CHAPTER 1
Introduction: Begin with Stability in Mind
“We are what we repeatedly do. Excellence, then, is not an act, but a habit.”
–Aristotle
Orthodontics has been a creditable specialty within dentistry for more than 100 years. And yet, after all these years and millions of patients treated, universal guidelines that can be taught and practiced on a daily routine have not been established. The phrase “begin with the end in mind” is well and good if we know where the end should be. A phrase better suited to this book is “begin with stability in mind.”
For many years, the world of orthodontics has been searching for the “golden horseshoe” when addressing the subject of long-term stability. So many factors must be included: growth, habits, treatment technique, application of forces, and compliance. Webster’s New World Dictionary defines stable as “not likely to change” and “firm, fixed, lasting.” When this subject is related to entities in the oral cavity, especially the teeth, is it realistic to think that they can remain firm and last throughout a patient’s life? Several variables exist, including eruption patterns, eruption direction, skeletal pattern, musculature, and habits, many of which cannot be controlled by the orthodontist throughout the patient’s life. Dr Little arbitrarily stated that any occlusion with less than a 3-mm irregularity index can be considered stable.1
The reality is that we are not dealing with teeth set in concrete. Perfection is not a realistic goal. Living hard and soft tissues place pressures on the teeth that can cause changes and movement. Our challenge is to find certain positions in which the teeth can be placed in the oral cavity so that the balancing intraoral forces will allow the teeth to be firm and lasting.
After all this time, are we as a specialty in orthodontics any closer to identifying the keys that are necessary to achieve adequate functional occlusion, acceptable esthetics, and stability? Historically, by not learning from our past mistakes, the pendulum has swung from nonextraction to extraction and then back to nonextraction.
Currently in the world of orthodontics, fantastic technology and new and different ways of viewing mechanics, such as cone beam imaging and controlling vertical anchorage with mini-implants, have shown great promise. But few things in life come without a price. The question is: Are we smart enough to know who has control of what? And is it worth the price?
In reading the history of the Roman Empire, one is amazed by the advanced technology the Romans created in the construction of their roads. During that special time in history, literally all roads did lead to Rome. In the world of orthodontics, wouldn’t it be wonderful if we had a Rome? No matter our technique or bracket system, our goals for the finished result would be the same, and we could expect good long-term stability. Yet there is currently no Rome in orthodontics. If I were to pass the diagnostic records of a particular patient around a room full of orthodontists and ask for a treatment plan, there is no question that I would receive a multitude of opinions. This sad scenario confirms the fact that orthodontics in general is still too much an art and not enough a science. The patient’s treatment results have a direct relationship to the clinician’s knowledge, manual dexterity, philosophy, and, most of all, effort.
For those orthodontists who lecture, showing difficult but beautifully treated patients is an exciting and rewarding experience. The audience members show their approval, and all are impressed. Such an example is Case 1-1.
The problem with such presentations is that they are anecdotal—“based on or consisting of reports or observations that are usually unscientific in nature”—especially if only one case shows nice results. But what about 10 to 20 or even 30 consecutively treated cases that show good results and long-term stability? One must ask: What was performed differently that enabled the long-term stability?
Much of this book is devoted to the display of a multitude of patients who had diagnostic records taken at the beginning of treatment, end of treatment, and many years posttreatment. The long-term records vary from 5 to 40 years posttreatment.
Each case is evaluated according to its diagnosis, treatment plan, and long-term stability in relationship to certain guidelines. These patients include malocclusions with mixed dentition (Case 1-2) and adult dentition as well as extraction and nonextraction cases.
In a February 2007 editorial in the American Journal of Orthodontics and Dentofacial Orthopedics, editor David Turpin addressed the issues of stability and treatment guidelines2p159:
As a specialty, it is time to ask these questions. Do we know how to predict, prevent, manage, and treat malocclusions, with all their manifestations, efficiently and with the best possible outcomes? If the answer is yes, based on the best available evidence, is it appropriate to write guidelines for the management and correction of malocclusions?
Realistically, ours might be the only specialty in dentistry that has not already produced guidelines. Are we as a specialty ready to begin the long process of writing guidelines for the management and correction of malocclusions? Orthodontic guidelines can be found now on various websites, but these guidelines were not written or endorsed by the American Association of Orthodontists! Now where do you stand on this issue?
The present author responded to this editorial, thanking the editor for addressing such an important subject:
Our forefathers in orthodontics taught us many things about treatment and stability. Dr Tweed might have been the first to actually state guidelines for treatment planning, using the Tweed Triangle as the diagnostic goal. Fifty years later, where are we in regard to having guidelines that most orthodontists can accept? It is sad to say that we might be farther away from a consensus now than back in Tweed’s days.
Over the last few decades, one of my orthodontic missions has been to establish certain guidelines for our patients that can routinely produce functional, esthetic, and stable results. These guidelines are based on many research studies with our patients.3–11
The bottom line is that research shows us that there are certain guidelines that, when followed, can be used to create the best result for that patient. Of course, there are exceptions to every rule, but I hope that creating guidelines is a start in the right direction.
The purpose of this book is to recognize and identify guidelines that will place the teeth in particular positions that will produce the healthiest, most functional, most esthetic, and most stable results possible. Are there not fundamental requirements we can all agree on? It has been said that the more things change, the more they stay the same. Hopefully, this book will help you understand and clarify that which is really critical to produce long-term stability with your patients.
The Greek philosopher Socrates is given credit for making this very poignant statement: “Nothing is really new … we just discover for ourselves.” Shortly after entering private practice, I was invited to become a clinical associate professor in the Baylor Orthodontic Department. Most of the students were older than I and had little respect for one who was just finishing his first cases. During those early years of spending every Friday morning in the Baylor Orthodontic Clinic in Dallas, I would spend my long drive back to Arlington searching my mind for answers to the students’ questions. I can remember telling myself that if I was going to continue teaching, I must find better answers than “that is what I was taught.”
