http://evolve.elsevier.com/Haveles/pharmacology
Dental hygienists may become involved with drug abuse in a variety of ways. Both legal and illegal drugs can be abused. Patients seen in the dental office may be abusing drugs. Another interaction with the abusing patient involves the “potential” patient. Potential patients call the dental office, complain of pain, and request a prescription. Employees working in the dental office, including the dentist, dental hygienist, dental assistant, receptionist, and bookkeeper, may abuse drugs. Friends and relatives, as well as their friends and relatives, may abuse drugs. In our society, drug abuse, especially in adolescents, is epidemic. Wherever there are people, drug abuse can occur. Therefore the dental hygienist should become familiar with the various types of drugs commonly abused and their patterns of abuse. It is important to be able to recognize the problem in others. Because drug abuse is also a community issue, the dental hygienist should have a heightened awareness of the potential for patients to present with abuse problems (a high index of suspicion, but not one unrealistically high). The proper awareness is only learned with experience.
Alcohol and tobacco abuse cause more medical problems than all the other drugs of abuse combined. If no one in the United States used tobacco or drank alcohol, half of the filled hospital beds would be empty.
The idea of using drugs for profound effects on mood, thought, and feeling is as old as civilization. Only the kinds of substances used for this purpose have changed. Abuse has assumed a much bigger role in society because the forms of drugs used today are much stronger and have a much faster onset of action. This quick reinforcement produces abuse more quickly. For example, natives in Colombia have chewed coca leaves for many years as part of their culture, with little inappropriate use. Purifying cocaine and making it into a powder form to be “snorted” increased its abuse. When cocaine was “free based,” it became easier to abuse, but the chemical reaction was dangerous. The more recent adaptation of cocaine, making it into “rocks,” has increased abuse of the drug even more by making it available to smoke in convenient, small, reasonably priced doses. As is common with drugs of abuse, the potential for abuse is greatly increased when a drug is very potent, has a quick onset of action, is inexpensive, and is easy to distribute, making it the perfect drug of abuse.
Agents used for their psychoactive properties (capable of changing behavior or inducing psychosis-like reactions or both) can be divided into those that also have therapeutic value (opioids and sedative-hypnotics) and those that have no proven therapeutic value (psychedelics). Some agents may move from one category to the other. For example, marijuana, an agent previously considered to be worthless, is now claimed to be useful in the treatment of the nausea associated with cancer chemotherapy and for glaucoma. However, more controlled studies are needed to determine whether this claim is true.
General considerations
Abuse of a drug is defined as its use for nonmedical purposes, almost always for altering consciousness. Both legitimate and illegitimate drugs may be abused. Whether a drug has an abuse potential is determined by the drug’s pharmacologic effect. In contrast, misusing a drug means using it in the wrong dose or for a longer period than prescribed. The difference between these two uses is subtle.
Definitions
Terms relating to abuse that are used in this chapter are defined as follows:
Psychological Dependence
Psychological dependence is a state of mind in which a person believes that he or she is unable to maintain optimal performance without having taken a drug. Psychological dependence can vary in severity from mild desire (e.g., for a morning cup of coffee) to compulsive obsession (e.g., for the next dose of cocaine). Although some highly abused drugs have only psychological dependence, the “need” to use them can be as strong as or stronger than that for drugs with a physical dependence. Other examples are benzodiazepines, opioids, and amphetamines.
Physical Dependence
Physical dependence refers to the altered physiologic state that results from constantly rising drug concentrations. The presence of physical dependence is established by the withdrawal or abstinence syndrome, a combination of many drug-specific symptoms that occur upon abrupt discontinuation of drug administration. Withdrawal symptoms are often the opposite of the symptoms of use of the drug; for example, excessive parasympathetic action (e.g., diarrhea, lacrimation, and piloerection [“goose flesh”]) when withdrawing from the opioids.
Tolerance
Tolerance is characterized by the need to increase the dose continually to achieve the desired effect or the diminishing effect of taking the same dose. The type of tolerance referred to in this discussion of abuse of psychoactive drugs is central (functional or behavioral) tolerance, that is, a definite decrease in the response of brain tissue to constantly increasing amounts of a drug. (One can think of the brain becoming “stronger” [less responsive] to “withstand” the large doses it must tolerate.) In terminally ill patients, this tolerance requires ever-increasing doses of opioids even if their pain remains constant. The doses reached over time with the terminally ill would be fatal to a patient without tolerance.
