Every orthodontic patient presents with a unique set of dental, occlusal, and skeletal discrepancies that require individualized treatment approaches as well as specific biomechanics to place teeth in the most ideal and stable position. Although distinctly different biomechanical approaches can be used to accomplish tooth movement, some methods are more effective and efficient at delivering the forces and placing the teeth and roots closest to the desired location while minimizing undesirable side effects. A firm foundation in sound biomechanical principles provides the orthodontist with the knowledge to make creative and efficient biomechanics plans and to design appropriate appliances that, contrary to popular belief, can be both patient friendly and staff friendly.
To date, continuous archwire mechanics remains the most often used and popular form of mechanics. Although this mechanical approach has several advantages, including ease of use, patient comfort, short chair-side doctor time, and ability to delegate to the staff, it also has several limitations. Thus, in some clinical situations, continuous archwire mechanics may be inappropriate or inefficient to deliver the type of tooth movement desired.
In contrast, segmenting the arch enables the implementation of many novel and efficient force systems designed to enhance patient care and treatment results. Segmented archwire mechanics has several disadvantages, however, including potential difficulty in designing custom-spring applications, careful activation to obtain controlled tooth movement, some level of patient discomfort, and the decreased ability to delegate to staff. Alternatively, many clinical situations are optimally suited to enable the orthodontist to combine the advantages of both continuous archwire mechanics and segmented arch mechanics in an approach called hybrid sectional mechanics.
This chapter provides an overview of continuous and segmented mechanics, introduces the concept of hybrid sectional mechanics, and uses biomechanical principles to discuss the pros and cons of each of these approaches. This chapter also describes the selective use of continuous, segmented, and hybrid sectional mechanics for individual cases and arches to achieve optimal and efficient treatment results, particularly in complex and compromised cases.
RECOGNIZING COMPLEXITIES TO AVOID PITFALLS
Before implementing treatment, the orthodontist must make an accurate and appropriate diagnosis, derive the treatment objectives, critically assess the various treatment options, and select an optimal treatment plan for the patient. The full principles of orthodontic diagnosis and treatment planning are beyond the scope of this chapter and therefore are not discussed here. However, within the context of treatment planning, it is important to realize that in addition to making important decisions about the overall treatment approach, such as whether or not to extract, which teeth to extract, and whether to incorporate surgery, the clinician must be equally diligent in planning the biomechanics, appliances, and wire sequences. In other words, the comprehensive treatment plan incorporates decisions on extractions and surgery, as well as optimal and customized biomechanics.
One of the more challenging components of designing the patient’s individualized biomechanical treatment plan is determining or predicting potential difficulties or adverse tooth movements that might occur during treatment. In general, it is more efficient to recognize these mechanical or treatment complexities before initiating treatment. Early recognition of potential problems enables the orthodontist to plan strategies to avoid difficulties or adverse tooth movements during treatment. Additional benefits of such a proactive approach to biomechanical planning include better treatment outcomes (as discussed later) and greater efficiency, resulting in increased orthodontic practice productivity and profitability with reduced stress.
CONTINUOUS ARCHWIRE MECHANICS
Indications
To enhance practice flow, orthodontists often use standardized treatment approaches that incorporate continuous archwire mechanics with the same or similar sequences of wires, retraction and space consolidation, detailing, and finishing for all patients. Although these “autopilot mechanics” have the benefits of the staff understanding and anticipating the next wire size or the next treatment stage, of possibly limiting clinician and staff time, and likely enhancing efficiency and productivity in most routine cases, the advantages of this approach may not apply to many complex and dentally or periodontally compromised cases. Indeed, the complications introduced by the use of routine mechanics in these cases will likely lead to increased treatment time, decreased productivity, and compromised esthetic and or functional results. Therefore, as a general rule, standard continuous archwire mechanics can be best used in most simple nonextraction cases, cases with spacing, extraction cases in which there is likely to be minimal round-tripping of teeth, or when decompensating in surgical cases.
Table 19-1 provides a listing of specific indications for continuous archwire mechanics and serves as a guide for clinical situations where alternate biomechanical approaches such as segmented archwire and hybrid sectional mechanics can be beneficial. Depending on the practice profile, approximately 40% to 70% of patients in a given practice would likely meet the criteria for use of routine continuous archwire mechanics to deliver the force systems necessary to produce the desired outcomes.
| Continuous Archwire | Segmented Archwire | Hybrid Sectional | |
|---|---|---|---|
| Generalized spacing | +++ | ||
| Mild crowding (nonextraction) | +++ | ||
| Crowding (extraction treatment; minimal round tripping anticipated) | +++ | ||
| Decompensations desired | +++ | ||
| Moderate to severe crowding (extraction treatment; round tripping anticipated) | — | +++ | +++ |
| Differential anchorage desired | — | +++ | ++ |
| Severe canine/premolar root angulations | — | +++ * | + |
| Asymmetric cases | — | +++ | + |
| Multiple missing teeth | — | ++ | +++ |
| Compromised periodontal health | — | ++ | +++ |
| Preservation of dental compensations | — | + * | +++ |
| Desire to perform multiple stages of treatment concurrently | — | + | +++ |
* Initiate with segmented, and follow up with hybrid sectional mechanics if needed.
