http://evolve.elsevier.com/Haveles/pharmacology
Many drugs have the ability to affect mental activity. Some are used in the treatment of psychiatric disorders. The dental health care worker is most likely to encounter the use of these agents in dental patients for whom they have been prescribed by psychiatrists or other physicians. Because these agents are so widely prescribed and can alter a patient’s dental treatment, the dental health care worker must understand their pharmacologic effects, adverse reactions, and dental implications.
Agents used in the treatment of the major psychiatric disorders are discussed in this chapter. Those used to treat anxiety are discussed in Chapter 11. The antiepileptic drugs used as “mood stabilizers” are discussed in Chapter 16. Because the psychotherapeutic drugs are classified by therapeutic use, a brief discussion of the common psychiatric illnesses follows.
Psychiatric disorders
There are many psychiatric disorders. Psychiatric disorders can be categorized as psychoses, affective disorders or anxiety disorders (Figure 17-1).
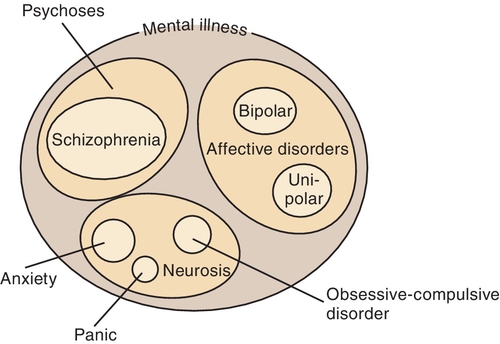
The psychoses are discussed first. Schizophrenia, the most common type of psychosis, is an extensive disturbance of the patient’s personality function with a loss of perception of reality. Schizophrenia is derived from the word meaning “splitting,” and in context it refers to the patient’s splitting from reality (not into multiple personalities). The patient’s ability to function in society is impaired because of altered thinking. The impaired thinking of patients with schizophrenia may be so detached from reality and their delusions or paranoia (e.g., someone is out to get me) so severe that their illness could lead to committing serious crimes, including assassination attempts or murders. Patients may suffer from hallucinations, delusions, or agitation. The positive symptoms of psychosis include agitation, and auditory hallucinations. Other patients may be introspective and uninvolved. The negative effects of psychosis include flat affect and apathy (Box 17-1).
The etiology of schizophrenia is not specifically known, but a familial pattern is often seen. The biochemical actions of the brain and even brain anatomy have been demonstrated to be different in some patients with schizophrenia from those in normal individuals.
Affective disorders include endogenous and exogenous depression and bipolar disorder or mania with or without depression.
Major depressive disorder, or depression, is the result of biologic, psychological, and social factors. Biologic factors consist low levels of the neurotransmitters serotonin, norepinephrine, and dopamine or a combination of the three in the brain. Psychological and social factors are related to specific external life events. Whether there are actually two types of depression separated by circumstances of occurrence is questionable. Theories for several different types of depression based on the biochemical situation in the brain have been developed, but no one has been able to demonstrate the types. Patients who exhibit alternating periods of depression and excitation (mania, elation) have bipolar (bi, two) depression, also known as manic-depressive disorder.
Anxiety Disorders are less severe than psychoses but can also be helped by drug therapy. Examples are anxiety, panic disorder, phobias, and obsessive-compulsive disorder. Psychophysiologic (somatic) disorders are those that have an emotional origin but manifest as physiologic symptoms. Personality disorders include sexual deviation, alcoholism, and drug dependence. Although many of these conditions are managed with the antidepressants and/or antipsychotics, the anxiety-related problems sometimes require the use of the benzodiazepines. Divisions of these different mental disorders have been and are continually changing to reflect either a greater knowledge or a political or “fad” perspective (What is “normal” anyway?).
This presentation is an oversimplification of the classifications of psychiatric disorders. The drug groups discussed in this chapter are antipsychotic agents, used to treat psychoses; antidepressant agents, used to treat affective disorders; and lithium, used to treat bipolar disorder. The benzodiazepines, used to treat anxiety and panic disorders, are discussed in Chapter 11.
Before the antipsychotic drugs were introduced into the management of psychiatric disorders, many physical methods were used to treat patients. Only electroconvulsive therapy (ECT, shock therapy) is still used in the treatment of depression. With the use of neuromuscular blocking agents, ECT therapy has become much safer. ECT produces the fastest results of any treatment for depression. It is reserved for patients whose disease is refractive to antidepressant therapy. Some memory loss occurs during the treatment (several sessions).