Tolerance of metabolic origin (dispositional or metabolic tolerance) is caused by an accelerated rate of metabolism of the drug and is excluded in this discussion. Metabolic tolerance is an insignificant factor in the tolerance observed in humans to most of the psychoactive drugs.
Addiction, Habituation, and Dependence
Addiction and habituation are terms that have been misused almost as much as the drugs they attempt to characterize. Any use of these terms must be preceded by an adequate definition. In both addiction and habituation, the desire to continue using the drug is present, but in addiction, dependence is also present. Habituation and addiction are really only degrees of misuse or abuse of drugs. It has been recommended that these terms be replaced by the term dependence, a state of psychological or physical desire to use a drug.
Drugs that produce tolerance and physical dependence are grouped according to their ability to be substituted for one another. For example, if a person is addicted to heroin, an opioid, then other opioids, such as morphine, can prevent withdrawal. However, a barbiturate cannot be substituted for an opioid, and vice versa. Therefore the opioids and barbiturates are separate groups of dependence-producing drugs. The phenomenon of substitution to suppress withdrawal between different drugs is called cross-tolerance or cross-dependence. It is observed among members of the same drug group but not among different drug groups. Cross-tolerance may be either partial or complete and is determined more by the pharmacologic effect of the drug than by its chemical structure.
Most characteristics of drug abuse are determined by the individual drug involved, but the following generalizations can be made:
Approximately 80% of incarcerated (jailed) individuals are there because of drug abuse problems.
Many drugs have been abused extensively, and whether abuse can occur is a function of a particular drug’s effects on neurotransmitters (combined with some genetic component within the user). At various times, sniffing airplane glue, inhaling propellant, smoking banana peels, smoking peyote (contains mescaline), and ingesting morning glory seeds have been attempted. The problems and treatment of drug abuse are less related to the drugs themselves, although they can cause definite problems, than to the “inner person” of the patient involved in this type of behavior and his or her genetic predisposition. To treat abuse, a multifactorial approach is needed: counseling, education, self-help groups, and an intense desire to stop.
Propellant that is included in paint cans is preferred. The procedure is called “huffing” because the contents are sprayed into a plastic bag and fumes are repeatedly inhaled. Abuse of paint can easily produce irreversible damage to the liver and brain.
This chapter discusses the properties of the specific groups of agents abused and the differences among the groups. The abusable drugs are divided into the following groups: central nervous system (CNS) depressants (“downers”), CNS stimulants (“uppers”), and hallucinogens. Some drugs, depending on the dose, may belong to more than one group. For example, marijuana may be classified as either a CNS depressant or a hallucinogen. Table 26-1 lists the common drugs of abuse by category.
Table 26-1
Drugs of Abuse by Category
| Drug Group | Most Common Examples | Other Examples |
| Opioids | Heroin | Morphine Codeine Meperidine Hydromorphone |
| Stimulants | Cocaine Methamphetamine Bath Salts |
Amphetamines Methylphenidate Nicotine |
| Depressants (sedative-hypnotics) | Ethanol Benzodiazepines Inhalants Nitrous oxide* |
Barbiturates Nonbarbiturate sedatives |
| Hallucinogens | Lysergic acid diethylamide (LSD) | Mescaline Phencyclidine (PCP) |
| Other | Marijuana Spice K-2 |
Caffeine |
* In dentistry because of availability.
Central nervous system depressants
CNS depressants include alcohol, opioids, barbiturates, benzodiazepines, volatile solvents (glue and gasoline), and nitrous oxide (abused mainly in dentistry).
Ethyl Alcohol
Ethyl alcohol, or ethanol (ETH-an-ol), is a sedative agent used socially. Because it is legal, its availability makes it the most often abused drug. Abuse of alcohol, called alcoholism, is the number one public health problem in the United States and is associated with many major medical problems. The incidence of alcoholism in the United States is approximately 15%. Many “accidental” deaths are associated with the use of alcohol. Two-fifths of traffic fatalities involve alcohol. More than 50% of gunshot wounds in teenagers are preceded by abuse of alcohol. The best use of resources for addiction would be to deal with alcoholism as soon as it can be identified.
