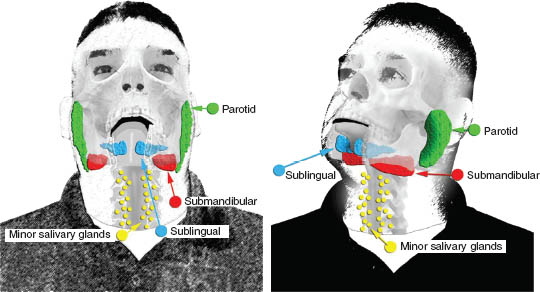
The salivary glands are part of the exocrine secretory apparatus that are traditionally considered part of the upper gastrointestinal tract. They are a very small organ with an average total weight of 50 g in adults compared with other systems. They are composed of two major groups: the major and minor salivary glands. The major glands are composed of three paired relatively larger glands: the parotid, submandibular, and sublingual. The minor group is numerous and widely distributed in the upper aerodigestive tract (Figure 1.1).
FIGURE 1.1. A diagram showing the general anatomy of salivary glands. The major salivary glands are composed of three paired, relatively larger glands: the parotid, submandibular, and sublingual. The minor salivary gland groups are numerous and widely distributed in and around the upper aerodigestive tract and are predominantly in the submucosal areas.
1.2 BASIC HISTOLOGY AND PHYSIOLOGY
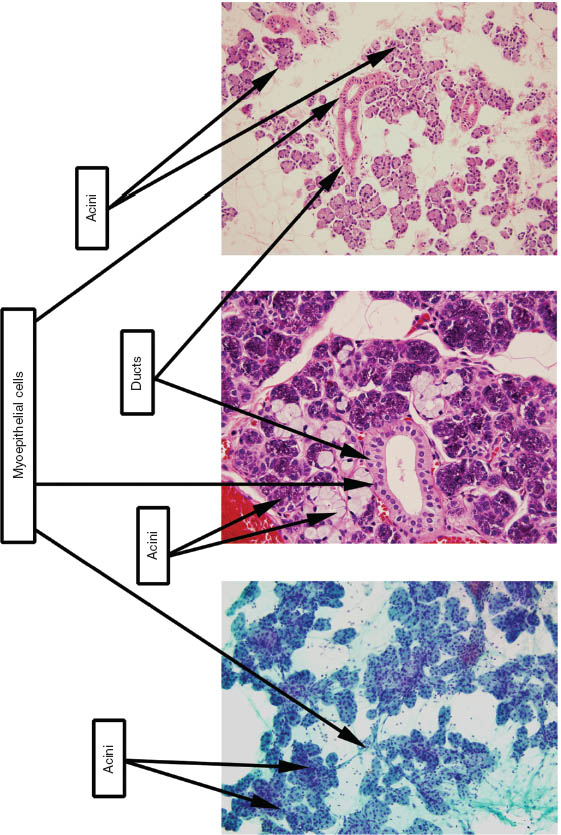
Salivary glands secrete digestive enzymes from their main functional unit “the acinus.” The major histological components of salivary glands are as follows (Figure 1.2 illustrates these components and their cytological correlates):
1. Acinus: The main functional unit that is composed of wedge-shaped cells, each with abundant cytoplasm pushing a small round-to-oval nucleus to its periphery. They can be serous where they mainly secrete amylase, and their cytoplasm appears basophilic and densely granular with zymogen granules. These granules are periodic acid Schiff positive and diastase resistant. The mucinous acini secrete sialomucin, and their cytoplasm appears clear with vacuoles. The parotid gland is almost purely serous, whereas both the submandibular and the sublingual are mixed. The submandibular is more serous, and the sublingual is more mucinous.
2. Ducts: They start as small, intercalated ductules between acinar cells that are lined by single, small cuboidal cells with relatively large, centrally located nuclei. These are difficult to see on histological sections. These ductules will then join and form larger, striated ducts lined by taller columnar cells with much more abundant and eosinophilic cytoplasm rich in mitochondria. These in turn will join larger interlobar excretory ducts lined by pseudo-stratified columnar epithelium with similar features.
3. Myoepithelial cells: These stellate-shaped cells are contractile and are located outside the basement membrane of the acinar cells. They contain smooth muscle actin, myosin, and intermediate filaments such as keratin. They are difficult to see histologically.
FIGURE 1.2. The three images were combined to show the three major cellular components of salivary glands. The left image is from an aspirate smear (Papanicolaou stain, 200×); the middle image is the corresponding histological section (hematoxylin and eosin, 400×); and the right image is from a cell block (hematoxylin and eosin, 200×).
1.3 DISEASES THAT AFFECT SALIVARY GLANDS
Many diseases can affect salivary glands. The common entities range from inflammatory/infectious non-neoplastic lesions, benign neoplasms, and malignant tumors. With an active otolaryngology service, pathologists are frequently asked to perform or interpret fine needle aspirates from salivary gland masses. Most mass lesions suspected to develop from salivary glands pose diagnostic challenges and are aspirated to determine the underlying disease process. Masses of the parotid gland are the most frequent. In these circumstances, the major questions that face pathologists are summarized in Table 1.1. Chapter 2 was written by an oncologic otolaryngology surgeon (Dr. Tulunay-Ugur) and clearly illustrates the preoperative approach of these tumors and lesions and what the surgeon would like to see in the fine needle aspiration report.
TABLE 1.1. Questions to be answered when evaluating aspirates from salivary gland masses
| 1. Is the lesion a salivary gland lesion? |
| 2. Is the lesion neoplastic? |
| 3. If neoplastic, is it benign or malignant? |
| 4. If malignant, is it high grade or low grade? |
| 5. Can the diagnosis be specific? |
1.4 EPIDEMIOLOGY OF SALIVARY GLAND TUMORS
Despite its small size, tumors of the salivary glands are numerous and they characteristically exhibit a relatively significant degree of overlap on both morphologic and cytologic grounds. The most recent World Health Organization (WHO) list of primary tumors included 10 benign epithelial tumors, 24 malignant epithelial tumors, 1 soft tissue benign tumor (hemangioma), and lymphomas (Table 1.2). Secondary and metastatic tumors can occur, but they are less frequent and most are secondary to other head and neck neoplasms. Benign tumors are much more common than malignant ones, and the parotid gland is the most frequently involved. In addition, it is well known that the relative frequency of malignancy is inversely proportional to gland size. Therefore, malignant tumors approximately comprise 25% of parotid gland tumors, 45% of submandibular gland tumors, 80% of sublingual tumors, and 50% of minor salivary gland tumors. Therefore, extra attention has to be paid to the salient features of malignancy on cytological grounds when dealing with sublingual and minor salivary gland masses. Most tumors that occur in the floor of the mouth, the tongue, and the retro molar areas are essentially malignant. There are well-known geographic variations and gender disparities. However, these will be tackled in the following chapters. In the United States, malignancies of salivary glands comprise approximately 6% of all head and neck cancers and less than 1% of all maligna/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