Although primarily indicated for relatively routine cases, continuous archwire mechanics can be beneficial even in a select number of cases that are quite complex in which none of the contraindications listed in Table 19-1 are present, as in the following case.
Deformed dentoalveolar structures and generalized spacing
Figure 19-1 shows a patient who had recently recovered from a 6-month coma during which he had oral intubation. He presented with wide dental arches, deformed dentoalveolar structures, severely proclined upper and lower incisors, overerupted maxillary molars, and generalized spacing ( Fig. 19-1, A-H ). The generalized spacing resulted from the intubation, multiple missing teeth, macroglossia, and partial tongue paralysis. Both the proclined incisors and the buccally inclined molars had compromised periodontal health.


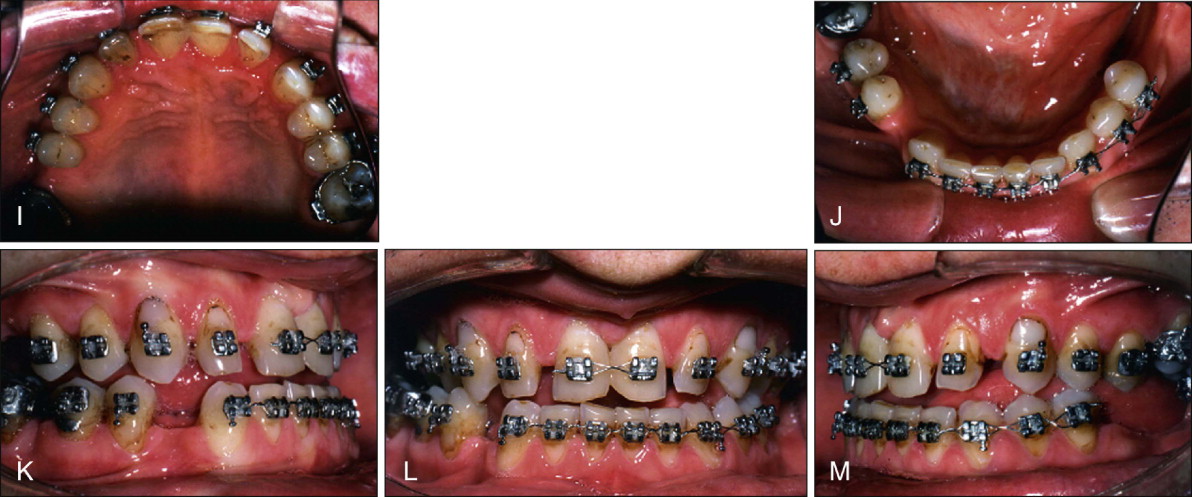
Periodontal evaluation, treatment, and maintenance therapy were performed before initiating orthodontic care. In addition, an orthognathic surgery consultation for evaluation of the underlying skeletal discrepancy and a reduction glossectomy were performed. The comprehensive treatment plan included periodontal management and reduction glossectomy, followed by orthodontic treatment with continuous archwire mechanics to consolidate and redistribute spaces and remove compensations as best as possible. As space consolidation and redistribution progressed, a final determination of space needs for restorations and obtaining optimal occlusal results was made in consultation with a prosthodontist. The final treatment stage required orthognathic surgery to achieve the best possible occlusal and esthetic results. Once orthodontic treatment was completed, the missing teeth would be replaced with a combination of implants and removable partial dentures.
Before orthodontic care began, the patient underwent a reduction glossectomy to enable retraction of the dentition. A decision was made to wait several months to allow for any self-correction of incisors resulting from the reduced tongue volume and pressure, which could alter the equilibrium on the teeth and possibly cause them to move lingually. After 1 year, however, only minimal incisor uprighting was observed. Treatment was then initiated with continuous archwire mechanics because of spacing and the expectation that minimal adverse tooth movements, including round tripping, would result from these mechanics. A routine archwire sequence, including nickel-titanium (Ni-Ti) wires for alignment and stainless steel wires with elastomeric power chains for space consolidation were used. A low-hanging transpalatal arch (TPA) was also placed to intrude or prevent the extrusion of the upper molars.
