In adult orthodontics it is extremely difficult to correct malocclusions such as incisor crowding, maxillary protrusion, anterior crossbite, and bimaxillary protrusion without extracting bicuspids. The main reason for this difficulty is that in the adult patient the second molars have already fully erupted and any distalization approach will involve the distal movement of both the first and the second molars. Headgear has been a representative “distalizer” in traditional orthodontics and is frequently used to distalize the maxillary first molars in adolescent patients. This is seldom an option for adult patients, however, because of the possible impact on esthetics and compliance.
To address these problems, various intraoral “noncompliance” appliances for maxillary molar distalization have been introduced and evaluated since the 1980s. Although it is possible to distalize the maxillary molars with these appliances, two side effects have been reported: (1) anchorage loss of the maxillary premolars and flaring of the incisors in reaction to molar distalization and (2) considerable relapse, because the distalized molars must be used as part of anchorage during retraction of the premolars and the anterior teeth. Moreover, most appliances used for molar distalization have been restricted to the maxilla; few effective noncompliance distalizers have been reported for the mandibular molars. Simultaneous distalization of the maxillary and mandibular molars in adults has been almost impossible.
SKELETAL ANCHORAGE SYSTEM
To remedy the problems of previous noncompliance appliances, the authors developed the skeletal anchorage system (SAS) consisting of titanium miniplates and monocortical screws temporarily placed in either the maxilla or the mandible (or in both) as absolute anchorage units for adult orthodontics. The SAS has been used as a multipurpose modality in combination with a multibracketed appliance, which makes it possible to move the maxillary and mandibular molars distally simultaneously. Although minor surgery for the implantation and removal of the miniplates are always necessary and infection can rarely occur (<10%), the SAS has a distinct advantage in that it enables distalization of the molars predictably in nongrowing patients. The SAS has been accepted as an effective modality for adult orthodontics and is expanding the envelope of nonextraction treatment modalities.
Recently, the authors conducted a study to verify the efficiency of the SAS. The purpose of this study was to investigate the following:
- •
Amount of distal movement of the maxillary and mandibular first molars
- •
Type of movement
- •
Difference between the predicted and actual amount of distalization
- •
Relationship between the amount of distalization and age of the patient
Three patients who underwent distalization of the maxillary and the mandibular posterior teeth at the same time utilizing SAS biomechanics are presented later in this chapter.
MATERIAL AND METHODS
Distalization of Maxillary Molars
Twenty-five nongrowing patients (22 females, 3 males) who had undergone SAS treatment for distalization of the maxillary molars were selected for the study. All the subjects met the following criteria for case selection:
- 1.
Confirmation of cessation of active mandibular growth through analysis of serial cephalograms
- 2.
Sufficient space behind the first molar for the second or third molars after distalization
- 3.
Achievable individualized treatment goals based on the cephalometric and occlusogram predictions
- 4.
Treatment executed through symmetrical distalization mechanics
The most common chief complaint of these patients was maxillary incisor crowding. Their average age at the beginning of treatment was 23 years, 11 months (range: 15 yr, 2 mo to 45 yr, 5 mo). The third molars were bilaterally extracted in 12 patients and bilaterally missing in five patients. The bilateral second molars were extracted in six patients because of anticipated difficulty in extracting the maxillary third molars. The average orthodontic treatment time using SAS was 19 months (range: 8-36 months).
Figure 24-1, A , shows the Y -type miniplates (Orthoanchor SMAP, Dentsply-Sankin, Tokyo, Japan) that were developed and used for distalization and intrusion for the maxillary posterior teeth. The plates were made of pure titanium and were suitable for osseointegration and tissue integration. In addition, they were sufficiently strong to resist the usual orthodontic forces as well as the headgear force. The miniplates could be bent with ease for fitting the bone contour of the implantation site. Figure 24-1, B , shows the head portion intraorally exposed and positioned outside the dentition so that it never disturbed the distalization of the maxillary molars. Each head portion had three continuous hooks for easier application of the orthodontic force vectors. The arm portion was transmucosal and had three graduated lengths—short (6.5 mm), medium (9.5 mm), and long (12.5 mm)—to compensate for individual morphological differences ( Fig. 24-1, A ). The body portion was positioned subperiosteally.
