CHAPTER 2
Selective Literature Review on Long-Term Stability
“Facts are stubborn things.”
–John Adams
What does the literature tell us concerning long-term stability? The most common form of dental malocclusion treated by orthodontists is crowding of the dentition, also known as tooth size–arch length discrepancy (TSALD). Only 34% of adults have well-aligned mandibular incisors, and these teeth continue to crowd with age. Nearly 15% of the population has extremely irregular incisors (more than a 10-mm irregularity index).
What determines tooth position? According to the equilibrium theory, the tongue pushes the teeth outward, the lips and perioral musculature push teeth inward, and developmental changes are also a factor. These are changes that occur throughout life in untreated individuals.
What about the stability of untreated occlusions? All studies show a loss of intercanine width shortly after the eruption of the permanent canines. Maxillary intermolar width remains the same or increases slightly during the transition from adolescence to adulthood. Mandibular intermolar width reacts similarly. Arch length and depth decrease in both arches with age, and this decrease is greater in the mandible. In 1983, Sinclair found that the arch length decreased almost 5 mm during the transition from mixed to permanent dentition.1 During this transition, the maxillary arch perimeter increases, and the mandibular arch perimeter decreases. Also, implant studies have shown that maxillary and mandibular basal bone change with growth.
History of Treating Malocclusion
In 1907, Edward H. Angle (Fig 2-1) became the father of modern orthodontics. His philosophy of treatment was totally nonextraction,2 despite Calvin Case’s challenge3 and advocation of selective extractions in 1905 (Fig 2-2). For the first half of the 20th century, Angle’s philosophy dominated. In 1944, Charles H. Tweed (Fig 2-3) became the most prominent proponent of extractions.4 While I was in graduate school during the mid 1960s, Drs Westfall and Gaylord had a large influence on bridging the transients from Tweed to contemporary orthodontics. During the 1970s, the pendulum began to swing again, led by Rolf Frankel in 1971.5,6 His Functional Regulator 2 screened dental arches from the musculature. This created tension in the alveolar bone, resulting in wider arches for nonextraction treatment.
Fig 2-1 Edward H. Angle.
Fig 2-2 Calvin Case.

Fig 2-3 Charles H. Tweed.
Relapse
To the casual reader, the literature may seem contradictory on the inevitability of the relapse of mandibular incisors. However, a diligent review of the referred literature and unpublished theses reveal that a majority of the long-term postretention studies have found satisfactory stability of less than 3.5 mm.7–17 In fact, most of the change from posttreatment to postretention is little or no greater than the change found with normal growth and aging.
My clinical experience has reflected these findings. As my practice has matured and as my son J. Moody has taken control of the practice, we are routinely seeing patients whose parents were treated by me 10 to 40 years ago. When possible, long-term diagnostic records on these former patients are taken; therefore, a good library of various types of long-term malocclusions is being collected. Patients who underwent both extraction and nonextraction and who have been out of treatment and retention for a significant period of time are demonstrating that with proper diagnosis and treatment, orthodontics can be stable after treatment.
The question then becomes: Why are some cases stable while others are not? Generally, three causes for relapse can be easily identified:
- Abnormal muscular habits that cannot be controlled by orthodontic treatment. When the oral musculature is out of balance with its environment (Fig 2-4), keeping the teeth in stable positions is virtually impossible. Thumb or finger sucking must be eliminated before orthodontic treatment can be successfully completed. Several techniques can be used to achieve this result. The method of choice is for the orthodontist to take the time to reason with the patient about why this habit must be stopped. Although this technique is time-consuming for the clinician, it is over 90% effective. Other techniques using fixed appliances, such as a tongue rake, can be used if the other approach fails. Mouth breathing negatively affects stability by causing muscular imbalance. Blockage in the airways must be addressed early in treatment. In certain cases, adenoid or tonsil removal may be recommended.
- Poor growth patterns that do not respond to orthodontic treatment. Excessive vertical growth (vertical maxillary excess) (Fig 2-5) causes abnormally long lower anterior face height, which prevents the patient from being able to keep the lips closed in a relaxed position, thus causing muscular imbalance and potential relapse. Excessive mandibular growth can occur after treatment has been completed, which will cause orthodontic relapse.
- Poor diagnosis, poor treatment, or poor patient cooperation. These may be the greatest causes of relapse. Diagnosis and treatment are the factors most under the control of the orthodontist.
