http://evolve.elsevier.com/Haveles/pharmacology
Allergic rhinitis
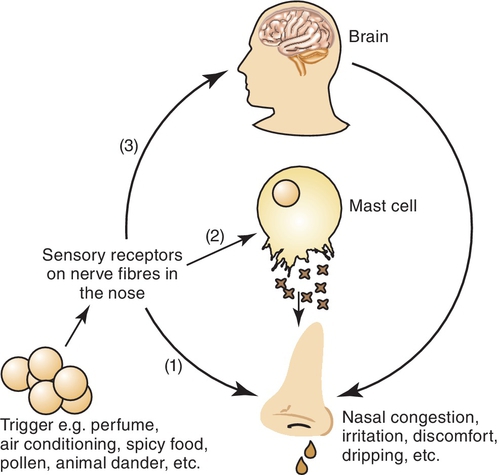
Allergic rhinitis is an inflammation of the nasal airways that occurs when an allergen is inhaled in an individual with a sensitized immune system. The allergen triggers the response of the antibody immunoglobulin E (IgE), which binds to mast cells and basophils containing histamine. The release of histamine causes itchy, watery eyes and runny nose. Symptoms vary in severity among those affected by allergies. Allergic rhinitis can be seasonal or perennial. Seasonal allergic rhinitis is usually caused by pollen from trees, grass, and flowers and lasts several weeks to months. Perennial allergic rhinitis is a result of sensitivity to different allergens, such as house dust and animal dander, and lasts throughout the year. Figure 20-1 illustrates the inflammatory process.
The most effective method of treating allergic rhinitis is to eliminate the source of allergen. If this is not possible, medication is necessary.
Antihistamines (H1-receptor antagonists)
The common term antihistamine refers to agents that are H1 antihistamines or H1-blockers. They are widely used drugs, and dental hygienists should be familiar with them for the following reasons:
Pharmacologic Effects