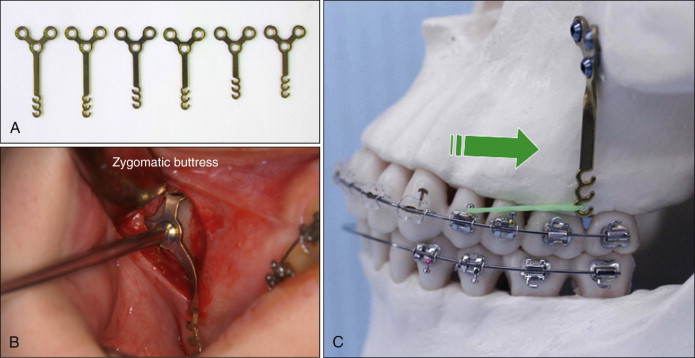
The implantation sites of the miniplates required sufficiently thick cortical bone, at least 2 to 3 mm, to enable fixation of the miniplates with monocortical miniscrews. The screws were made of pure titanium. Each screw had a head with a tapered square inside and self-tapping thread. The diameter of the screw was 2 mm, and the available length was 5 mm. The miniplates were placed at the zygomatic buttress to distalize the maxillary posterior teeth ( Fig. 24-1, B ). Although the lateral wall of the maxilla was too thin to hold the screws of the miniplates, the bone of the zygomatic buttress was thick enough.
The operation was carried out under local anesthesia by oral surgeons. First, a mucoperiosteal incision was made at the buccal vestibule of the implantation site. A mucoperiosteal flap was elevated after subperiosteal ablation, and the surface of the cortical bone at the implantation site was exposed. The miniplate was selected according to the distance between the implantation site and the dentition, as shown on the panoramic x-ray film or the cone-beam computed tomography (CBCT) scan taken before surgery. The selected plate was contoured to fit the bone surface. A pilot hole was then drilled and a self-tapping monocortical screw inserted. After placement of the remaining screws, the miniplate was then firmly attached to the bone surface. The wound was closed and sutured with absorbable thread. The surgery took 10 to 15 minutes for each miniplate.
Orthodontic force was applied approximately 3 weeks after the implantation surgery, after soft tissue healing around the miniplates. It was unnecessary to wait for osseointegration of the titanium screws and miniplates. All miniplates were removed immediately after debonding.
Most patients who underwent the miniplates placement had mild to moderate facial swelling for several days after surgery. Infection occurred occasionally during orthodontic treatment (<10% of patients). Mild infections were controlled using antiseptic mouthwash and careful brushing techniques. In more severe cases, antibiotics were required.
Figure 24-1, C , shows the representative SAS mechanics for en masse distalization of the maxillary posterior teeth. All subjects were bonded with preadjusted multibracketed appliances with .022-inch slots. Heat-treated .018 × .025–inch Elgiloy (Rocky Mountain Orthodontics, Denver, Colo.) wires were used as the main archwires. The orthodontic forces were approximately 400 to 500 gf (grams force) for en masse distalization of posterior teeth. Orthodontic forces were mostly provided by nickel-titanium (Ni-Ti) open-coil springs (Tomy International, Tokyo, Japan) or elastic chain modules (Pro-Chain, Dentsply-Sankin, Tokyo, Japan).
Lateral cephalometric radiographs with wide-open mouths were used in this study to identify the crown shapes of the maxillary first molars without being obscured by the opposing teeth ( Fig. 24-2 ). The radiographs were taken before treatment and immediately after debonding in all subjects. The cephalograms were traced, and the craniomaxillary tracings were carefully superimposed by using stable anatomical structures such as the cranium, anterior cranial base, and fine structures in the maxilla. The tracings of the left and right first molars were averaged.