Pharmacokinetics
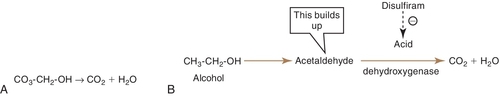
Ethyl alcohol is rapidly and completely absorbed from the gastrointestinal tract. Peak levels during fasting occur in less than 40 minutes. Food delays absorption and reduces the peak levels. Alcohol is oxidized in the liver to acetaldehyde, which is then metabolized to carbon dioxide (CO2) and water (H2O) (Figure 26-1).
Its metabolism follows zero-order kinetics, so a constant amount of alcohol is metabolized per unit of time regardless of the amount ingested. Because of zero-order kinetics, excessive intake of alcohol can have a prolonged effect. It is also excreted from the lungs (alcohol breath) and in urine.
Acute Intoxication
With mild alcohol intoxication, impairment of judgment, emotional lability, and nystagmus occur. When intoxication is moderate, dilated pupils, slurred speech, ataxia, and a staggering gait are noted. If intoxication is severe, seizures, coma, and death can occur. Treatment involves fluids and electrolytes, thiamine (vitamin B6), sodium bicarbonate, and magnesium.
Withdrawal
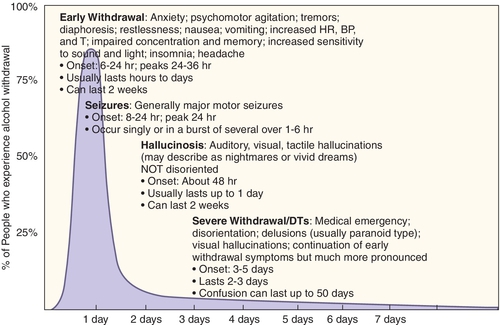
Withdrawal from alcohol use occurs after the use of alcohol. The more alcohol consumed and the more time spent consuming it, the more violent the withdrawal syndrome is (Figure 26-2). Stage 1 withdrawal usually begins 6-8 hours after drinking has stopped; and includes psychomotor agitation, and autonomic nervous system hyperactivity. Stage 2 withdrawal includes hallucinations, paranoid behavior, and amnesia. Stage 3 includes disorientation, delusions, and grand mal seizures. It takes 3-5 days after cessation of drinking alcohol for stage 3 to occur. A cross-tolerant benzodiazepine (e.g., chlordiazepoxide; see Chapter 11) may be used to prevent withdrawal symptoms. Withdrawal from alcohol is termed delirium tremens (DTs) because the patient often experiences shaky (tremor) movements. Alcohol withdrawal can be life threatening if not properly treated.
Long-Term Effects
The long-term medical effects of alcoholism can include deficiency of proteins, minerals, and water-soluble vitamins. Impotence, gastritis, esophageal varices, arrhythmias, and hypertension have been reported. If a pregnant woman is using ethanol chronically, fetal alcohol syndrome can occur (see Figure 25-4). The infant is retarded in body growth and has a small head (microencephaly), poor coordination, underdevelopment of the midface, and joint anomalies. In more severe cases, cardiac abnormalities and mental retardation are present. Chronic alcohol use increases the risk of cancer of the mouth, pharynx, larynx, esophagus, and liver, which may also occur with tobacco use, making the risk higher than with alcohol alone. The liver can be affected with alcoholic hepatitis and amnesic syndrome (Wernicke-Korsakoff syndrome), and peripheral neuropathy can occur.
Alcoholism
Alcoholism is a disease in which the alcoholic continues to drink despite the knowledge that drinking is causing a variety of problems (Box 26-1). There is a genetic link for alcoholism; children of alcoholics are at a much greater risk for becoming alcoholic. In the future, genetic testing may be able to identify at-risk children and target that population for intense educational and social intervention for prevention.
“Red flags” for alcohol abuse include drinking at an inappropriately early time, shaking when not drinking, blackouts when drinking, and being told that you drink too much. Missing work and problems in personal relationships are also strong warning signs.
Treatment
Alcoholics Anonymous
Alcoholics Anonymous, the most successful group for treating alcoholism, is a self-help organization made up of recovering alcoholics. The members (who are recovering alcoholics) give support to alcoholics who are attempting recovery. For most alcoholics, inpatient detoxification is usually not required. In fact, inpatient treatment does not give the alcoholic any experience in recovery in the “real world.” Outpatient psychiatric treatment can help provide some insight for alcoholics.