Certain criteria must be followed and particular goals achieved to maximize the likelihood that a patient will exhibit satisfactory stability over a period of years. In addition to the active therapy, proper retention procedures must be followed.
So where is the state-of-the-art position in diagnosis and treatment planning currently? Treatment choices for gaining space include (1) extraction and (2) nonextraction: interproximal enamel reduction, expansion of arch width, increasing arch length, and flaring of the anterior dentition.
In other words, either increase the space available for teeth or decrease tooth mass. Yet how should this decision be made? Does it really make a difference? Is long-term stability affected?

Fig 2-4 Anterior view of open bite. Open bite causes mouth breathing, which leads to muscular imbalance and thereby threatens stability.
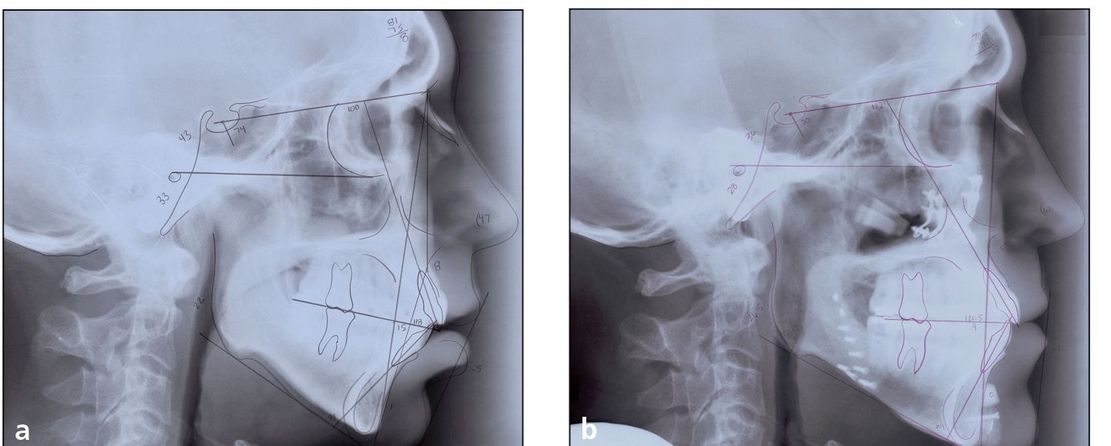
Fig 2-5 (a) Pretreatment cephalometric tracing and radiograph of a patient with vertical maxillary excess. Note that the lips are open while the patient’s muscles are relaxed. (b) Posttreatment cephalometric tracing and radiograph of the same patient. Note that the lips are now closed.
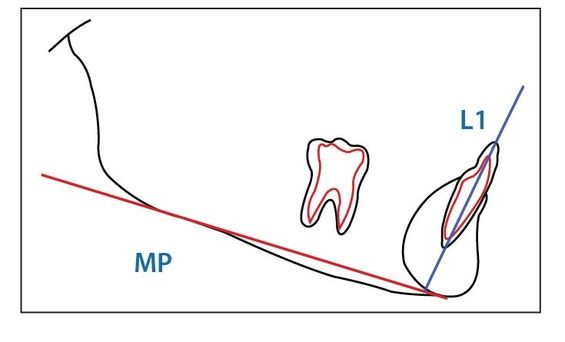
Fig 2-6 Mandibular incisor position and plane angle.
Cephalometric Guides
Cephalometric measurements are important guides, but they should not be taken as final truths. Much emphasis is placed upon the vertical and sagittal growth dimensions. These dimensions are identified to determine the amount and direction of growth of the patient’s skeletal pattern.
The mandibular incisor position (Fig 2-6) is observed and a decision made as to where the final position should be. Where is the most stable position of the mandibular incisors? Tweed stated that “the lower incisors should be upright on the basal bone.”4 It has been my observation that “stable” is the position in which the patient presents. A stable range for mandibular incisors can be from 70 degrees to 110 degrees depending on the skeletal pattern of the patient.
