CHAPTER 5
Sagittal Skeletal Alteration and Vertical Skeletal Control
“The quality of our expectations determines the quality of our actions.”
—André Godin
A ligning the teeth into normal positions within the arches is the simple part of orthodontics. The major challenge faced by orthodontists is the correction of skeletal problems. One of the most interesting subjects in orthodontics is growth and development. During my 45 years in orthodontics, the knowledge and understanding of this subject has changed dramatically.
Under certain circumstances, particular forces can create excellent changes in the maxillofacial complex. In orthodontic treatment, the affected areas include the maxilla, mandible, and dentoalveolar complex.
I first discovered this knowledge when studying the effects the Milwaukee brace had on tooth position and maxillofacial growth during scoliosis treatment. The conclusions of my research1 stated that the forces the Milwaukee brace applied to the mandible demonstrated a directional change of growth in the lower face of a growing child. The occlusal forces created by the brace extruded the incisors and depressed the molars. These forces also depressed the total anterior face height. This new knowledge changed the way the profession thought, shifting focus from dental tooth movement to dentofacial orthopedics.
However, although this study showed that maxillofacial growth can be permanently altered (Fig 5-1), it is clinically impossible to create the same force levels delivered almost 24 hours a day as those achieved by the Milwaukee brace.
Growth
Before orthopedic forces have an opportunity to control or change growth, the patient must have growth potential. Because girls generally grow sooner than boys, early treatment in the mixed dentition is usually more successful with girls. If possible, delaying treatment in boys is preferred. Several methods have been used to determine growth potential. Hand, wrist, and cervical vertebrae radiographs are useful but tend to be unreliable in the borderline stages in which it is unknown whether the patient has any growth left. The old-fashioned way of observing the size of the parents and siblings and talking with the parents about the growth potential is usually as good an indicator as other approaches.
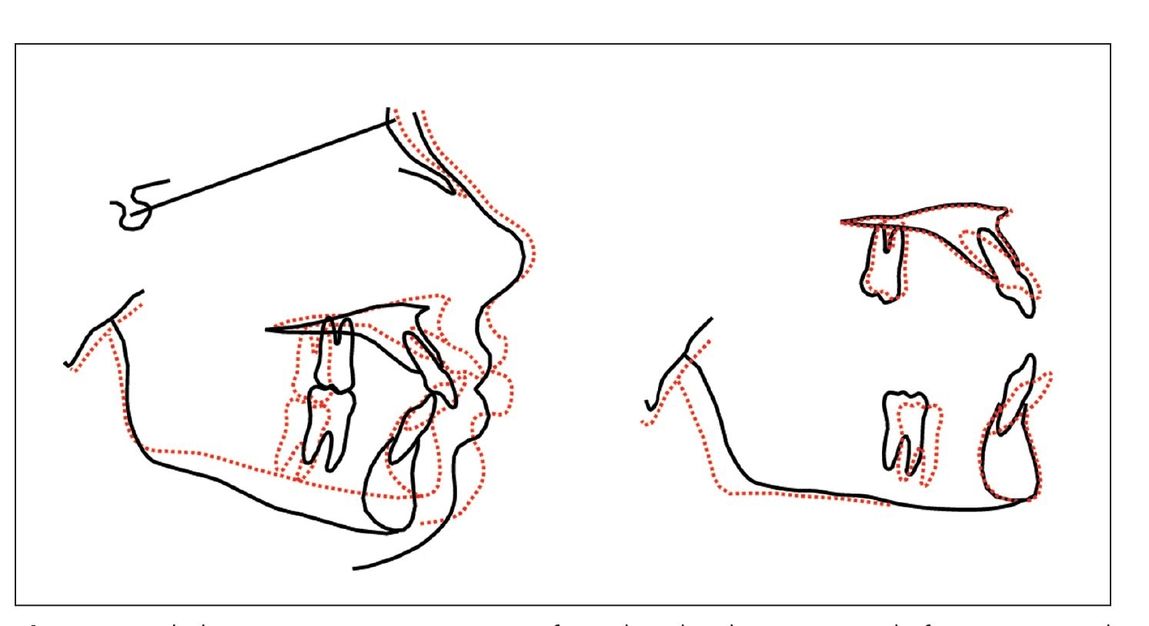
Fig 5-1 Cephalometric tracing comparison of a Milwaukee brace patient before (black) and after (red) wearing the brace.