This patient was treated before the introduction of temporary anchorage devices (TADs). Had TADs been available, they would have been used to intrude the maxillary molars and maintain their anteroposterior position during space consolidation.
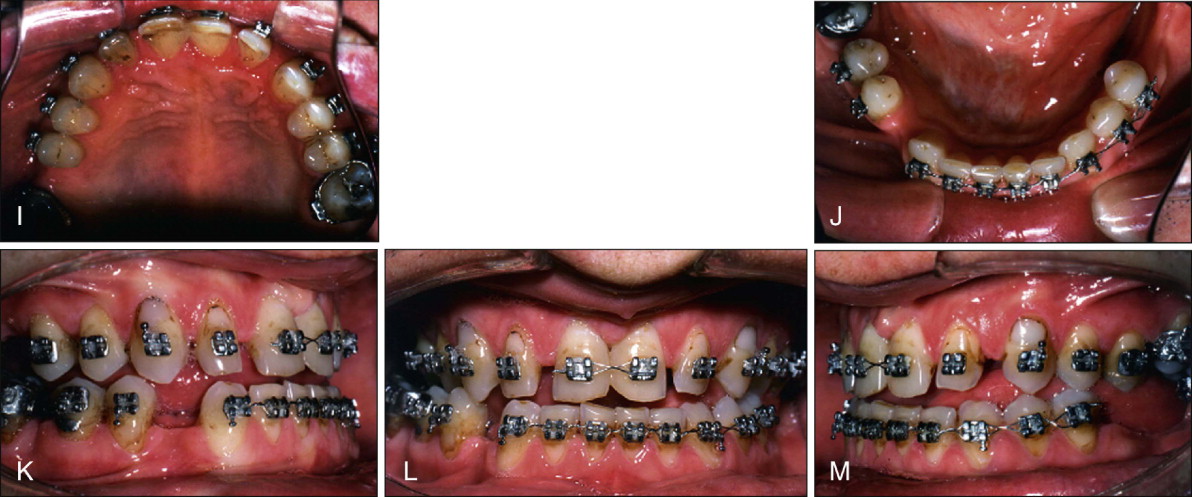
The decision on optimal space distribution and restorations were finalized as spaces were being closed. Presurgical records demonstrate the space consolidation and the significant amount of incisor retraction in both arches ( Fig. 19-1, I-M ). Small spaces were preserved in the maxillary anterior region because of an underlying maxillary Bolton deficiency. After surgery, the spaces were refined to enable the prosthodontist to fabricate appropriately sized central and lateral incisor restorations. The postorthodontic and postsurgical and prerestorative results demonstrate that in some complex cases, high-quality results are possible with conventional continuous archwire mechanics ( Fig. 19-1, N-U ).
Contraindications
Unlike the complex case in Fig. 19-1 , other cases may present with occlusal discrepancies that are not well suited for continuous archwire mechanics. Such cases include patients with multiple missing teeth, compromised periodontal health, asymmetric malocclusions, and moderately to severely crowded arches where round tripping is undesirable, as well as those where dental compensations must be maintained (see Table 19-1 ).
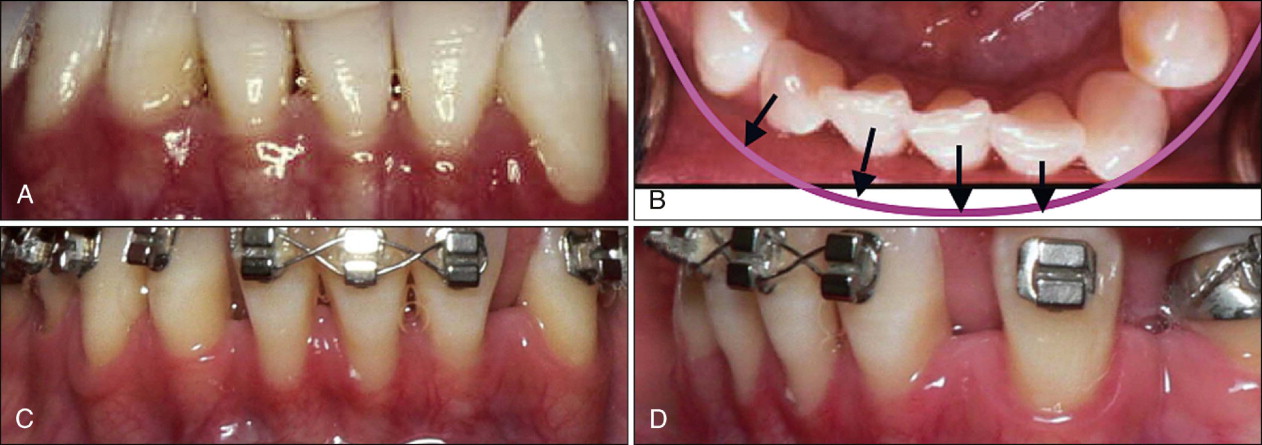
Additional examples of such cases include those patients who present with severe angulations of the canine, which occurs more frequently than realized, particularly in the mandibular arch ( Fig. 19-2, A ). If the canine presents with a severe mesial crown/distal root angulation, a continuous archwire will generate significant protrusive and intrusive forces on the incisors. Intrusion may be desirable, but because the intrusive forces are applied labial to the lower incisor center of resistance, additional proclination or flaring of the anterior teeth can occur ( Fig. 19-2, B ). Finally, because such a canine crown is often more labial than the incisors, it will tend to move the incisors labially ( Fig. 19-2, C ).