When treating patients with mental disorders, the dental hygienist should observe the following general precautions:
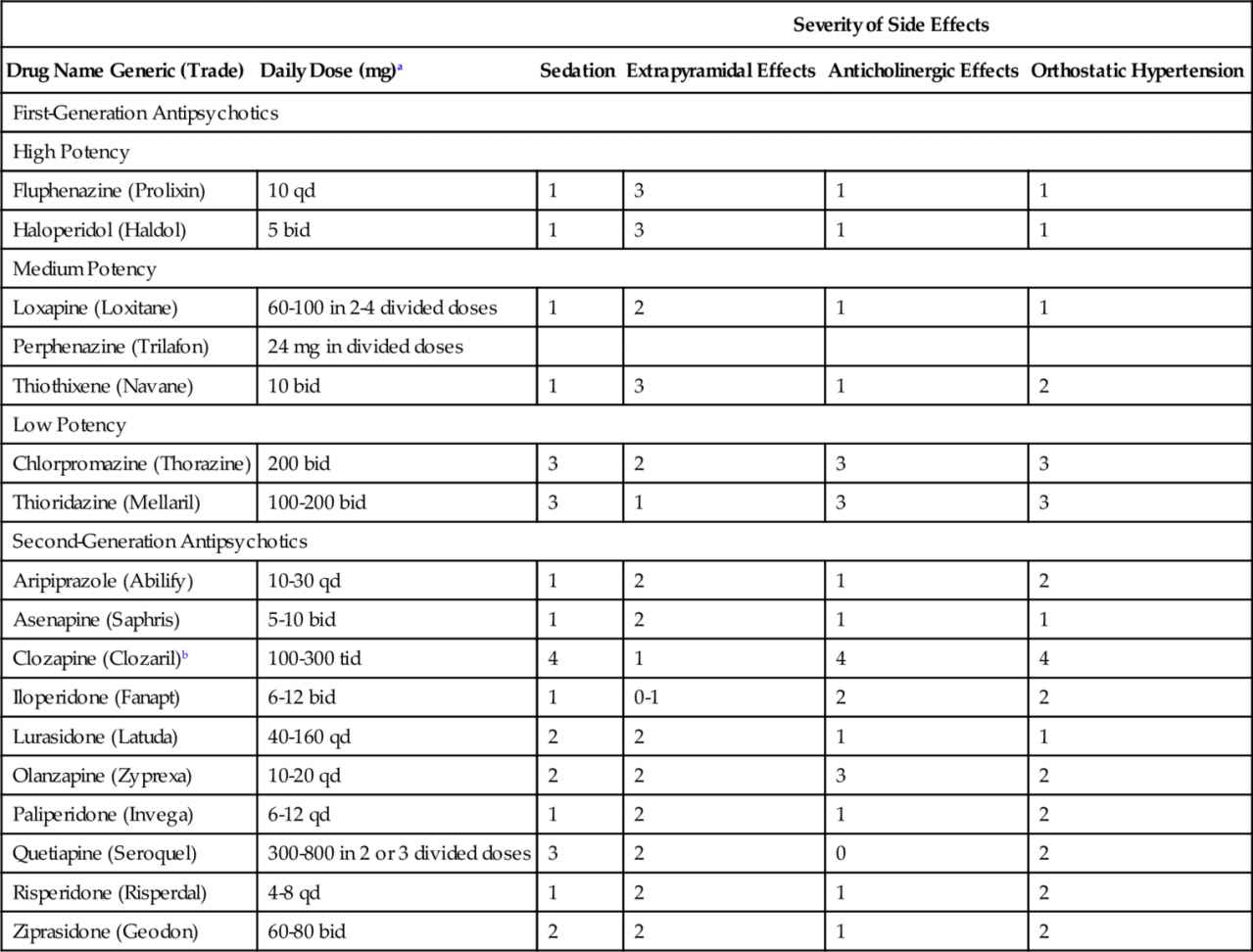
Antipsychotic agents
Antipsychotic drugs are used for the treatment of schizophrenia, schizoaffective disorder, delusional disorder, and other types of psychosis. The first generation antipsychotic drugs are more likely to treat the positive symptoms (agitation, hallucinations, delusions) than the negative symptoms (apathy, social withdrawal, blunted affect) of schizophrenia. Some symptoms may improve rapidly with antipsychotic therapy but chronic schizophrenia may take weeks to months to respond. Most patients require maintenance therapy with antipsychotics, which can help reduce the rate of relapse. Patients can be treated with either first- or second-generation antipsychotics. The second-generation antipsychotics are now used more commonly than the first-generation agents even though clinical trials have not demonstrated a clear advantage in efficacy, except for clozapine and possibly olanzapine. However, the newer agents are better tolerated. Table 17-1 lists available antipsychotic drugs, their adult usual daily dose ranges for maintenance therapy, and their adverse effect profiles.