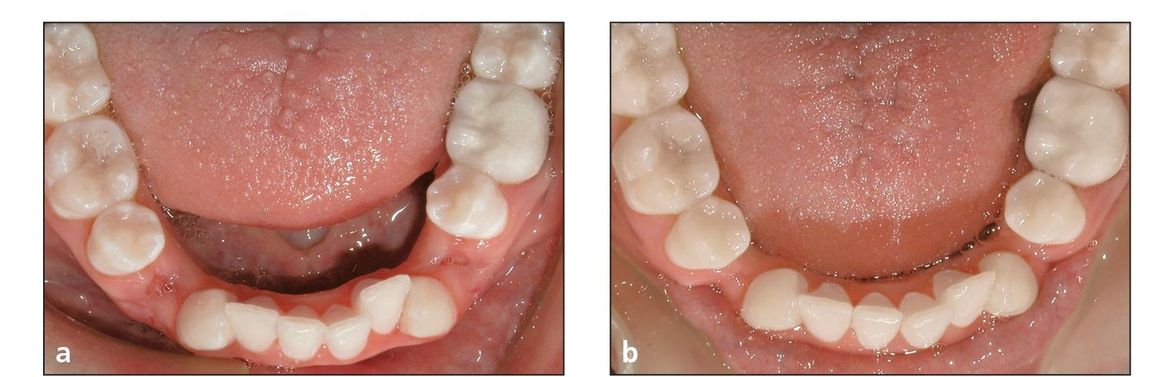
Fig 2-7 Driftodontics. (a) Mandibular arch directly after the extraction of four first premolars. Treatment is initiated on the maxillary arch only. (b) Mandibular arch after driftodontics have occurred, reducing the space between the canines and the second premolars.
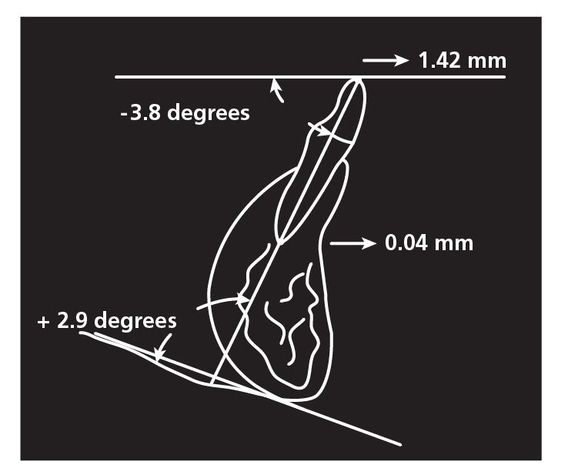
Fig 2-8 Nevant’s drawing of the mandibular incisor’s tipping labially 1.42 mm.
The mandibular incisors can be uprighted a great amount and remain stable. Papandreas studied the amount of drift that takes place when four first premolars are extracted in Class I malocclusions and treatment is initiated only on the maxillary arch.18 This “driftodontics” of the mandibular teeth (Fig 2-7) demonstrated some interesting results. Papandreas found that on an annual basis, (1) the mandibular anterior teeth uprighted an average of 8 degrees; (2) the canines drifted distally and expanded 1.7 mm; and (3) the molars drifted forward only 1.2 mm.
Clinically, this study shows that the mandibular anterior teeth move distally more than the molars move anteriorly. And although the mandibular intercanine width expands, other long-term studies show that this expansion is not stable.
Why would this be true? In my extraction protocol, the maxillary canines are retracted to a wider part of the arch early in treatment. Does it not make sense that these maxillary canines protect the mandibular canines from the perioral musculature during this time period (about 6 months)? However, after all spaces are closed and centric relation and final arch form are obtained, the mandibular canines should show little, if any, intercanine expansion.
Nevant showed some interesting results regarding the advancement of mandibular incisors.19 In his study of 40 patients (20 each from two practices), the mandibular incisors tipped labially 1.4 mm, 3 degrees in each case (Fig 2-8). Does this indicate that an anterior limit exists as to how far the incisors can be advanced and still be in stable positions? This study, with others, helped us develop the 3-degree rule in advancing mandibular incisors.
In addition to torque control of the mandibular incisors, the maxillary incisors and their relationship with the mandibular incisors must be addressed. To maintain the corrected overbite, good maxillary torque and interincisal angle must be established during treatment (see chapter 4).
Mandibular First Molar Position
In deep bite cases, the permanent correction of overbite is also related to the ability to upright, or tip back, the mandibular first molars.20 By uprighting the first molars, several good things result:
- As much as 3 mm of mandibular arch length is gained.