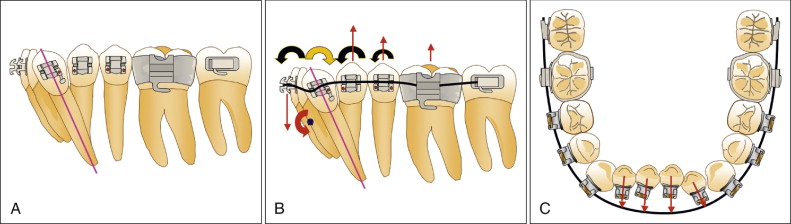
Of equal concern is the force system on the posterior portion of the arch resulting from the continuous archwire. As the continuous archwire exits the distal aspect of the canine bracket, it generates an extrusive force on the first and second premolars, as well as the first and second molars ( Fig. 19-2, B ). Large, multirooted teeth might be assumed to have enough anchorage to resist these extrusive forces, but this is not always the case. Extrusive forces to the posterior dentition, particularly in patients with long faces and weaker facial musculature, can result in undesired eruption leading to the iatrogenic development of an anterior open bite. In addition to these undesirable forces generated by the archwire, the teeth neighboring the canine also experience moments that cause the teeth to tip adversely ( Fig. 19-2, B ).
The consequences of such moments and forces in contributing to adverse and undesirable tooth movements are evident in the following case, which is followed by a description of the authors’ method of choice for distalizing crowns or roots of severely angulated teeth.
Severe dental angulations
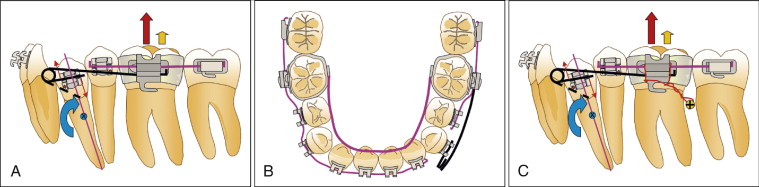
A 12-year-old girl presented with bimaxillary protrusion, incompetent lips from increased maxillary vertical excess and short upper lip, increased gingival display on smiling, and a Class I molar relationship with severe mandibular crowding ( Fig. 19-3, A-H ). Multiple viable treatment options ranging from orthognathic surgery to a variety of different extraction protocols could be used in this case. Because of the parent’s desire not to undergo surgery and because patient compliance was considered questionable, the orthodontist planned the shortest treatment approach possible. This included extraction of the upper first premolars and lower canines, combined with routine continuous archwire mechanics.