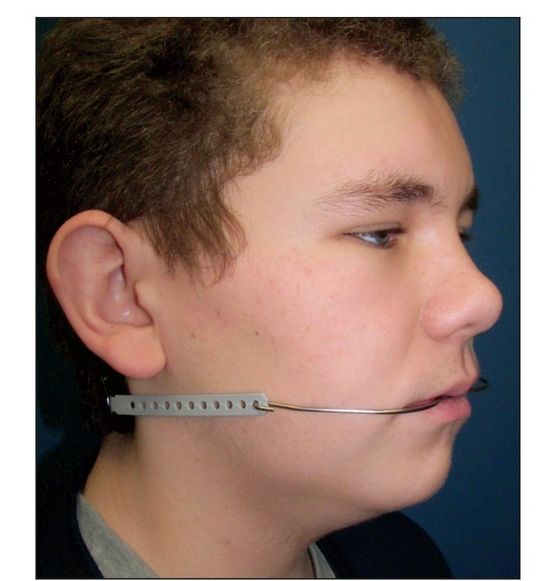
Fig 5-2 Patient wearing a cervical facebow.
Growth takes place in three planes of space: transverse, vertical, and sagittal. This chapter discusses sagittal and vertical skeletal deficiencies and how they can be corrected, and chapter 6 discusses transverse skeletal issues. As clinical orthodontists, we need to understand how much we can affect the facial skeletal patterns in growing patients. Orthodontically, the maxilla is our best friend. If the timing is correct while the patient grows, the maxillary bone and teeth can be permanently and significantly altered without surgery.
Sagittal Skeletal Control
The cephalometric goal of sagittal skeletal control is the correction of ANB to 1 to 3 degrees. In my analysis, the sagittal skeletal pattern is measured by SNA, SNB, and ANB. The Wits analysis can be more accurate in high-angle and Class III skeletal patterns.
Maxilla
The maxilla is a very malleable bone. Its forward growth can be controlled effectively by the use of orthopedic appliances such as the facebow (Fig 5-2) or functional appliances. As shown in many studies,2–5 the maxilla can be sagittally inhibited from growing while the mandible continues to grow to its genetic potential. On the other hand, in skeletal Class III patients, the maxilla can be advanced slightly by the use of a face mask.6
Evidence
The positive results that can be achieved with a cervical facebow are best described in a study by Sproul2 (Fig 5-3). The conclusions include the following:
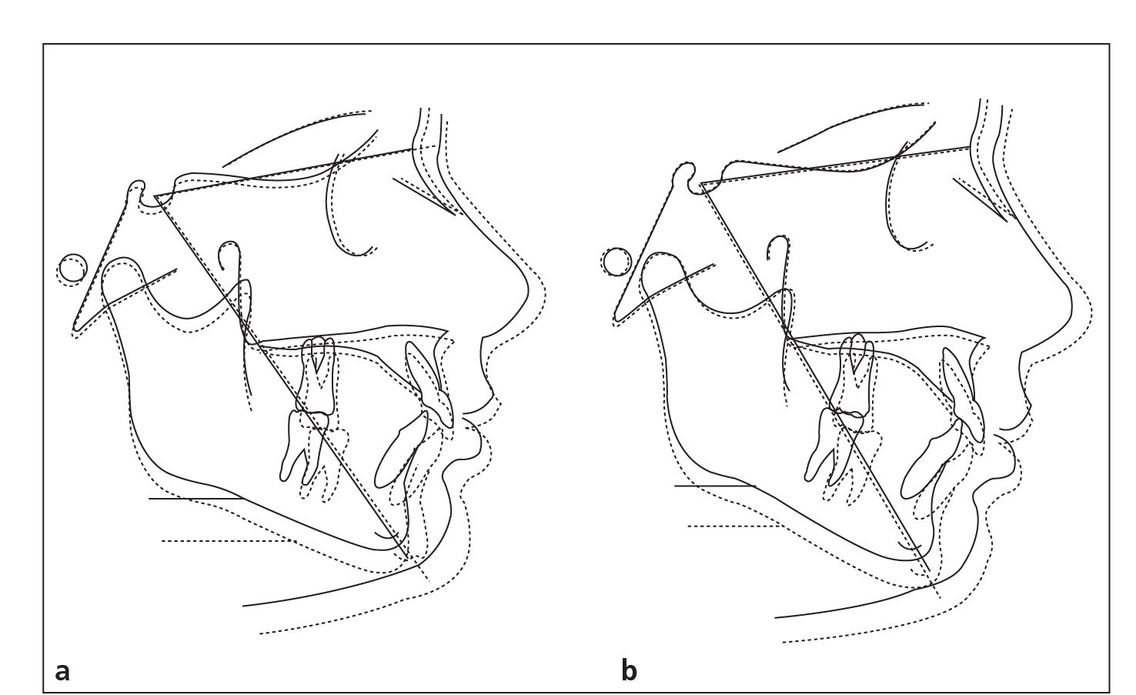
Fig 5-3 Superimposition of pretreatment (solid lines) and posttreatment (dotted lines) composite tracings of maxillary protrusive (a) and mandibular retrusive (b) groups with y-axis changes.