- First and second premolars are simultaneously extruded to help level the mandibular arch.
- Posterior occlusal stops are established to prevent anterior overbite relapse. Clinically, this is accomplished by placing reverse curve in the mandibular tied-back archwire. The–5-degree bracket torque in the incisor brackets and–6-degree tip in the first molar band/bracket will allow the controlled leveling of the mandibular arch.
In their discussion of the Alexander Discipline, Bernstein et al highlight its effectiveness in leveling the curve of Spee in Class II, Division 1 deep bite cases using nonextraction.21 This is accomplished by combining premolar extrusion with minor incisor intrusion (Fig 2-9). Mandibular incisor position is therefore controlled during the leveling process, and excessive flaring is avoided. In addition, although there is a 30% loss after treatment, the–6-degree angulation in the molar band prevents the mandibular molar from tipping back during treatment. In addition, Bernstein et al note that the Alexander Discipline does not cause excessive opening of the vertical dimension during treatment.21 The angulation of the functional occlusal plane is altered, and it appears to remain stable over time, making the results of this treatment stable in the long term.
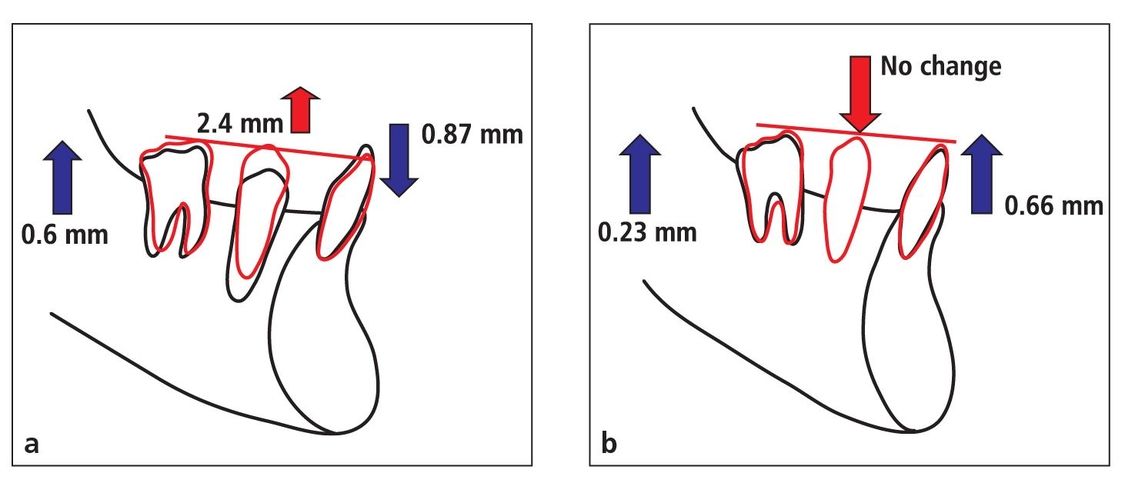
Fig 2-9 (a) Treatment effects of reverse curve of Spee in archwires as demonstrated in the studies of Bernstein et al21 and Carcara.22 (b) At an average posttreatment period of 11 years 5 months, the results show no relapse in the premolar area, and thus the leveled arch is maintained.
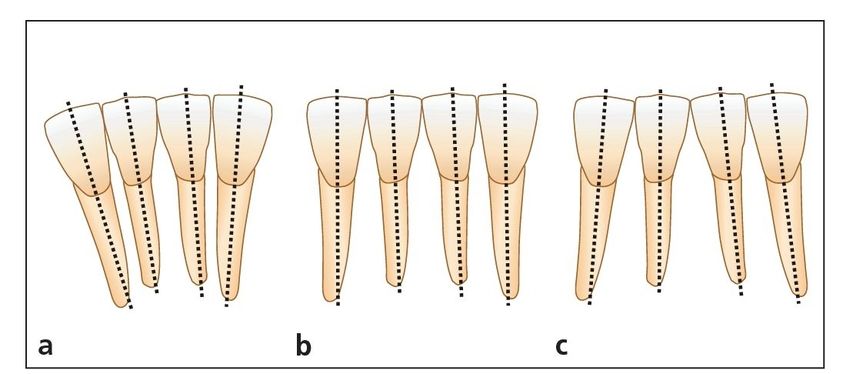
Fig 2-10 Mandibular incisor angulation.