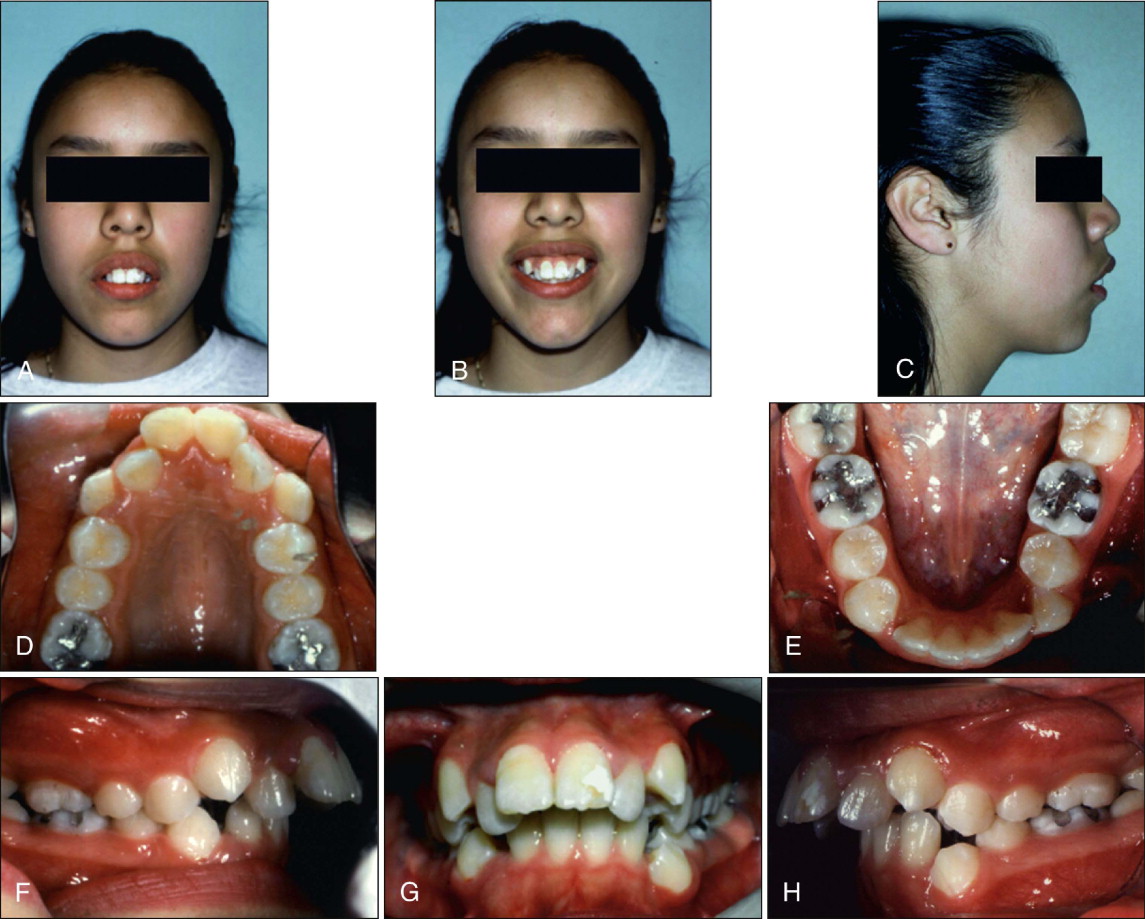
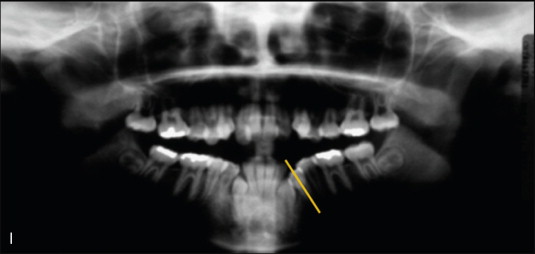
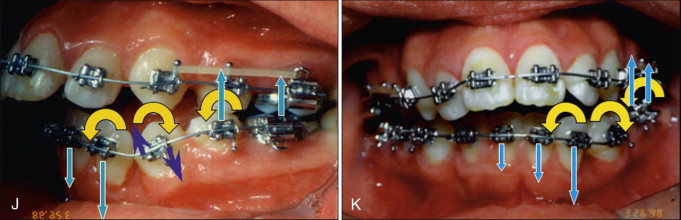
Unfortunately, in choosing these biomechanics, no serious consideration was given to the negative effects that would result from placing the wire into the bracket on the severely mesial crown/distal root angulated lower left premolar ( Fig. 19-3, I ). Placement of the initial series of Ni-Ti continuous archwires for alignment generated the desired moment to upright the premolar, but this also introduced force systems to intrude and flare the mandibular incisors, extrude the left posterior teeth, and produce rotational moments on the incisors and premolars ( Fig. 19-3, J and K ). These adverse movements largely occur asymmetrically on the side with the mesially inclined premolar, resulting in canting of the anterior and posterior occlusal planes, an asymmetric left anterior and lateral open bite, and an increase in vertical face height caused by the posterior extrusion.
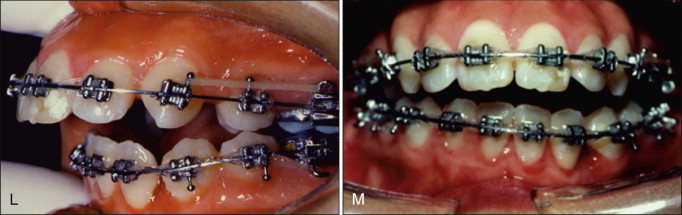
As stiffer, stainless steel wires were inserted and left to work until passive, they produced the clinical findings depicted in Figure 19-3, L and M , which displays the results that could have been predicted from a detailed pretreatment mechanical analysis. Because of the undesirable and iatrogenic eruption of the posterior teeth and the creation of an asymmetric lateral and anterior open bite, additional treatment time and complexity have been added to the case, which now requires complicated mechanics to resolve. Although not an optimal method for resolving these undesirable consequences, significant anterior elastic wear was used to compensate for the open bite. The pre-debond occlusion, although not optimal, is acceptable compared with the very poor occlusion during treatment ( Fig. 19-3, N-S ). However, the extrusion of the anterior teeth due to the extensive use of vertical elastics has resulted in substantially diminished esthetics due to excessive gingival display, not only when smiling but also in repose.