- The treatment of Class II malocclusions with cervical facebow and fixed appliances, according to the principles of the Alexander Discipline, improves the skeletal component of the malocclusion by restricting the anterior growth of the maxilla while the normal growth pattern of the mandible is expressed in both maxillary protrusive and mandibular retrusive Class II malocclusions.
- The maxillary protrusive group showed a significantly greater reduction in ANB and convexity measurements than the mandibular retrusive group because of the combination of greater restriction of the anterior growth of the maxilla and a more forward growth of the mandible.
- Mandibular plane angle changes were found to be insignificant for both maxillary protrusive and mandibular retrusive groups.
- The eruption of the maxillary and mandibular incisors was maintained at insignificant levels with treatment in both groups.
- The mandibular incisor inclination to the mandibular plane was not significantly increased in either group.
- The soft tissue convexity of the face was reduced and improved by significant increases in the anterior position of the soft tissue pogonion for both groups. Small increases in the position of the soft tissue landmark sub-spinale were found to be insignificant in both groups.
- The anterior positions of the upper and lower lips were found to significantly decrease in relation to the Sn-Pg and E-planes for both groups. Accordingly, the nasolabial angle measurement increased, but the increase was not significant for either group.
- A qualitative assessment of posttreatment superimposi-tions of both treatment groups with an age-matched Bolton norm tracing revealed that the average bony and soft tissue profile of the maxillary protrusive group more closely resembled the Bolton norm.
Several other long-term studies have been published from the Room of Truth concerning skeletal correction of Class II malocclusions. In Glenn’s study,3 anteroposterior mandibular growth continued from T1 through T3. Little change was noted in the SNB angle. A decrease of 2 degrees in the ANB angle from T1 to T2 was noted with little change occurring postretention. The ANB angle also decreased 2 degrees during treatment in Elms’s study.4,5
Mechanics
When addressing the long-term stability of orthodontic treatment, ideally the occlusion needs to be in a Class I skeletal pattern, not necessarily a Class I dental pattern. Clinically, the majority of our patients present with Class II malocclusions. Although there are numerous options to address this type of malocclusion, I have accomplished much long-term success through the use of the facebow. At this time in orthodontic history, I believe that the facebow is the most effective and inexpensive Class II appliance.

Fig 5-4 Example of an expanded inner bow parallel to the headgear tube.
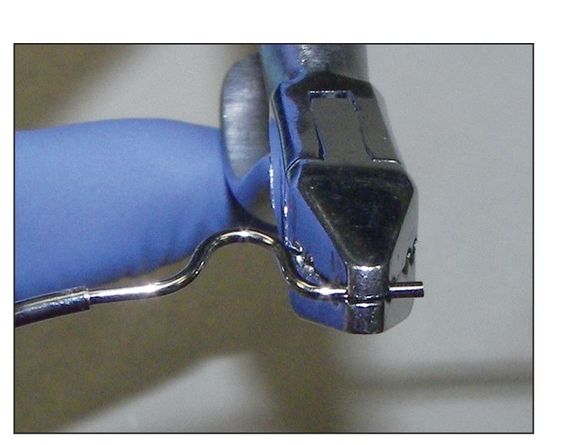
Fig 5-5 The distal end of the expanded inner bow is bent to be parallel to the headgear tube.