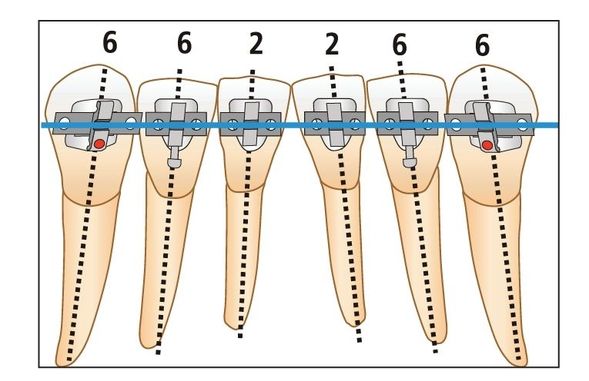
Fig 2-11 Bracket angulations (in degrees) of the mandibular incisors and canines.
Angulation (Artistic Positioning) of Mandibular Incisors
Williams observed that the mandibular lateral incisors should be positioned with more angulation to improve stability 23 (Fig 2-10). My clinical observation of posttreatment patients over the years has led me to agree that one of the causes of relapse in the mandibular anterior arch is poor artistic positioning of the mandibular lateral incisors. If the incisal edges of the mandibular anterior teeth are aligned evenly, the lateral incisors will be too upright. However, when the roots of the lateral incisors are aligned more parallel to the roots of the canines, relapse seems less severe and may not occur at all (Fig 2-11).
Active Treatment
After the patient’s malocclusion and skeletal pattern, including factors already mentioned, are evaluated and goals for the treatment objectives are set, orthodontic treatment is initiated. The philosophy of treatment is to begin with the end in mind.
Although all of the goals mentioned can be achieved with any orthodontic edgewise appliance, it makes sense to incorporate as many of these factors into the design of a straight-wire appliance. Therefore, a bracket system has been designed that places the teeth in specific positions to help eliminate relapse, as long as proper diagnosis and treatment planning have taken place.24,25
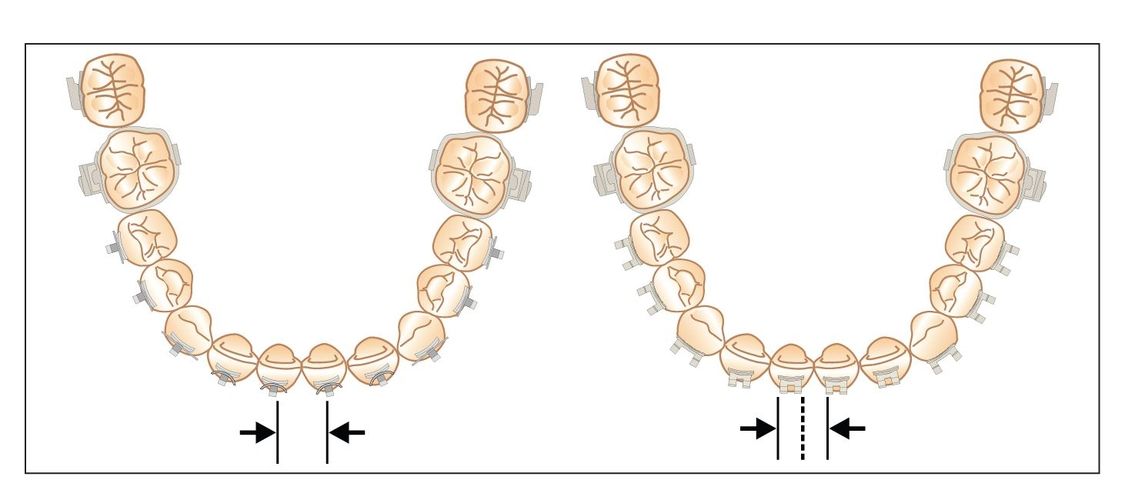
Fig 2-12 Increased interbracket distance. Almost 50% more interbracket distance is obtained with single (left) versus twin (right) brackets.