The poor choice of initial mechanics resulted in negative facial changes and substantially increased her treatment time to 4 years. These consequences are highly undesirable from both a patient and practice management perspective.
This case represents several occlusal discrepancies that contraindicate the use of continuous archwire mechanics (see Table 19-1 ). These include the severe angulation of the premolar and the asymmetry between left and right premolar angulations ( Fig.19-3, A-I ) that, when corrected with continuous archwire mechanics, is transferred to other parts of the arch ( Fig. 19-3, J-M ).
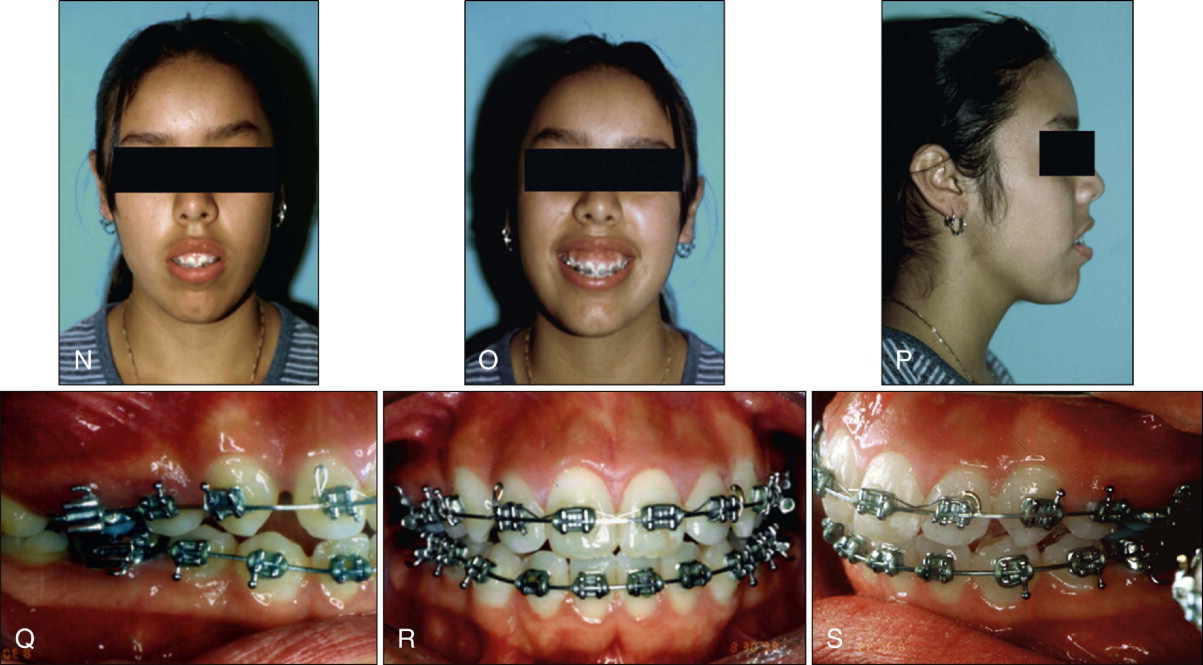
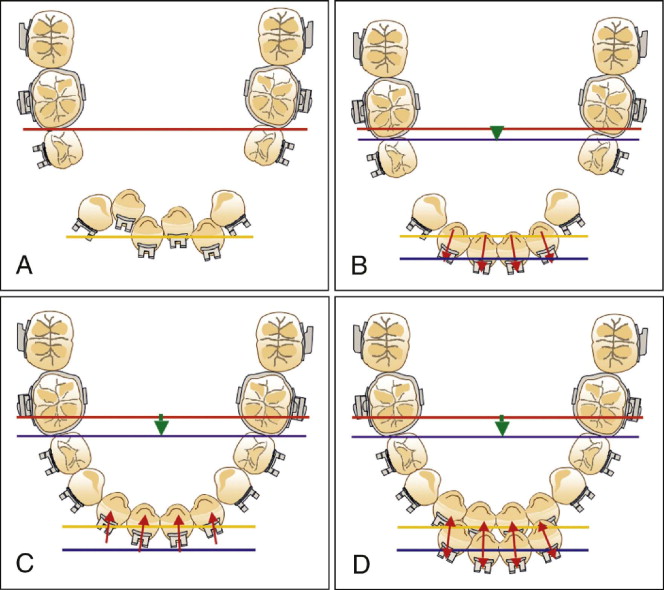
An alternative and optimal approach to correct this malocclusion would strategically focus first on correcting the premolar angulation with a segmented mechanical approach, as depicted in Fig. 19-4 . Any type of segmental spring that introduces a moment that moves the premolar root mesially can be designed and engaged in the premolar and molar brackets. Using the principles of biomechanics, it is clear that the desired clockwise moment on the premolar generated by this spring results in an undesired extrusive force on the molar ( Fig. 19-4, A ). The extrusion of the molar resulting from this extrusive force can be minimized by enhancing anchorage on this tooth by (1) incorporating a sectional wire on the second premolar and the two molars, (2) adding a lower lingual arch between the molars, and (3) if necessary, further reinforcing the anchorage on the contralateral molar by placing an archwire segment that engages the right quadrant up to the left lateral incisor ( Fig. 19-4, A and B ). Alternatively, these additional features for enhancing anchorage may be replaced by a TAD placed gingival and distal to the left molar and simply tied to the molar to prevent adverse vertical and mesial movements of the molar ( Fig. 19-4, C ). Once the premolar has been fully uprighted, the case could be routinely finished through continuous archwire mechanics.