Significant influences in those early years included my older brother C. Moody, the West Texas Orthodontic Study Group, classmate Robert Orr, the Texas Orthodontic Study Club, and, especially, our local study club. Each month this group met, and its members challenged one another on all aspects of orthodontics. I am forever grateful to Jim Boley, Bill Robinson, Bob Harris, Bob Stringfellow, and Gib Robertson for making me either think and defend my beliefs or change them. Therefore, in those early years, and throughout my career, I have continued to discover for myself.
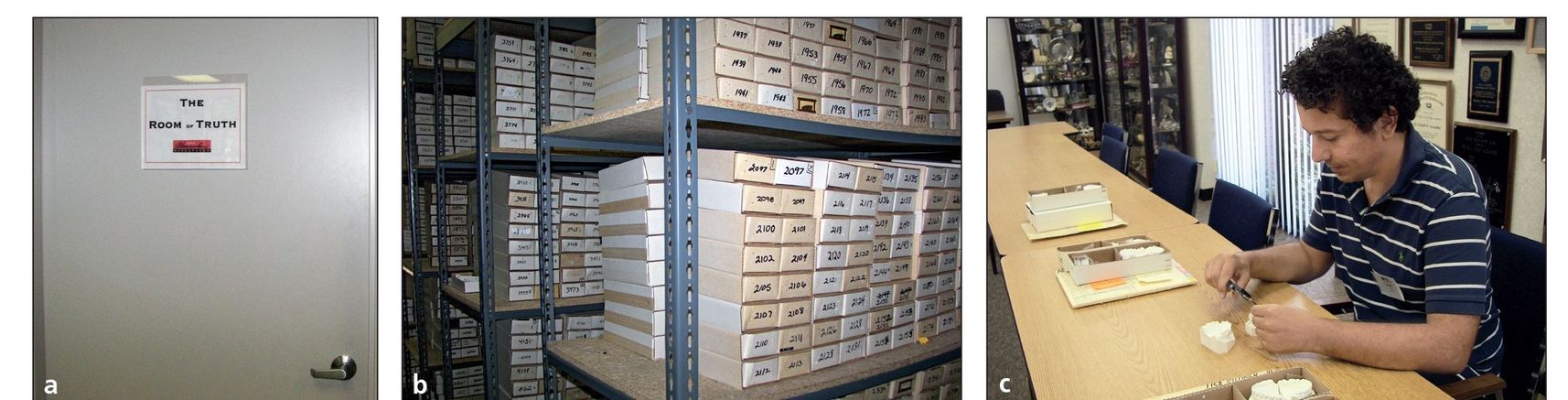
Fig 1-1 (a) The door to the Room of Truth. (b) Diagnostic records inside the Room of Truth. (c) Italian orthodontic graduate student Dr Aldo Coli studying diagnostic records in the Room of Truth.
The great American poet Robert Frost, in evaluating his life, wrote that “Two roads diverged in a wood, and I—I took the one less traveled by, And that has made all the difference.” In evaluating my own journey in orthodontics, I sometimes ask myself if I chose the right road. The answer is yes, but only after taking occasional detours. Early on, I discovered what not to do, but it took years of trial and error to choose the better paths to develop my orthodontic technique.
Experience has taught us certain truths about where and how best to place the teeth. These facts cannot be disputed. They might be ignored, but they cannot be disputed. For the private practitioner, it can be difficult to resist the urge to compromise. The challenge before us is to apply new technology to create results that good science has already proven.
The benchmarks have now been established. Until science changes these benchmarks, isn’t it our responsibility as professionals to strive to achieve them? By combining knowledge from our forefathers, clinical experience, and research, specific guidelines can be followed to consistently produce quality, stable results.
The Room of Truth
After a few years in practice, almost every orthodontist has the problem of storing patients’ diagnostic records. In addition to the growing amount of space required, there is also an added burden of finding time to take these final records. With the combination of time, space, and cost involved, virtually all orthodontists stop taking final records as they become busy.
Certain advantages regarding records evolved early in my professional career without my realizing it. In graduate school, we were all taught to take complete pretreatment and posttreatment diagnostic records. Upon entering private practice, because I was teaching, I continued this sequence, and I have continued it to this day. More than 15,000 patients have been treated in our office, and we have full initial and final records for at least 10,000 of them.
One of the few advantages of my age is that many patients I treated years ago have since brought their children in for treatment. When we discover this former relationship, the first thing our staff does is to look into the Room of Truth (Figs 1-1a and 1-1b). This is the room where many of these records are stored. If we have complete records on the parent, we ask to take new postretention records. We have about 300 to 400 of these T3 records (postretention), and the number is growing monthly.
From this room, more than 50 master theses have been written. The majority of students have come from Baylor, but other schools include the University of Texas, University of Alabama, University of Southern California, New York Univeristy, Loyola University, and other schools in Canada, Germany, Mexico, Brazil, and other countries. A large number of these theses have been published. An open-door policy concerning these records has always been in force. Any student in the world is welcome to come study these diagnostic records (Fig 1-1c). The only stipulation is that no records be removed from the office.
Throughout this book, I quote many statements from these research studies that changed some of our concepts on long-term stability from anecdotal to evidence-based information.
In volume one of this series, I attempted to identify the 15 keys to orthodontic stability. Although the keys have not changed, I have consolidated them into six guidelines. Hopefully this book presents to the reader a more precise approach to identifying the goals for long-term stability.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