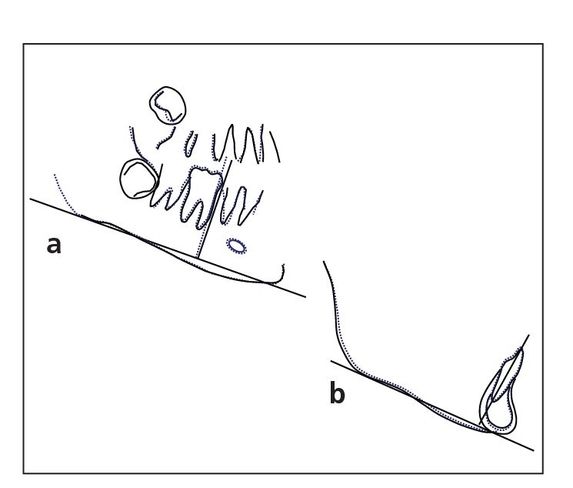
Fig 2-13 (a) Uprighting molar. (b) Incisor torque control.
Bracket design, bracket placement, and selected individualized forces will allow the teeth to be positioned properly during treatment. These steps are specifically addressed in chapters 6 and 7 of volume 1 of this series.
Finishing procedures,26 band removal, and retainer placement must be properly orchestrated. A regimented retention sequence is then followed that will help enhance long-term stability for the patient.
These clinical observations are the results of more than 40 years of orthodontic practice in which I have treated more than 15,000 patients with fixed edgewise appliances. In addition to clinical observation, research findings by the Baylor Orthodontic Department graduate students27–30 as well as studies from other programs and individuals show that orthodontic treatment can be stable long after the appliances are removed.
Alexander Discipline Technique
The Alexander Discipline technique is designed to place the teeth in positions that promote function, esthetics, stability, and health of the periodontal tissues. Four specific factors make this technique different from others: (1) its unique bracket selection and prescription, (2) its unique arch form, (3) its treatment mechanics, and (4) its stability.
Unique bracket selection and prescription
Specific bracket designs are created for specific teeth. Increased interbracket space created by single brackets with wings instead of twins allows more flexibility with a stiffer archwire (Fig 2-12), resulting in easier engagement and fewer archwire changes. Rotational wings give controlled guidance and direction to teeth.
A special prescription of torques and angulations gives the Alexander Discipline a unique straight-wire appliance. In treatment, maximum efforts should be made to control mandibular incisor flaring and intercanine width. The most significant and important design feature unique to this bracket system is expressed in the mandibular anterior brackets. Single brackets with wings create an advantage not possible with twin brackets. To control mandibular incisors, each tooth is ligated initially with a rectangular flexible wire. The resistance of the incisors to tip labially, caused by the–5-degree torque in the incisor brackets, places a distal force on the first molars (angulated at–6 degrees), causing them to upright. This can gain 2 to 3 mm of arch length without flaring the incisors (Fig 2-13).
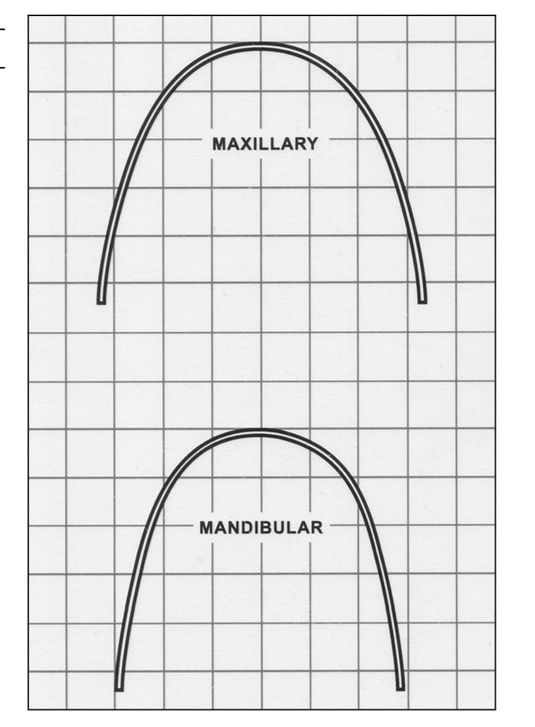
Unique arch form
The arch form used in the Alexander Discipline is developed by the compilation of hand-bent archwires to provide an arch form that will fit most patients within one standard deviation. It is more stable than other commercially available arch forms29,31 (Fig 2-14).
Fig 2-14 Alexander long term stability arch form tem plate.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