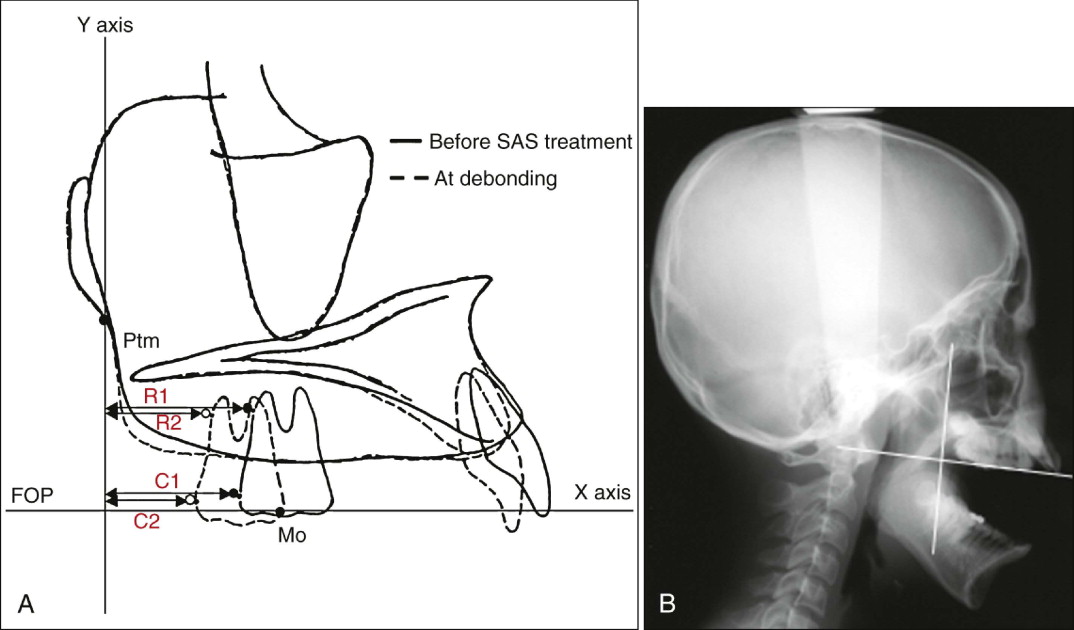
Figure 24-2, A , shows the reference planes and landmarks for determining the distal movement of the maxillary first molars. The initial maxillary occlusal plane, defined by the first molar and the maxillary central incisor, served as the x axis, and the y axis was a perpendicular line drawn from the pterygomaxillary fissure. C1 and C2 were the most distal points of the maxillary first molar crown before treatment and at debonding, respectively. Similarly, R1 and R2 were the most distal points of the maxillary first molar root before treatment and at debonding, respectively. The x axis of each landmark was measured with calipers at a precision of 0.1 mm. The amount of posterior displacement at the crown (C1-C2) and root (R1-R2) was calculated, and the type of tooth movement was evaluated by the crown/root movement ratio. The difference from the predicted amount of the crown distalization (treatment goals) was then assessed. In addition, the relationship between the amount of posterior displacement of the crown and the patients’ age (before treatment) was evaluated.
The Pearson correlation coefficient test was applied to evaluate the relationships between the amount of posterior displacement at the crown and root levels and the difference from the predicted crown movement.
Distalization of Mandibular Molars
Twenty-nine patients (24 females, 5 males) who had complained about lower anterior crowding or an anterior crossbite before orthodontic treatment were also selected for the study. The mandibular posterior teeth were symmetrically distalized with the SAS based on individualized treatment goals in all subjects. The criteria for case selection were the same as for the maxillary molars. The average age at the beginning of treatment was 23 years, 10 months (range: 15 yr, 6 mo to 46 yr, 3 mo). The mandibular third molars were bilaterally extracted in 21 patients and were bilaterally missing in eight patients before orthodontic treatment.
Figure 24-3 shows T -type miniplates that are applied in the mandible and the biomechanics for en masse distalization of mandibular posterior teeth. Generally, L -type miniplates are used by cutting off one of the circles of T -plates, which then are subperiosteally placed at the mandibular body between the first and second molars. Surgical procedures for implantation of miniplates in the mandible are almost the same as those for the maxilla.