The first-generation H1 antihistamines, also called H1-blockers, have several pharmacologic effects, including antihistaminic, anticholinergic, antiserotonergic, and sedative effects. Second-generation H1 antihistamines penetrate poorly into the CNS and so are less likely to cause sedation. Because they have a chemical structure similar to that of histamine, they can bind with the H1-receptor and prevent or block the action of histamine (if it is released). Table 20-1 reviews the both the first- and second-generation H1-antihistamines.
Table 20-1
Selected Oral Drugs for Allergic Rhinitis
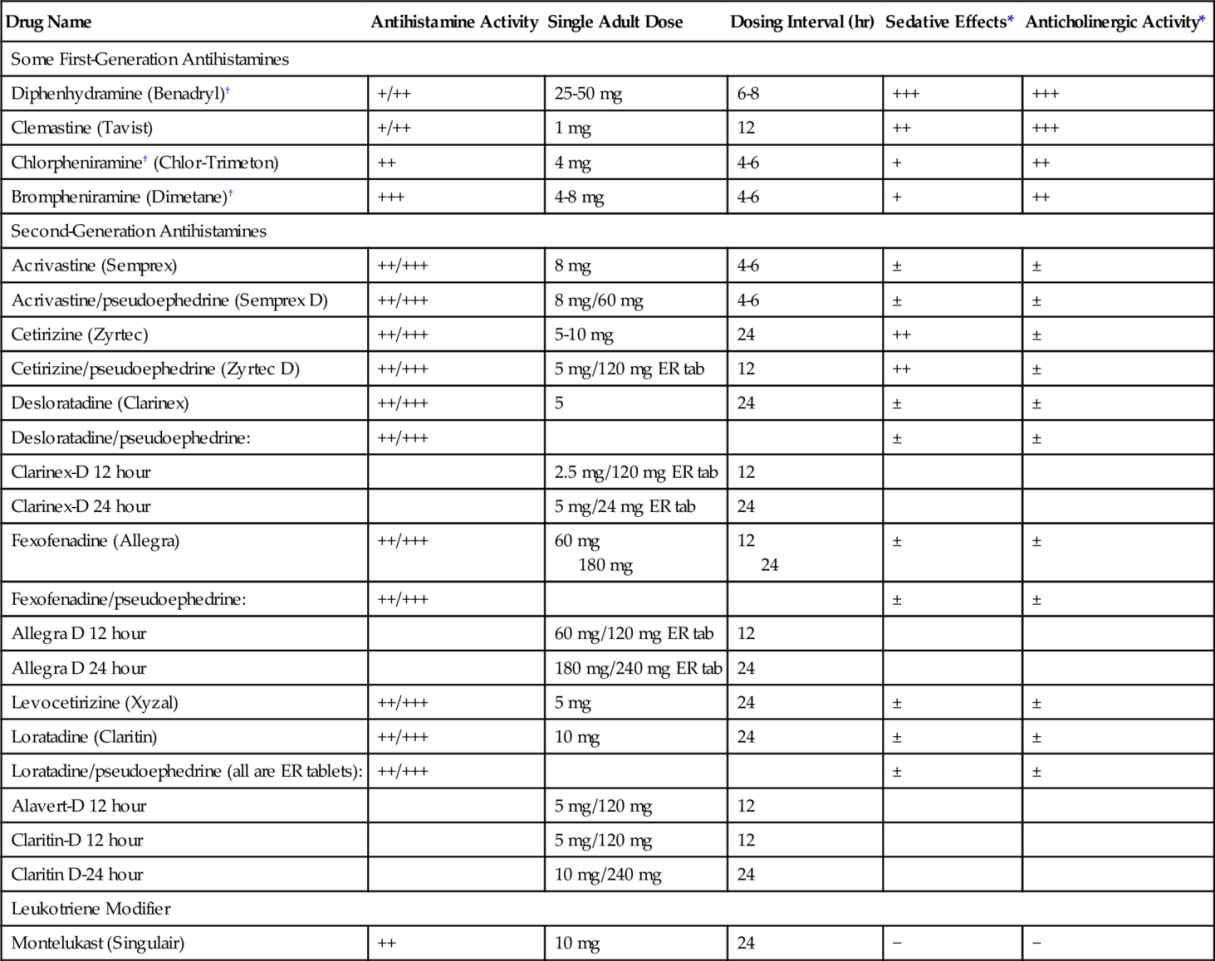
ER tab, extended-release tablet.
* ++++, Very high; +++, high; ++, moderate; +, low; ±, may have some effect; –, no effect;
† Available over the counter.
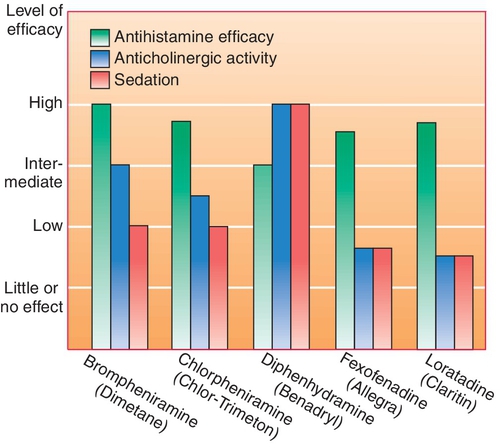
Figure 20-2 compares the relative sedative, antihistaminic, and anticholinergic effects of five common antihistamines: brompheniramine (brome-fen-EER-a meen) (Dimetane), chlorpheniramine (klor-fen-EER-a-meen) (Chlor-Trimeton), diphenhydramine (dye-fen-HYE-dra-meen) (Benadryl), fexofenadine (feks-oh-FEN-a-deen) (Allegra), and loratadine (lor-A-ti-deen) (Claritin).
The pharmacologic effects of antihistamines can be divided into those caused by blocking of histamine at the H1-receptor and those independent of this effect.
H1-Receptor Blocking Effects
Antihistamines, which are H1-antagonists, competitively block or antagonize histamine’s effect at the following sites:
Other Effects (Unrelated to H1-Blocking Effects)
Central nervous system effects
The antihistamines produce varying degrees of CNS depression.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