Round Tripping
Another clinical problem that can be difficult to avoid with continuous archwire mechanics is “round tripping.” When initial alignment is performed in a crowded arch using a continuous archwire, the clinician is attempting to align crowded teeth by increasing the overall length of the arch, which generally translates into expansion at the incisors, commonly referred to as “proclination.” This will occur in crowded arches even if teeth have already been extracted ( Fig. 19-5, A and B ). Subsequently, after canine retraction the incisors are also retracted ( Fig. 19-5, C ). The initial proclination of the incisors followed by their retraction is often referred to as “round tripping” ( Fig. 19-5, D ).
The final position of the teeth after “retraction” might not be significantly different from the start position, but the path traveled by the teeth is extensive. Also, if the incisors are overly proclined during initial alignment in a patient with thin alveolar bone support, it may be accompanied by tissue destruction such as gingival stripping or loss of crestal bone height, as depicted in Figure 19-6 . Another potentially negative consequence of round tripping may be root resorption resulting from unnecessarily proclining the incisors and placing their roots in contact with the lingual or palatal cortical plate or from the increased magnitude of tooth movement and time in treatment.
An additional potential adverse effect of round tripping is increased anchorage loss and its negative consequences on final incisor position and lip prominence. The anchorage loss occurs not only during initial alignment (i.e., posterior teeth drift forward as incisors procline) but also during retraction of the incisors from a more anterior position than at the start of treatment (see Fig. 19-5, B-D ). This results in less extraction space for retraction. If the goal of treatment is to perform significant retraction of incisors to improve incisor position and lip esthetics and competency, the desired facial goals may not be achieved.
Examination of the patient’s pretreatment records, particularly the casts and the lateral cephalogram, can help identify situations where incisor round tripping may have negative consequences. In this regard, situations that have incisor crowding or incisor flaring are of particular concern because placement of a continuous archwire will lead to their further proclination. Patients who also exhibit thin periodontal biotypes are at further increased risk of adverse changes. Thin biotypes are identified when the periodontal probe inserted into the gingival sulcus is visible through the patient’s translucent tissues, and by observing prominent roots on the labial aspect of the alveolus.
Another diagnostic aid for assessing the ability of periodontal supporting structures to adapt to proclination or round tripping of incisors is the thickness of the alveolar bone, which can be readily observed in lateral cephalograms, as demonstrated later. In some patients in whom the alveolar process around the incisor roots is relatively thin, significant labial or even lingual movement may contribute to tissue damage and loss in periodontal support. In the future, three-dimensional cone-beam computed tomography (CBCT) will likely provide additional diagnostic information that will be important in assessing the limits to which round tripping or proclination of incisors can be performed while maintaining integrity of bony structures housing the incisors.
Anchorage Considerations
An additional caveat of continuous archwire mechanics is that it poses a challenge in adequately controlling the anchorage at its extremes. The two extremes of anchorage are commonly described as maximum anchorage (or “A” anchorage) and minimum anchorage (or “C” anchorage). Symmetrically activated closing loops, coil springs, and elastomeric power chains all produce reciprocal space closure because these mechanics are unable to produce differential moment/force ratios in the anterior and posterior regions. Differential space closure with these mechanics is often achieved through intermaxillary elastics, which can provide some assistance to differential space closure but with drawbacks. Class II elastics will extrude the mandibular posterior dentition and extrude and retrocline the maxillary anterior teeth and potentially result in greater incisal display. The mandibular posterior extrusion will contribute to posterior occlusal plane anomalies, increase the vertical face height, and result in occlusal interferences. Class III elastics have similar effects but in opposing directions.