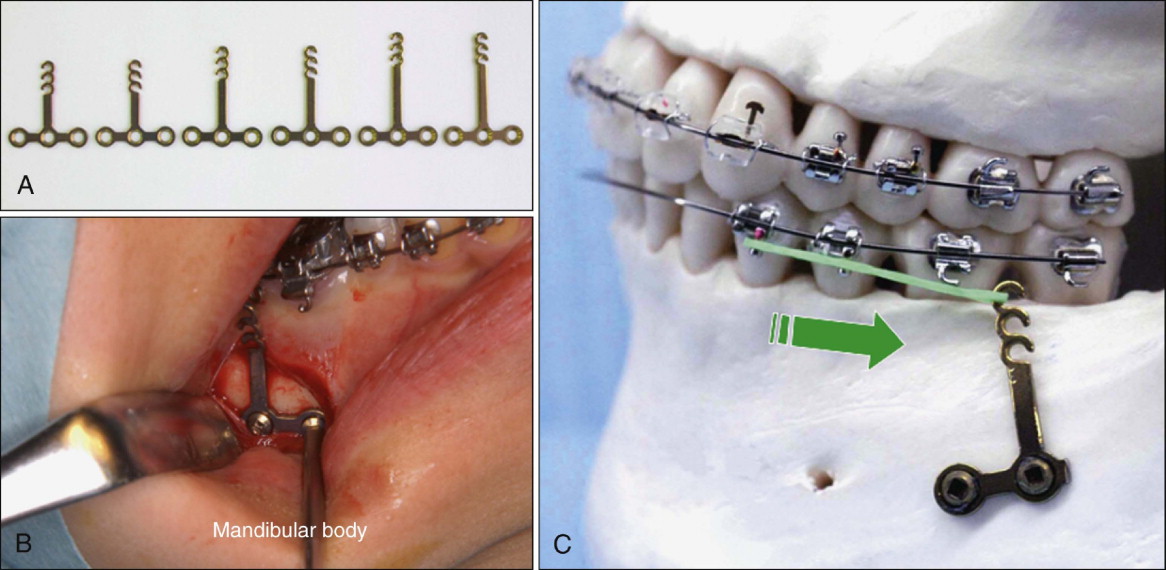
Figure 24-4 shows the reference planes and landmarks for evaluation of distalization of the mandibular first molars. The mandibular cephalometric tracings were carefully superimposed by using fine anatomical structures of the mandible. The tracings of the left and right first molars were averaged. The initial functional occlusal plane in the mandible served as the x axis. The y axis was a perpendicular line drawn from the intersection point of the anterior border of the ramus with the occlusal plane. C1 and C2 were the most distal points of the mandibular first molar crown before treatment and at debonding, respectively. Similarly, R1 and R2 were the most distal points of the mandibular first molar root before treatment and at debonding, respectively. The x axis of each landmark and the amount of posterior displacement at the crown (C1-C2) and root (R1-R2) were measured. The types of distalization of the mandibular molars were evaluated following the same methods used for the maxillary molars.
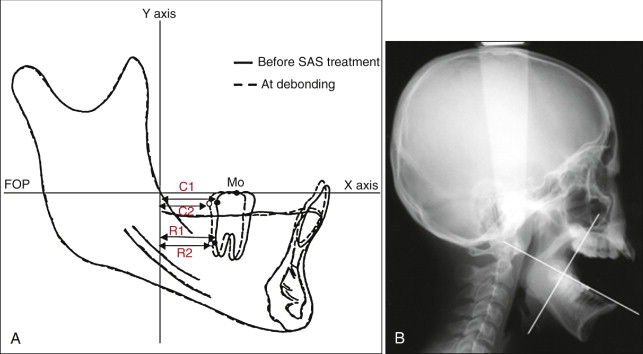
Again, the Pearson correlation coefficient test was applied to evaluate the relationships between the amount of distal movement at the crown and root levels and the difference from the predicted amount of crown movement.
MATERIAL AND METHODS
Distalization of Maxillary Molars
Twenty-five nongrowing patients (22 females, 3 males) who had undergone SAS treatment for distalization of the maxillary molars were selected for the study. All the subjects met the following criteria for case selection:
- 1.
Confirmation of cessation of active mandibular growth through analysis of serial cephalograms
- 2.
Sufficient space behind the first molar for the second or third molars after distalization
- 3.