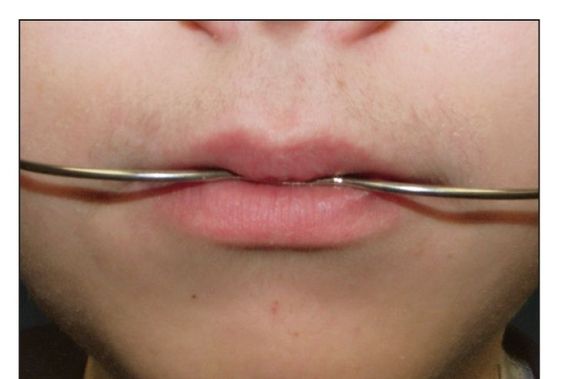
Fig 5-6 The connection of the inner bow and outer bow should be positioned just beyond the closure of the lips and balanced between the upper and lower lips.
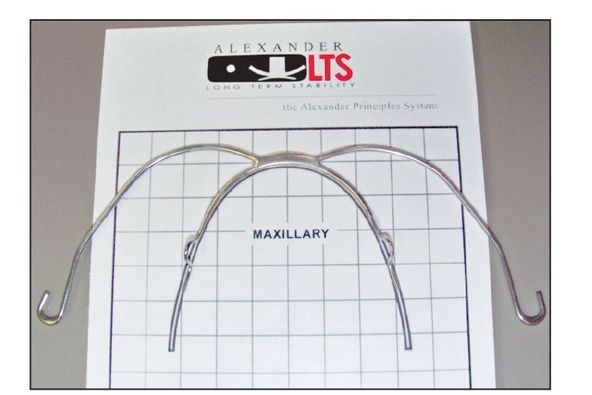
Fig 5-7 Inner bow of a facebow on the archwire template.
Facebow adjustments
To achieve success with facebow treatment, this appliance must be adjusted properly, as discussed in the first volume of this series.
Transverse adjustment. In the transverse dimension, an inner-bow expansion of approximately 4 mm should be maintained at each appointment (Fig 5-4) in order to widen the usually narrow maxillary intermolar width found in Class II skeletal patterns. In addition to the facebow, this transverse expansion can be accomplished by rapid palatal expansion or archwire expansion depending on the severity of the needed expansion.
Molar rotation. The distal end of the inner bow, the portion inserted into the headgear tube, must be adjusted so that it can enter passively. Because the molars are being rotated by the archwire and the 15-degree distal offsets in the first molar tube, this adjustment must be repeated at each appointment (Fig 5-5).
Sagittal adjustment. The anteroposterior position of the inner bow–outer bow connection is just anterior to the lips at rest (Fig 5-6). This positioning is accomplished by enlarging or constricting the adjustment loop on the inner bow.
Vertical adjustment. Vertically, the facebow is positioned at the center of the lips. This is accomplished by bending the inner-bow wire, where it enters the headgear tube, up or down as necessary. After the facebow is attached, its vertical position should not change. Initially, the inner bow is adjusted to be similar to the maxillary arch form template (Fig 5-7).
Vertical Skeletal Control
The vertical dimension is decidedly the most difficult growth pattern through which to effect skeletal change. The Milwaukee brace study1 indicated that it is possible to permanently decrease the mandibular angle if the force is strong enough. However, as previously mentioned, such force and time requirements (22 hours per day) are not realistic for a patient to achieve. If the patient has a vertical skeletal pattern, it is extremely difficult to do anything more than control this pattern and prevent it from getting worse. This in itself is a clinical challenge.
Treatment of high-angle patients is accomplished with the use of a high-pull facebow. Extractions, in some cases, and muscle-squeezing exercises may also help to a lesser degree. With these treatments, if followed conscientiously, the high-angle pattern can be controlled nonsurgically.
With the advent of miniscrews (temporary bony implants), a continuous intrusive force can be achieved, which could actually reduce vertical dimensions. Future well-controlled studies are needed to confirm this possibility.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