Drug treatment
Alcoholics who are motivated and socially stable can be given disulfiram (dye-SUL-fi-ram) (Antabuse). Occasionally, employers insist on the ingestion of disulfiram as a condition of employment of an alcoholic person.
Because disulfiram inhibits the metabolism of aldehyde dehydrogenase, a buildup of acetaldehyde occurs. Acetaldehyde produces significant side effects if alcohol is ingested. They include vasodilation, flushing, tachycardia, dyspnea, throbbing headache, vomiting, and thirst. The reaction may last from 30 minutes to several hours. Certain drugs that produce the disulfiram-like reaction (e.g., metronidazole) may cause a minor version of these symptoms with alcohol intake.
Naltrexone (ReVia), an oral opioid antagonist, is an old drug with a new use. Originally, it was indicated to prevent relapse in the opioid-dependent patient. Its new use is to reduce alcohol craving. Because naltrexone is partially effective in decreasing craving for alcohol, the logical conclusion is that alcohol stimulates some of the opioid receptors (among other receptors). More detailed knowledge of the receptors affected by alcohol may improve the chance of developing other agents to manage this disease. Other agents that might be useful are related to other neurotransmitters such as dopamine and serotonin.
Psychotropic agents may be helpful in managing the alcoholic patient because of the high incidence of comorbidity of psychiatric conditions.
Dental Treatment of the Alcoholic Patient
The dental hygienist must have an index of suspicion for alcoholism in patients treated in the dental office. The great majority of alcoholics look exactly like our neighbors, not like those characterized in old movies (e.g., unshaven, shaky). All health care workers have been given the charge to identify alcoholic patients and help them obtain treatment.
The dental treatment of the alcoholic patient involves some modifications, depending on the severity of the disease process. Most alcoholic patients have poor oral hygiene. Check for the sweet musty breath and painless bilateral hypertrophy of parotid glands characteristic of alcoholism. Cirrhosis of the liver can occur when alcoholics continue to abuse alcohol (Figure 26-3). The major problem in these patients is a failure of the liver to perform adequately. Because of hepatic failure, the liver is able to store less vitamin K and the conversion of vitamin K to the coagulation factors is reduced. The outcome of these effects is a deficiency in coagulation factors II, VII, IX, and X (vitamin K-dependent factors) with resulting bleeding tendencies. The patient’s international normalized ratio (INR) can be elevated to 6 or more without the presence of other concomitant medications. Thrombocytopenia secondary to portal hypertension and bone marrow depression magnifies the hemostatic deficiency, sometimes resulting in spontaneous gingival bleeding. With the presence of esophageal varices, spontaneous bleeding can occur. Later in liver failure, the abdomen becomes distended with fluid (the patient appears to be 9 months pregnant).
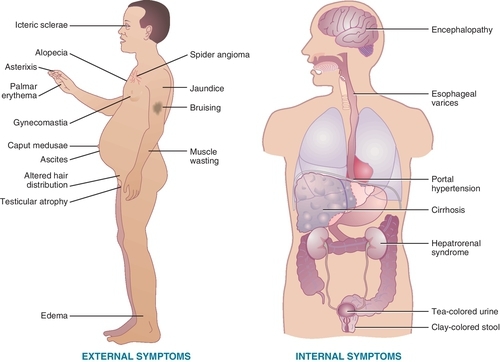
Oral complications of alcoholism include glossitis, loss of tongue papillae, angular/labial cheilosis, and Candida infection. Healing after surgery may be slow, and bleeding may be difficult to stop.
Because alcohol and tobacco use and abuse predispose a patient to oral squamous cell carcinoma, the dental hygienist should check any oral lesions carefully. Special attention should be paid to leukoplakia and ulceration (especially on the lateral border of the tongue or the floor of the mouth).
With reduced liver function, the liver has difficulty metabolizing drugs usually metabolized in the liver. The levels of drugs metabolized by the liver, such as amide local anesthetics and oxidized benzodiazepines, will not fall as rapidly as in normal patients. Dose reductions are necessary because of diminished liver function. The signs of potential advanced alcoholic liver disease are listed in Box 26-2.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