Achievable individualized treatment goals based on the cephalometric and occlusogram predictions
- 4.
Treatment executed through symmetrical distalization mechanics
The most common chief complaint of these patients was maxillary incisor crowding. Their average age at the beginning of treatment was 23 years, 11 months (range: 15 yr, 2 mo to 45 yr, 5 mo). The third molars were bilaterally extracted in 12 patients and bilaterally missing in five patients. The bilateral second molars were extracted in six patients because of anticipated difficulty in extracting the maxillary third molars. The average orthodontic treatment time using SAS was 19 months (range: 8-36 months).
Figure 24-1, A , shows the Y -type miniplates (Orthoanchor SMAP, Dentsply-Sankin, Tokyo, Japan) that were developed and used for distalization and intrusion for the maxillary posterior teeth. The plates were made of pure titanium and were suitable for osseointegration and tissue integration. In addition, they were sufficiently strong to resist the usual orthodontic forces as well as the headgear force. The miniplates could be bent with ease for fitting the bone contour of the implantation site. Figure 24-1, B , shows the head portion intraorally exposed and positioned outside the dentition so that it never disturbed the distalization of the maxillary molars. Each head portion had three continuous hooks for easier application of the orthodontic force vectors. The arm portion was transmucosal and had three graduated lengths—short (6.5 mm), medium (9.5 mm), and long (12.5 mm)—to compensate for individual morphological differences ( Fig. 24-1, A ). The body portion was positioned subperiosteally.
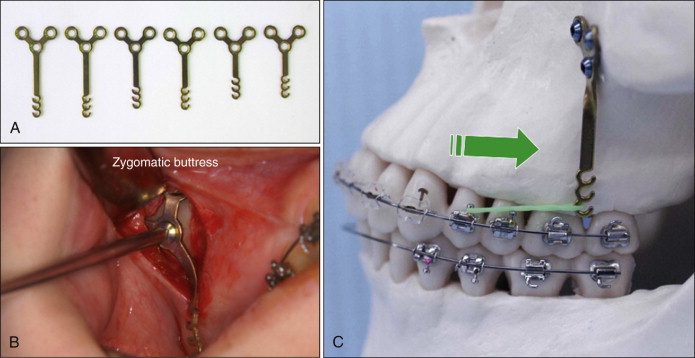
The implantation sites of the miniplates required sufficiently thick cortical bone, at least 2 to 3 mm, to enable fixation of the miniplates with monocortical miniscrews. The screws were made of pure titanium. Each screw had a head with a tapered square inside and self-tapping thread. The diameter of the screw was 2 mm, and the available length was 5 mm. The miniplates were placed at the zygomatic buttress to distalize the maxillary posterior teeth ( Fig. 24-1, B ). Although the lateral wall of the maxilla was too thin to hold the screws of the miniplates, the bone of the zygomatic buttress was thick enough.
The operation was carried out under local anesthesia by oral surgeons. First, a mucoperiosteal incision was made at the buccal vestibule of the implantation site. A mucoperiosteal flap was elevated after subperiosteal ablation, and the surface of the cortical bone at the implantation site was exposed. The miniplate was selected according to the distance between the implantation site and the dentition, as shown on the panoramic x-ray film or the cone-beam computed tomography (CBCT) scan taken before surgery. The selected plate was contoured to fit the bone surface. A pilot hole was then drilled and a self-tapping monocortical screw inserted. After placement of the remaining screws, the miniplate was then firmly attached to the bone surface. The wound was closed and sutured with absorbable thread. The surgery took 10 to 15 minutes for each miniplate.
Orthodontic force was applied approximately 3 weeks after the implantation surgery, after soft tissue healing around the miniplates. It was unnecessary to wait for osseointegration of the titanium screws and miniplates. All miniplates were removed immediately after debonding.
Most patients who underwent the miniplates placement had mild to moderate facial swelling for several days after surgery. Infection occurred occasionally during orthodontic treatment (<10% of patients). Mild infections were controlled using antiseptic mouthwash and careful brushing techniques. In more severe cases, antibiotics were required.