Orthodontists also attempt to use other anchorage devices to aid in cases with high anchorage needs, but sometimes these approaches are “sprinkled in” haphazardly or implemented once trouble is observed. Two such approaches are use of a Nance holding arch and use of a TPA. The Nance appliance, originally proposed by Hayes Nance in 1947, utilizes a stainless steel .036-inch wire bent along the contours of the maxillary arch to connect the maxillary first molars. Once contoured and soldered to the maxillary molars, cold-cured acrylic is applied to the anterior portion of the wire to establish a rest on the palatal mucosa. It is hoped that the pressure exerted by continuous space closure mechanics onto the palatal mucosa and underlying palatal bone will be sufficient to resist anchorage loss. Unfortunately, according to some reports, this and other forms of anchorage may have less anchorage value than previously thought.
The TPA has also been used as an anchorage auxiliary. Controversy exists regarding the anchorage value of the traditional TPA, with a recent report suggesting similar levels of anchorage loss with or without a passive TPA. Orthodontists who use the TPA for anchorage suggest that part of the anchorage resistance results from using an active rather than a passive TPA.
Another approach to enhancing anchorage includes the use of headgear. This can include Klöhn-type headgear in high-pull, cervical-pull, or straight-pull directions. Other treatment disciplines recommend “J hook” headgear directly to the canines or the anterior portion of the maxillary and mandibular arches. The biggest limitation of headgear is the need for patient compliance.
The introduction of TADs is likely to diminish the need for many of these approaches for anchorage preservation. However, as with other aspects of orthodontic treatment, TADs should be used rationally and with careful attention to detail in planning and optimizing the biomechanics to be used.
CONTINUOUS ARCHWIRE MECHANICS
Indications
To enhance practice flow, orthodontists often use standardized treatment approaches that incorporate continuous archwire mechanics with the same or similar sequences of wires, retraction and space consolidation, detailing, and finishing for all patients. Although these “autopilot mechanics” have the benefits of the staff understanding and anticipating the next wire size or the next treatment stage, of possibly limiting clinician and staff time, and likely enhancing efficiency and productivity in most routine cases, the advantages of this approach may not apply to many complex and dentally or periodontally compromised cases. Indeed, the complications introduced by the use of routine mechanics in these cases will likely lead to increased treatment time, decreased productivity, and compromised esthetic and or functional results. Therefore, as a general rule, standard continuous archwire mechanics can be best used in most simple nonextraction cases, cases with spacing, extraction cases in which there is likely to be minimal round-tripping of teeth, or when decompensating in surgical cases.
Table 19-1 provides a listing of specific indications for continuous archwire mechanics and serves as a guide for clinical situations where alternate biomechanical approaches such as segmented archwire and hybrid sectional mechanics can be beneficial. Depending on the practice profile, approximately 40% to 70% of patients in a given practice would likely meet the criteria for use of routine continuous archwire mechanics to deliver the force systems necessary to produce the desired outcomes.
| Continuous Archwire | Segmented Archwire | Hybrid Sectional | |
|---|---|---|---|
| Generalized spacing | +++ | ||
| Mild crowding (nonextraction) | +++ | ||
| Crowding (extraction treatment; minimal round tripping anticipated) | +++ | ||
| Decompensations desired | +++ | ||
| Moderate to severe crowding (extraction treatment; round tripping anticipated) | — | +++ | +++ |
| Differential anchorage desired | — | +++ | ++ |
| Severe canine/premolar root angulations | — | +++ * | + |
| Asymmetric cases | — | +++ | + |
| Multiple missing teeth | — | ++ | +++ |
| Compromised periodontal health | — | ++ | +++ |
| Preservation of dental compensations | — | + * | +++ |
| Desire to perform multiple stages of treatment concurrently | — | + | +++ |
* Initiate with segmented, and follow up with hybrid sectional mechanics if needed.
Although primarily indicated for relatively routine cases, continuous archwire mechanics can be beneficial even in a select number of cases that are quite complex in which none of the contraindications listed in Table 19-1 are present, as in the following case.
Deformed dentoalveolar structures and generalized spacing
Figure 19-1 shows a patient who had recently recovered from a 6-month coma during which he had oral intubation. He presented with wide dental arches, deformed dentoalveolar structures, severely proclined upper and lower incisors, overerupted maxillary molars, and generalized spacing ( Fig. 19-1, A-H ). The generalized spacing resulted from the intubation, multiple missing teeth, macroglossia, and partial tongue paralysis. Both the proclined incisors and the buccally inclined molars had compromised periodontal health.


Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


