CHAPTER 3
Special Considerations in Orthodontics
“The direction in which education starts a person will determine his future life.”
—Plato
Periodontal Considerations
Although debate surrounds the question of which factors influence the stability of orthodontic results, there is one factor for which there is no debate: periodontal health. Periodontal research has shown us that plaque control is the most essential element in maintaining the health of the teeth throughout one’s lifetime. Without healthy teeth, long-term stability is not a realistic goal
Theoretically, teeth and periodontal tissues will last a lifetime if the tissues are periodontally plaque free, regardless of the patient’s occlusion or function. Although deep bite malocclusion and bruxism can cause dental attrition and eventually soft tissue recession, regardless of the high quality of the finished occlusion, there will be no long-term health of the teeth if the patient does not have good oral hygiene (Fig 3-1). If a person has perfectly straight teeth but horrible plaque control, early periodontitis, gingival inflammation, gingival recession (from poor brushing techniques), periodontal bone loss, and eventual tooth loss are inevitable.
Therefore, one of the greatest opportunities afforded the orthodontist is to educate the patient regarding excellent oral hygiene and to reinforce this education during each routine visit. If good oral hygiene habits can be instilled at a young age during orthodontic treatment, then lifelong dental health is a real possibility.

Fig 3-1 A patient with poor oral hygiene. (a to c) Intraoral views. (d and e) Occlusal views.
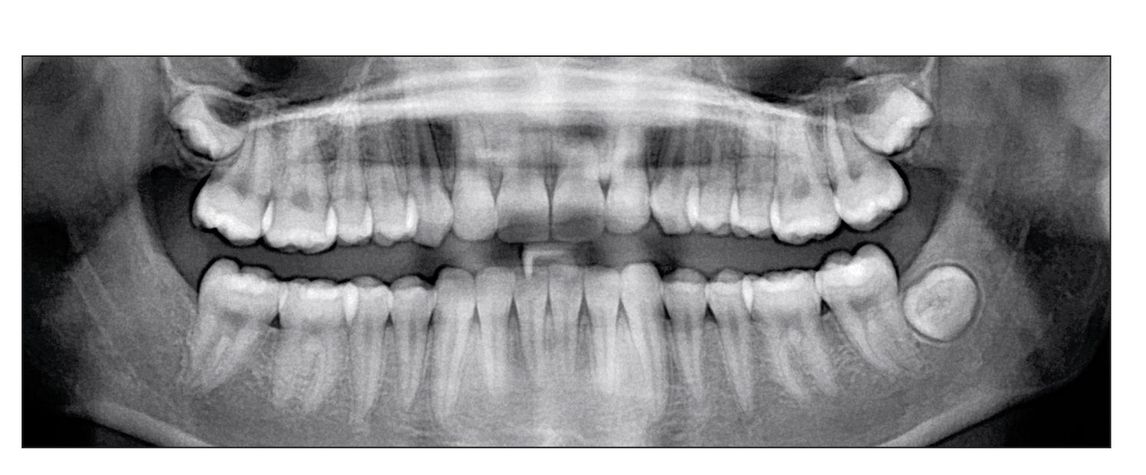
Fig 3-2 Panoramic radiograph showing root resorption.
Potential periodontal problems during orthodontic treatment
The most common periodontal problem that develops during orthodontic treatment is gingivitis. This condition is the result of a buildup of plaque and calculus that forms because of the patient’s inability to keep his or her teeth clean while orthodontic appliances are present. The acid-etching technique used in bonding can also cause irritation of the gingival tissue if proper care is not taken. A longstanding gingivitis can develop into soft tissue hyperplasia while the patient is wearing the orthodontic appliances. Other iatrogenic causes of periodontal problems could include the improper fitting of bands around the teeth, excessive cement not being cleaned properly, and elastic wear causing pressure on the tissue. Periodontal abscesses can form as a result of poorly fitting appliances or unclean areas surrounding them. As the teeth are moved during orthodontic treatment, occlusal trauma can occur that may result in periodontal disorders. As treatment continues, progressive periodontitis can develop, resulting in lost gingival attachment. This is a result of the tissue inflammation not being controlled. Improper orthodontic therapy can also be a factor. If the forces are too great or the movement is too rapid, permanent periodontal problems can develop.
One of the hidden scars of orthodontic treatment is root resorption (Fig 3-2). Although much research has been done on this phenomenon, there is still uncertainty about what actually causes this condition.
With all these potential problems arising during orthodontic treatment, the forces instigating dental movement should be as gentle as possible.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