Figure 24-1, C , shows the representative SAS mechanics for en masse distalization of the maxillary posterior teeth. All subjects were bonded with preadjusted multibracketed appliances with .022-inch slots. Heat-treated .018 × .025–inch Elgiloy (Rocky Mountain Orthodontics, Denver, Colo.) wires were used as the main archwires. The orthodontic forces were approximately 400 to 500 gf (grams force) for en masse distalization of posterior teeth. Orthodontic forces were mostly provided by nickel-titanium (Ni-Ti) open-coil springs (Tomy International, Tokyo, Japan) or elastic chain modules (Pro-Chain, Dentsply-Sankin, Tokyo, Japan).
Lateral cephalometric radiographs with wide-open mouths were used in this study to identify the crown shapes of the maxillary first molars without being obscured by the opposing teeth ( Fig. 24-2 ). The radiographs were taken before treatment and immediately after debonding in all subjects. The cephalograms were traced, and the craniomaxillary tracings were carefully superimposed by using stable anatomical structures such as the cranium, anterior cranial base, and fine structures in the maxilla. The tracings of the left and right first molars were averaged.
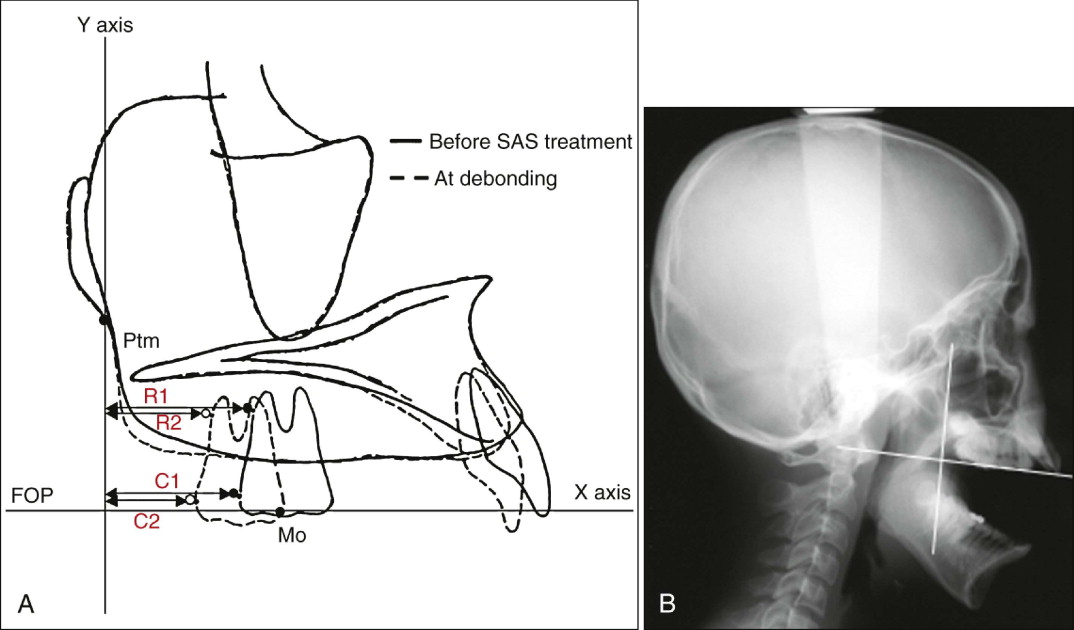
Figure 24-2, A , shows the reference planes and landmarks for determining the distal movement of the maxillary first molars. The initial maxillary occlusal plane, defined by the first molar and the maxillary central incisor, served as the x axis, and the y axis was a perpendicular line drawn from the pterygomaxillary fissure. C1 and C2 were the most distal points of the maxillary first molar crown before treatment and at debonding, respectively. Similarly, R1 and R2 were the most distal points of the maxillary first molar root before treatment and at debonding, respectively. The x axis of each landmark was measured with calipers at a precision of 0.1 mm. The amount of posterior displacement at the crown (C1-C2) and root (R1-R2) was calculated, and the type of tooth movement was evaluated by the crown/root movement ratio. The difference from the predicted amount of the crown distalization (treatment goals) was then assessed. In addition, the relationship between the amount of posterior displacement of the crown and the patients’ age (before treatment) was evaluated.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