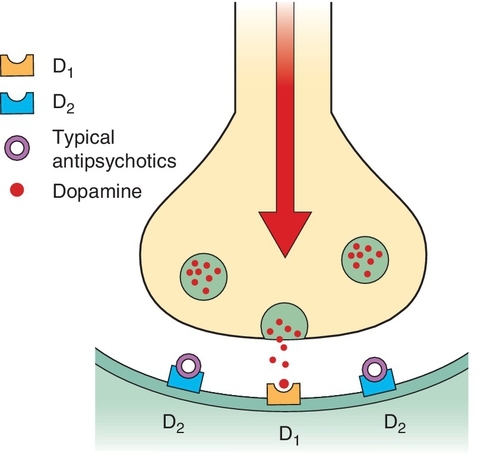
Mechanism of Action
There are several differences between the first-generation and second-generation antipsychotic agents. The first-generation antipsychotic agents were primarily dopamine antagonists (Figure 17-2). The second-generation agents have action at more than one receptor, for example, the dopamine, serotonin (5-HT), and norepinephrine (NE) receptors, improving their efficacy. The side effects of the second-generation antipsychotics are less than those of the older agents antipsychotics. Like the first-generation antipsychotics, the second-generation agents are effective against the positive effects associated with psychoses. However, unlike the first-generation antipsychotics, the second-generation antipsychotic agents are effective against the negative effects.
Pharmacologic Effects
First-Generation Antipsychotics
The pharmacologic effects of the first-generation antipsychotic agents are as follows.
Antipsychotic effect
All antipsychotics have antipsychotic effects, such as slowing of the psychomotor activity in an agitated patient and calming of emotion with suppression of hallucinations and delusions. These agents are active against the positive effects of psychosis but have little effect on the negative effects. Second-generation antipsychotics differ in that they appear to be effective against both the positive and negative symptoms of schizophrenia.
Antiemetic effect
The antiemetic effect of first-generation antipsychotics is a result of depression of the chemoreceptor trigger zone, an area in the brain that causes nausea and vomiting. These agents are useful in the symptomatic treatment of certain types of nausea and vomiting. Historically, prochlorperazine (Compazine) has been used for this effect.
Adverse reactions
Table 17-1 lists the side effects of the first generation antipsychotic agents, and Figure 17-3 demonstrates the relative side effects of several first-generation antipsychotic agents. Management of patients taking these agents involves minimizing the troubling side effects in each patient. Though first-generation antipsychotics are used less commonly than second-generation antipsychotics, the former’s adverse effects are discussed in greater detail because they can negatively affect oral health care.
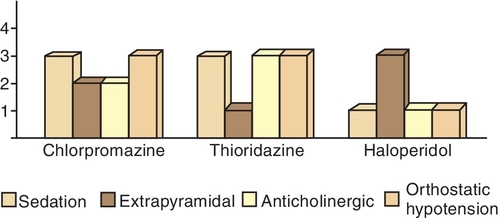
Sedation
First-generation antipsychotics differ in the degree of sedation and drowsiness they produce. The degree of sedation is one factor that determines which antipsychotic agent is prescribed. Tolerance develops to the sedative effect but not to the antipsychotic effect.
Extrapyramidal effects
The most common type of adverse reactions associated with these agents results from stimulation of the extrapyramidal system. All first-generation antipsychotics have this effect, although the incidence of the reaction varies. The following types of extrapyramidal effects can occur:
Its onset is gradual and the movements are coordinated and rhythmic. This effect is exacerbated by drug withdrawal. The involuntary movements, especially those involving the face, jaw, and tongue, can make home care difficult if not impossible. Performing oral prophylaxis is difficult because of the strength of the oral facial and tongue muscles.
The dental hygienist should discuss the patient’s side effects with his or her physician if oral prophylaxis cannot be performed. A dosage or drug change may be instituted by the patient’s psychiatrist. With the availability of the second-generation agents, extrapyramidal side effects can be greatly minimized.
The extrapyramidal side effects of first-generation antipsychotics can cause severe intermittent pain in the region of the temporomandibular joint (TMJ). This pain is produced by a spasm of the muscles of mastication. In an acute attack, it becomes difficult or impossible to open or close the jaw. Should muscle spasm be present, force should not be exerted to open the patient’s mouth for dental treatment because dislocations of the mandible can occur.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses